New CBHI Materials
A note from Secretary Judy Ann Bigby (EOHHS)
This important information is for families and care givers.
see more...
|
Implementing the Rosie D. Remedy: Important Information for
School & Agency Staff
The information below is taken directly from a document entitled Implementing the Rosie D. Remedy: The Opportunities and Challenges of Restructuring a System of Care for Children’s Mental Health in Massachusetts. This document, written by Holly A. Kenny for the Massachusetts Medicaid Policy Institute, contains important information that all school and agency staff should become familiar with. The full report is available at http://www.massmedicaid.org (go to Reports under “MMPI Publications”).
In July of 2007 a district court ruling found that Massachusetts’ children with serious emotional disturbance (SED) were not receiving appropriate mental health screenings, service coordination, and home-based treatment services. This decision entitles children to extensive home and community-based services and calls for the creation of a new mental health infrastructure.
Among the court-ordered remedies were the following:
- Primary care providers and pediatricians must provide Early and Periodic Screening,
Diagnosis, and Treatment to eligible children.
- Clinicians will rely on clinical assessments and the Child and Adolescent Needs and
Strengths (CANS) survey to make an SED assessment and diagnosis.
- The child’s care manager and care planning team (including the child, family members, and other relevant support people – e.g. caseworkers, school staff – will develop a treatment plan.
- The development of intensive home and community-based services will allow children to return to their homes more quickly from restrictive treatment settings and will allow more children to receive treatment in their homes, schools, and communities.
- The state will augment certain existing services (e.g. mobile crisis intervention and stabilization services) and will create new services to children with SED such as In-Home Behavioral and Therapy Services and Mentor Services.
- MassHealth, in collaboration with the Department of Mental Health, will establish a statewide service delivery network, using community service agencies to coordinate home-based care.
Among the benefits that will result from the implementation of this remedy are (1) early identification of children with SED which may result in more successful and, possibly, less expensive treatments, (2) an integrated system across multiple child-serving agencies will result in a single point of entry, significantly improving access for children, and (3) children with SED will receive care in less restrictive settings that are more conducive to treatment and familiar and comfortable to them (e.g. their homes, schools, and child-care centers).
Although the brunt of the responsibility for implementing Rosie D. will fall upon MassHealth, interagency collaboration will be a critical component of the Rosie D. remedy. Implementation of the Rosie D. remedy began on December 31, 2007.
<><><><><><><><><><><><><>

|
|
THE COMMONWEALTH OF MASSACHUSETTS
EXECUTIVE DEPARTMENT
STATE HOUSE BOSTON, MA 02133
(617) 725-4000
DEVAL L. PATRICK GOVERNOR
TIMOTHY P. MURRAY LIEUTENANT GOVERNOR
June 9, 2008
Dear School Leaders:
The Executive Office of Education and the Department of Elementary and Secondary Education are partnering with MassHealth to spread the word about well-child and behavioral health services available through MassHealth and to set the stage for future conversations and collaborations regarding implementation of the remedy in Rosie D. v Romney.
MassHealth pays for “well-child” visits (except for members with MassHealth Limited) for children and young adults under the age of 21. MassHealth also covers behavioral health (mental health and substance abuse) services for children and young adults under the age of 21. The first phase of the remedy, implemented in December 2007, improves the process of screening children for behavioral health issues, as part of their primary care well-child visits. Subsequent phases of the remedy will enhance standardized assessments provided by behavioral health providers, and will cover several new behavioral health services for MassHealth Standard and MassHealth CommonHealth members under the age of 21.
Below, we have included links to fact sheets about MassHealth services in three languages.
The fact sheet includes:
- Information about the importance of well-child visits covered by MassHealth, and about how to find a primary-care doctor or nurse to provide well-child visits for children with MassHealth coverage;
- A description of a new requirement that primary care providers must offer to conduct behavioral health screenings using standardized screenings tools during well-child visits;
- Information about follow-up assessment for behavioral health issues after well-child visits;
- Behavioral health services available now for MassHealth members under 21, and behavioral health services that will be available in the future to members under the age of 21 who have MassHealth Standard or MassHealth CommonHealth;
- Information about how to apply for MassHealth; and
- Contact information for families who are enrolled in MassHealth to get more information.
Fact Sheet Links…
English Fact Sheet: http://www.mass.gov/Eeohhs2/docs/masshealth/provlibrary/epsdt-cbh-fs2.pdf
Spanish Fact Sheet: http://www.mass.gov/Eeohhs2/docs/masshealth/provlibrary/epsdt-cbh-fs2-sp.pdf
Portuguese Fact Sheet: http://www.mass.gov/Eeohhs2/docs/masshealth/provlibrary/epsdt-cbh-fs2-b-por.pdf
What You Can Do Now…
- Familiarize yourself with the information in the fact sheet;
- Share this information with your colleagues and the families with whom you work.
- Over the next several months, particularly at the start of the new school year, please watch for additional information about the Rosie D. remedies and how we will all be working together to ensure the best possible care and services for children and youth.
On behalf of MassHealth, the Executive Office of Education and ESE, we thank you for your assistance and look forward to working with you.
Sincerely,
JudyAnn Bigby
Secretary of Health and Human Services
Paul Reville
Secretary Designate of Education
|

Children’s Behavioral Health Initiative
An Overview of Rosie D. v. Romney Remedy and Implementation Plans:
Implications for Elementary and Secondary Education
+++
Overview
- The Case
- The Remedy
- Implications for Elementary and Secondary Education
- Eligible Children
- Children’s Behavioral Health Initiative
- Core Service: Intensive Care Coordination
- Project Governance and Next Steps
+++
Rosie D. v. Romney
A class action lawsuit filed in 2001 on behalf of children and youth with serious emotional disturbance, alleging MassHealth’s (the Massachusetts Medicaid program) failure to meet the obligations of the “Early Periodic Screening Diagnosis and Treatment” (EPSDT) provisions of federal Medicaid law in its services to this class of children.
- 2005: The case goes to trial
- January 2006: U.S. District Court Rules that the Commonwealth has violated the EPSDT and “reasonable promptness” provisions of Medicaid law
- Specifically, the Court finds that the Commonwealth has not provided sufficient:
- BEHAVIORAL HEALTH SCREENINGS
- ASSESSMENTS
- SERVICE COORDINATION
- HOME-BASED BEHAVIORAL SUPPORT SERVICES
- Court’s final Order issued July 16, 2007
+++
The Remedial Order Requires:
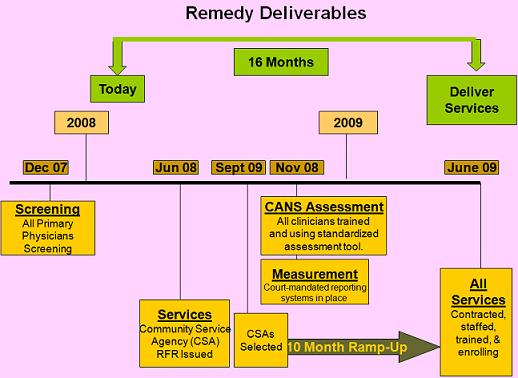
1. Standardized Behavioral Health Screening: 12/31/07
MassHealth must:
- Require primary care providers to offer all children and youth up to age 21 a standardized behavioral health screen at every “well-child” visit
- Select a menu of standardized screening tools
- Train providers in the use of the tools
- Educate providers, members and the public about the new requirements
- Report to the Court on screens delivered and screens indicating a behavioral health need
- If needed, take measures to improve the rate of screen
2. Educate Members, Providers, Public: 12/31/08
MassHealth:
- Must educate members, providers and the general public about the remedy services and how to obtain them
- Will implement the educational campaign in phases, timed to each phase of remedy implementation
3. Implement Standardized Clinical Assessment: 11/30/08
- MassHealth must ensure that all children and youth eligible for EPSDT up to age 21 receiving BH services are assessed using a standard assessment tool, Child and Adolescent Needs and Strengths (CANS)
- CANS will be used to help determine medical necessity and to develop service plans
- MassHealth must report to Court on the number of assessments performed and number of children identified with serious emotional disturbance
- Court-Ordered Reporting In Place by 11/30/08
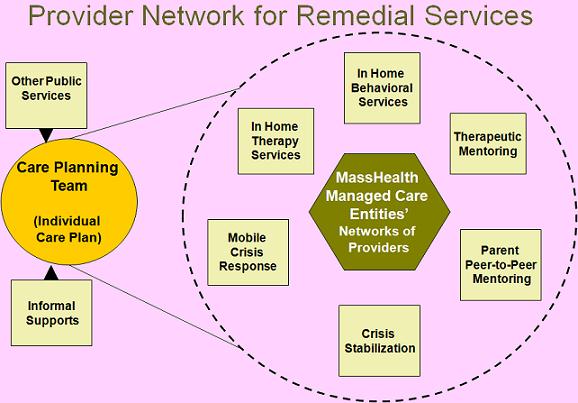
- New Services to be available state-wide by 6/30/09:
- Intensive Care Coordination (ICC) - “Wraparound” model of service planning and delivery
- Mobile crisis response
- Crisis stabilization services
- In-home behavioral services
- In-home therapy services
- Mentor services: Therapeutic Mentors for children and youth and Peer to Peer Family Mentors
+++
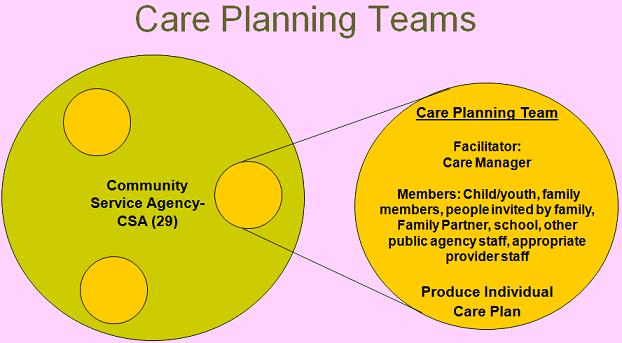
The Remedial Order Requires Inter-Agency Care Coordination
- EOHHS must:
- Ensure that representatives of involved EOHHS agencies participate in child’s care planning team
- Establish interagency protocols to coordinate agency-specific planning processes with the ICC care planning process
- Establish a conflict-resolution process for resolving differences among members of care planning teams
+++
Potential Implications of Remedy Services for Schools:
- Screening
- A “normal” place to refer parents for BH screening: their child’s pediatrician
- Earlier identification of mental health needs
- Assessment
- More standard, comprehensive assessments
- Earlier identification of mental health needs
- A common assessment framework across providers and state agencies (MassHealth, DSS, DMH
- Services
- Improved crisis response services, available to children wherever they are
- Greatly expanded access to ongoing community-based services for children on MassHealth – designed to support children and youth with chronic needs
- Remedy services may:
- Identify children with mental health needs earlier, preventing SPED referrals
- Identify children with mental health needs earlier, increasing SPED referrals
- Support schools by providing more effective crisis response services
- Support schools by providing needed services and supports to students and their families
- Keep students with significant MH needs in community schools rather than residential schools
- Require staff involvement in Intensive Care Coordination
+++
Who will be eligible for services?
- The Order requires MassHealth to provide remedy services to any child or youth:
- eligible for EPSDT (MassHealth Standard and Commonhealth members ages 0 - 21)
- who meets either the SAMHSA or IDEA definitions of “emotional disturbance”
- for whom the service is “medically necessary”
- However, MassHealth, according to its understanding of EPSDT, will provide remedy services to any EPSDT-eligible child who has a medical need for the service
- The exception is ICC, which, as a “Targeted Case Management” service, may be limited to a defined group – in this case, children who meet the SAMHSA or IDEA definitions
- Form for recording clinician’s assessment of whether a child meets either definition was developed in conjunction with DESE and notes that this assessment IS NOT a determination of eligibility for special education services
+++
SAMHSA Definitions of “SED”
Child from birth to age 18 who currently or at any time during the past year, has had a diagnosable mental, behavioral, or emotional disorder of sufficient duration to meet diagnostic criteria specified within DSM-III-R, that resulted in functional impairment which substantially interferes with or limits the child’s role or functioning in family, school, or community activities.
+++
IDEA definitions of “SED”
- Emotional disturbance means a condition exhibiting one or more of the following characteristics over a long period of time and to a marked degree that adversely affects a child’s educational performance:
- An inability to learn that cannot be explained by intellectual, sensory, or health factors
- An inability to build or maintain satisfactory interpersonal relationships with peers and teachers
- Inappropriate types of behavior or feelings under normal circumstances
- A tendency to develop physical symptoms or fears associated with personal or school problems
+++
+++
Intensive Care Coordination Model: Wraparound Service Planning
“Wraparound is a definable planning process that results in a unique set of community services and natural supports that are individualized for a child and family to achieve a positive set of outcomes.”
Burchard, J.D., Bruns, E.J., & Burchard, S.N. (2002). The Wraparound Process. In B.J. Burns and K. Hoagwood, Community-based Treatment for Youth. Oxford: Oxford University Press.
+++
What is Wraparound?
- Structured team-based process
- Plans & implements individualized care plans for children & families
- Based on an ecological understanding of the child and family
- Strong emphasis on cultural competence
- Especially appropriate for children and families with most complex and severe needs
+++
+++
+++
“Why we think wraparound is important”*
- Wraparound was a response to overly professionalized and restrictive services
- Research has found poor outcomes for treatments (including “evidence-based practices”) delivered in “real world” settings
- Why?
- Families don’t think treatments they get are relevant
- Lack of “fit” between family needs and actual services/supports received
- Lack of full engagement of families
- Programs and systems are not engineered to support flexible, individualized care
* The National Wraparound Initiative: Jane Adams, Eric Bruns, Trina Osher, Janet Walker, Jim Rast, Nancy Koroloff, Pat Miles, John VanDenBerg, and the National Wraparound Initiative advisory group. 11th Annual Building on Family Strengths Conference, Portland, Oregon, May 7, 2004
+++
Plan for Delivering Intensive Care Coordination (ICC)
- 29 Community Service Agencies (CSAs) will be designated ICC providers
- Selected by MA Behavioral Health Partnership through RFR released in June ’08
- All MassHealth insurers will contract with the same network of providers
Core Functions:
- Deliver ICC services
- Convene and staff the local System of Care Committee
+++
Children’s Behaviorial Health Initiative Mission
To strengthen, expand and integrate Massachusetts services into a comprehensive system of community-based, culturally competent behavioral health and complementary services for all children with serious emotional disturbance and other emotional and behavioral health needs, along with their families.
+++
Children’s Behavioral Health Initiative Beyond Remedy Services
- Support the creation of a System of Care
- Workforce Development Strategies
- Strengthen Cultural Competence
- Training to Fidelity & Best Practice
- Measure Client & System-level Outcomes
- Long-term Cultivation of Evidence-Based Practice
+++
Identifying next steps for Education & CBHI partnership:
- Communication Needs:
- WHO: Prioritizing constituencies
- WHAT: Stages: basic information now, operational protocols later
- WHERE: Venues, sponsors
- WHEN: Coordinate for optimal timing
- Program Planning:
- Development of proposed operational protocols
- Developing collaboration strategies
|
|
|

