"Paxil 10mg generic, medicine 6mp medication."By: Noreen A Hynes, M.D., M.P.H. - Director, Geographic Medicine Center of the Division of Infectious Diseases
- Associate Professor of Medicine
 https://www.hopkinsmedicine.org/profiles/results/directory/profile/0010761/noreen-hynes
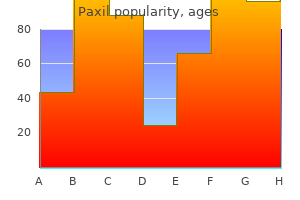
Order paxil 30mg lineAtony is often associated with uterine overdistention (multiple gestation and polyhydramnios). The anesthesiologist could additionally be consulted to help in venous access or fluid and blood resuscitation, in addition to to present anesthesia for careful examination of the vagina, cervix, and uterus. Perineal lacerations can often be repaired with native anesthetic infiltration or pudendal nerve blocks. Residual anesthesia from prior epidural or spinal anesthesia facilitates examination of the patient; however, supplementation with an opioid, nitrous oxide, or each may be required. Induction of spinal or epidural anesthesia ought to be averted in the presence of marked hypovolemia. General anesthesia is normally required for manual extraction of a retained placenta, reversion of an inverted uterus, or repair of a major laceration. Three parameters are evaluated: baseline coronary heart price, baseline variability, and the connection to uterine contractions (deceleration patterns). Baseline Heart Rate the mature fetus usually has a baseline heart fee of 110 to a hundred and sixty beats/min. An elevated baseline coronary heart rate could additionally be as a end result of prematurity, delicate fetal hypoxia, chorioamnionitis, maternal fever, maternally administered medication (anticholinergics or -agonists), or, rarely, hyperthyroidism. A decreased baseline coronary heart rate may be as a result of a postterm pregnancy, fetal coronary heart block, or fetal asphyxia. By 32 weeks, fetuses show periodic increases in baseline coronary heart price that are associated with fetal movements. Normal fetuses have 15 to forty accelerations/h, and the mechanism is believed to contain increases in catecholamine secretion with decreases in vagal tone. Accelerations diminish with fetal sleep, some medication (opioids, magnesium, and atropine), in addition to fetal hypoxia. Accelerations to fetal scalp or vibroacoustic stimulation are thought-about a reassuring signal of fetal well-being. The absence of each baseline variability and accelerations is nonreassuring and could also be an necessary sign of fetal compromise. Early decelerations are typically not associated with fetal misery and happen during descent of the top. Late decelerations may be delicate (as few as 5 beats/min) and are thought to symbolize the impression of decreased arterial oxygen tension on atrial chemoreceptors. Late decelerations with regular variability could additionally be noticed following acute insults (maternal hypotension or hypoxemia) and are normally reversible with treatment. Late decelerations with decreased variability are associated with prolonged asphyxia and may be a sign for fetal scalp sampling (see section on Other Monitoring). Complete abolition of variability on this setting is an ominous signal signifying extreme decompensation and the necessity for quick delivery. These decelerations are variable in onset, period, and magnitude (often >30 beats/min). Baseline Variability the wholesome mature fetus usually displays a baseline beat-to-beat (R-wave to R-wave) variability that can be categorized as minimal (<5 beats/min), reasonable (6�25 beats/min), or marked (>25 beats/min). Baseline variability, which is finest assessed with scalp electrodes, has become an important sign of fetal well-being and represents a normally functioning autonomic system. A sinusoidal pattern that resembles a clean sine wave is associated with fetal despair (hypoxia, drugs, and anemia secondary to Rh isoimmunization). Variable decelerations are typically associated with fetal asphyxia when fetal heart rate declines to less than 60 beats/min, fetal bradycardia lasts more than 60 s, or recurrent bradycardia happens in a sample that persists for greater than 30 min. Clinical expertise is limited with all of those modalities besides fetal scalp pH measurements. Unfortunately, fetal scalp pH measurement is associated with a small however vital incidence of false negatives and false positives. Fetal blood could be obtained and analyzed through a small scalp puncture as soon as the membranes are ruptured. Because of wide overlap, fetal blood sampling could be interpreted appropriately solely along side heart rate monitoring. Treatment of the Fetus Treatment of intrauterine fetal asphyxia is aimed at stopping fetal demise or permanent neurological damage. All interventions are directed at restoring an sufficient uteroplacental circulation. Aortocaval compression, maternal hypoxemia or hypotension, or excessive uterine exercise (during oxytocin infusions) must be corrected. Changes in maternal place, supplemental oxygen, and intravenous ephedrine or fluid, or adjustments in an oxytocin infusion usually right the problem. Failure to relieve fetal stress, as well as progressive fetal acidosis and asphyxia, necessitate quick supply. If the neonate is obviously depressed, the cord is clamped early and resuscitation is initiated immediately. Respirations should be 30 to 60 breaths/min and the guts fee one hundred twenty to one hundred sixty beats/min. Respirations are assessed by auscultation of the chest, whereas coronary heart price is decided by palpation of the heart beat at the base of the umbilical twine or auscultation of the precordium. In addition to respirations and heart rate, colour, tone, and reflex irritability should be evaluated. The Apgar score (Table 41�7), recorded at 1 min and again at 5 min after supply, stays essentially the most useful evaluation of the neonate. The 1-min score correlates with survival, whereas the 5-min rating has limited relationship to neurological end result. Neonates with Apgar scores of eight to 10 are vigorous and should require solely mild stimulation (flicking the foot, rubbing the again, and additional drying). A catheter ought to first be gently handed via each nostril to rule out choanal atresia, and then via the mouth to suction the stomach and rule out esophageal atresia. Meconium-Stained Neonates the presence or absence of meconium in the amniotic fluid (approximately 10% to 12% of deliveries) modifications the immediate management of the neonate at delivery. Fetal misery, particularly after forty two weeks of gestation, is often related to release of thick meconium into the amniotic fluid. Fetal gasping during stress results in entry of a large amount of meconium-containing amniotic fluid into the lungs. When the neonate initiates respiration at start, the meconium strikes from the trachea and large airways down towards the periphery of the lung. Thick or particulate meconium might impede small airways and trigger extreme respiratory distress in 15% of meconium-stained neonates. As the head is delivered, the nostril, mouth, and pharynx are suctioned with a bulb syringe. After the rest of the physique is delivered, the pores and skin is dried with a sterile towel.
Buy discount paxil 10mg on lineThe energy output must be saved at the minimally efficient level to forestall myocardial harm. In the primary place, one electrode is positioned on the proper second intercostal space next to the sternum and the opposite is placed on the left fifth intercostal house in the midclavicular line. When pads are used for the anteroposterior method, one is placed anteriorly over the ventricular apex in the fifth intercostal space and the opposite beneath the affected person within the left infrascapular region. For supraventricular tachycardias, with the notable exception of atrial fibrillation, vitality levels of 25 to 50 J can efficiently reestablish normal sinus rhythm. Synchronized shocks should be used for all tachyarrhythmias besides ventricular fibrillation. All medical personnel ought to stand away from the patient and the bed in the course of the shock. Atrial fibrillation usually requires a minimal of 50 to 100 J, and larger power levels are sometimes used. Hemodynamically secure ventricular tachycardia can typically be terminated with 25 to 50 J, however ventricular fibrillation and unstable ventricular tachycardia require 200 to 360 J. Regardless of the arrhythmia, a higher power degree is necessary when the primary shock is ineffective. Elective cardioversion could be performed in any setting during which full provisions for cardiopulmonary resuscitation, together with cardiac pacing capabilities, are immediately out there. The patient must be fasted, evaluated, and treated as if he had been receiving a general anesthetic within the working room. Preoperative laboratory values must be within normal limits because metabolic disorders, notably electrolyte and acid�base abnormalities, might contribute to the arrhythmia. An antiarrhythmic agent is usually began in sufferers with atrial fibrillation 1 to 2 days prior to the process to assist preserve normal sinus rhythm. Patients with atrial fibrillation of longer than a few hours period probably may have been anticoagulated for a adequate time previous to cardioversion to scale back the likelihood of a left atrial thrombus. Maintaining steady verbal contact with the patient could the most effective technique for assessing whether or not a adequate amnestic dose of (usually) propofol has been given. An anesthetic drug equipment that features at least one sedative-hypnotic in addition to succinylcholine. A cart that includes all necessary medication and equipment for cardiopulmonary resuscitation (see Chapter 55). American Society of Extracorporeal Technology Standards and Guidelines for Perfusion Practice (11/08/2013). Following preoxygenation with 60% to 100% oxygen for 3 to 5 min, the sedative-hypnotic is given in small increments) every 30 to 60 s while maintaining verbal contact with the affected person. The shock is delivered when the patient is now not in a place to reply verbally; some clinicians use lack of the eyelid reflex as an end point. Transient airway obstruction or apnea could also be observed, particularly if a couple of shock is critical. Complications include transient myocardial despair, postshock arrhythmias, and arterial embolism. Arrhythmias are often because of inadequate synchronization, however even a correctly timed cardioversion can occasionally end in ventricular fibrillation. Although recovery of consciousness is usually very rapid, sufferers must be treated like others receiving general anesthesia (see Chapter 56). Recovery additionally particularly contains monitoring for each recurrence of the arrhythmia and signs of cerebral embolism. The Society of Thoracic Surgeons, the Society of Cardiovascular Anesthesiologists, and the American Society of ExtraCorporeal Technology: Clinical Practice Guidelines for Cardiopulmonary Bypass- Temperature administration throughout cardiopulmonary bypass. Lumbar cerebrospinal fluid drainage for thoracoabdominal aortic surgery: Rationale and sensible considerations for administration. Current outcomes of off-pump versus on-pump coronary artery bypass grafting: Evidence from randomized managed trials. Current randomized management trials, observational studies and meta evaluation in off-pump coronary surgical procedure. Anesthetic pharmacology and perioperative concerns for heart transplantation. The proper mainstem bronchus lies in a more linear association with the trachea, whereas the left mainstem bronchus lies in a more angular orientation with the trachea. At this volume, the inward elastic recoil of the lung approximates the outward elastic recoil of the chest (including resting diaphragmatic tone). This enhance might be responsible for the normal agerelated decline in arterial O2 rigidity. Local factors are extra important than the autonomic system in influencing pulmonary vascular tone. The overall effect of shunting is to decrease (dilute) arterial O2 content material; this type of shunt is referred to as right-to-left. The generally used inhalation anesthetics rely upon the lungs for uptake and elimination. Both inhalation and intravenously administered anesthetics produce prominent respiratory side effects. Moreover, muscle paralysis, uncommon positioning throughout surgery, and techniques such as one-lung anesthesia and cardiopulmonary bypass profoundly alter normal pulmonary physiology. This article critiques the fundamental pulmonary ideas essential for understanding and making use of anesthetic methods. Although the pulmonary results of every of the assorted anesthetic brokers are discussed elsewhere in the e-book, this chapter additionally evaluations the overall results of general anesthesia on lung function. Rib Cage & Muscles of Respiration the rib cage accommodates the 2 lungs, each surrounded by its own pleura. The apex of the chest is small, allowing only for entry of the trachea, esophagus, and blood vessels, whereas the bottom is fashioned by the diaphragm. Contraction of the diaphragm-the principal pulmonary muscle-causes the bottom of the thoracic cavity to descend 1. Accessory respiratory muscular tissues additionally increase chest volume (and lung expansion) by their action on the ribs. Each rib (except for the final two) articulates posteriorly with a vertebra and is angulated downward as it attaches anteriorly to the sternum. During regular breathing, the diaphragm, and, to a lesser extent, the external intercostal muscles, are liable for inspiration; expiration is generally passive. With growing effort, the sternocleidomastoid, scalene, and pectoralis muscles could be recruited throughout inspiration. The sternocleidomastoid muscular tissues assist in elevating the rib cage, whereas the scalene muscles prevent inward displacement of the upper ribs during inspiration. Expiration is generally passive within the supine place, but turns into active within the upright position and with increased effort. Exhalation could also be facilitated by the abdominal muscles (rectus abdominis, exterior and inner indirect, and transversus) and maybe the internal intercostal muscles-aiding the downward motion of the ribs.
Paxil 10mg genericIn such situations, the movement of water out of cells (down its osmotic gradient) is accompanied by motion of K+ out of cells. Hypothermia has been reported to decrease plasma [K+] on account of cellular uptake. Rewarming reverses this shift and will lead to transient hyperkalemia if potassium was given during the hypothermia. Urinary Excretion of Potassium Urinary potassium excretion typically parallels its extracellular concentration (see previous discussion). Extracellular [K+] is a significant determinant of aldosterone secretion from the adrenal gland. Hyperkalemia stimulates aldosterone secretion, whereas hypokalemia suppresses aldosterone secretion. Renal tubular move in the distal nephron can also be an important determinant of urinary potassium excretion as a outcome of high tubular flow rates (as throughout osmotic diuresis) improve potassium secretion by keeping the capillary to renal tubular gradient for potassium secretion high. Conversely, sluggish tubular move rates improve [K+] in tubular fluid and decrease the gradient for K+ secretion, thereby decreasing renal potassium excretion. Plasma potassium concentration usually correlates poorly with the entire potassium deficit. A decrease in plasma [K+] from four mEq/L to three mEq/L normally represents a 100- to 200-mEq complete physique deficit, whereas plasma [K+] under 3 mEq/L can represent a deficit of 200 mEq to 400 mEq. Increased gastrointestinal lack of potassium is most commonly due to nasogastric suctioning or to persistent vomiting or diarrhea. Other gastrointestinal causes embrace losses from fistulae, laxative abuse, villous adenomas, and pancreatic tumors secreting vasoactive intestinal peptide. Chronic elevated sweat formation occasionally causes hypokalemia when potassium consumption is proscribed. Dialysis with a low-potassium-containing dialysate resolution also can trigger hypokalemia. Uremic sufferers may actually have a total body potassium deficit (primarily intracellular) regardless of a standard and even high plasma concentration; the absence of hypokalemia in these cases is probably as a end result of acidosis-induced intercompartmental shifts. Dialysis in these sufferers unmasks the whole physique potassium deficit and often results in hypokalemia. Urinary [K+] lower than 20 mEq/L is generally indicative of increased extrarenal K+ losses, whereas concentrations greater than 20 mEq/L suggest renal losing of K+. Low potassium intake, nonetheless, typically accentuates the effects of increased potassium loss. Hypokalemia as a end result of the Intracellular Movement of Potassium Hypokalemia due to the intracellular movement of potassium occurs with alkalosis, insulin remedy, 2adrenergic agonists, and hypothermia and through assaults of hypokalemic periodic paralysis. Cellular K+ uptake by purple blood cells (and platelets) additionally accounts for the hypokalemia seen in sufferers just lately treated with folate or vitamin B12 for megaloblastic anemia. Clinical Manifestations of Hypokalemia Hypokalemia can produce widespread organ dysfunction (Table 49�10). Renal wasting of potassium is most commonly the results of diuresis or enhanced mineralocorticoid exercise. Hypokalemia induced by diuretics is usually associated with metabolic alkalosis; as the kidneys absorb sodium to compensate for intravascular volume depletion and within the presence of diuretic-induced hypochloremia, bicarbonate is absorbed and potassium is excreted. Increased ammonia manufacturing represents intracellular acidosis; hydrogen ions move intracellularly to compensate for intracellular potassium losses. The resulting metabolic alkalosis, along with increased ammonia manufacturing, can precipitate encephalopathy in sufferers with superior liver illness. Treatment of Hypokalemia the treatment of hypokalemia is determined by the presence and severity of any associated organ dysfunction. Digoxin therapy-as properly as the hypokalemia itself-sensitizes the guts to adjustments in potassium ion concentration. Increased myocardial cell automaticity and delayed repolarization promote each atrial and ventricular arrhythmias. Neuromuscular results of hypokalemia embrace skeletal muscle weak point, hyporeflexia, muscle cramping, ileus, and, not often, flaccid paralysis or three. Intravenous replacement of potassium chloride is normally reserved for sufferers with, or in danger for, important cardiac manifestations or severe muscle weak point. The goal of intravenous therapy is to take away the patient from instant hazard, not to right the complete potassium deficit. Dextrose-containing options should be prevented because the resulting hyperglycemia and secondary insulin secretion could worsen the low plasma [K+]. Potassium chloride is the preferred potassium salt when a metabolic alkalosis can be current because it additionally corrects the chloride deficit mentioned earlier. Potassium bicarbonate or equivalent (K+ acetate or K+ citrate) is preferable for sufferers with metabolic acidosis. Potassium phosphate is a suitable various with concomitant hypophosphatemia (eg, diabetic ketoacidosis). When potassium consumption is elevated slowly, the kidneys can excrete as a lot as 500 mEq of K+ per day. The sympathetic nervous system and insulin secretion also play important roles in preventing acute will increase in plasma [K+] following acquired potassium masses. Hyperkalemia may end up from (1) an intercompartmental shift of potassium ions, (2) decreased urinary excretion of potassium, or, rarely, (3) an elevated potassium intake or elevated release from a previously ischemic organ (Table 49�11). The determination to proceed with elective surgical procedure is usually primarily based on lower plasma [K+] limits somewhere around 3 mEq/L. The decision, nevertheless, also wants to be based mostly on the rate at which the hypokalemia developed in addition to the presence or absence of secondary organ dysfunction. The exception is sufferers receiving digoxin, who threat creating digoxin toxicity from the hypokalemia; plasma [K+] values above 4 mEq/L are fascinating in such patients. Intravenous potassium must be given if atrial or ventricular arrhythmias develop. Glucose-free intravenous options ought to be used and hyperventilation averted to stop further decreases in plasma [K+]. In vitro release of potassium from blood specimen leukocytes can also falsely indicate increased ranges in the measured plasma [K+] when the leukocyte rely exceeds 70,000 � 109/L. A comparable release of potassium from platelets might occur when the platelet depend exceeds 1,000,000 � 109/L. Hyperkalemia due to Extracellular Movement of Potassium Movement of K+ out of cells could be seen with acidosis, cell lysis following chemotherapy, hemolysis, rhabdomyolysis, massive tissue trauma, hyperosmolality, digitalis overdoses, during episodes of hyperkalemic periodic paralysis, and with administration of succinylcholine, 2-adrenergic blockers, and arginine hydrochloride. Hyperkalemia due to Decreased Renal Excretion of Potassium Decreased renal excretion of potassium may result from (1) marked reductions in glomerular filtration, (2) decreased aldosterone exercise, or (3) a defect in potassium secretion in the distal nephron. Glomerular filtration charges less than 5 mL/min are nearly all the time associated with hyperkalemia. Patients with lesser levels of kidney impairment also can readily develop hyperkalemia when faced with elevated potassium masses (dietary, catabolic, or iatrogenic).
Buy on line paxilNociceptors Nociceptors are characterized by a excessive threshold for activation and encode the intensity of stimulation by rising their discharge rates in a graded style. Following repeated stimulation, they characteristically display delayed adaptation, sensitization, and afterdischarges. In contrast to well-localized epicritic sensation, which may be transduced by specialized end organs on the afferent neuron (eg, pacinian corpuscle for touch), less well-localized protopathic sensation is transduced primarily by free nerve endings nociceptors that sense warmth and mechanical and chemical tissue harm. Nociceptor sorts include (1) mechanonociceptors, which reply to pinch and pinprick, (2) silent nociceptors, which respond solely within the presence of inflammation, and (3) polymodal mechanoheat nociceptors. Polymodal nociceptors are gradual to adapt to strong stress and show heat sensitization. Visceral Nociceptors Visceral organs are usually insensitive tissues that mostly contain silent nociceptors. Some organs seem to have particular nociceptors, similar to the center, lung, testis, and bile ducts. Most different organs, such as the intestines, are innervated by polymodal nociceptors that reply to clean muscle spasm, ischemia, and irritation. Like somatic nociceptors, those within the viscera are the free nerve endings of main afferent neurons whose cell our bodies lie in the dorsal horn. These afferent nerve fibers, however, frequently travel with efferent sympathetic nerve fibers to attain the viscera. Nociceptive C fibers from the esophagus, larynx, and trachea journey with the vagus nerve to enter the nucleus solitarius in the brainstem. Afferent pain fibers from the bladder, prostate, rectum, cervix and urethra, and genitalia are transmitted into the spinal wire via parasympathetic nerves on the stage of the S2�S4 nerve roots. Though relatively few in contrast with somatic ache fibers, fibers from main visceral afferent neurons enter the twine and synapse more diffusely with single fibers, typically synapsing with a quantity of dermatomal ranges and sometimes crossing to the contralateral dorsal horn. Cutaneous Nociceptors Nociceptors are current in both somatic and visceral tissues. Primary afferent neurons reach tissues by traveling along spinal somatic, sympathetic, or parasympathetic nerves. Somatic nociceptors embrace these in skin (cutaneous) and deep tissues (muscle, tendons, fascia, and bone), whereas visceral nociceptors embrace those in inner organs. Chemical Mediators of Pain Several neuropeptides and excitatory amino acids operate as neurotransmitters for afferent neurons subserving pain (Table 47�4). Many, if not most, of those neurons contain more than one neurotransmitter, which are concurrently released. Also found in other elements of the nervous system and the intestines, Deep Somatic Nociceptors Deep somatic nociceptors are less sensitive to noxious stimuli than cutaneous nociceptors but are simply sensitized by irritation. Specific nociceptors exist in muscular tissues and joint capsules, they usually reply to mechanical, thermal, and chemical stimuli. Sensitization may be manifested as an enhanced response to noxious stimulation or a newly acquired responsiveness to a wider range of stimuli, including nonnoxious stimuli. In the periphery, substance P neurons ship collaterals that are intently related to blood vessels, sweat glands, hair follicles, and mast cells within the dermis. Substance P�releasing neurons also innervate the viscera and ship collateral fibers to paravertebral sympathetic ganglia; intense stimulation of viscera, due to this fact, can cause direct postganglionic sympathetic discharge. Primary Hyperalgesia Sensitization of nociceptors results in a decrease in threshold, a rise within the frequency response to the identical stimulus depth, a decrease in response latency, and spontaneous firing even after cessation of the stimulus (afterdischarges). Such sensitization, termed primary hyperalgesia, commonly occurs with injury and following software of heat and is mediated by the release of noxious substances from damaged tissues. Histamine is launched from mast cells, basophils, and platelets, whereas serotonin is released from mast cells and platelets. The lipoxygenase pathway converts arachidonic acid into hydroperoxy compounds, which are subsequently transformed into leukotrienes. The analgesic impact of corticosteroids is likely the outcome of inhibition of prostaglandin manufacturing via blockade of phospholipase A2 activation. Facilitation 6 At least three mechanisms are liable for central sensitization in the spinal wire: 1. Dorsal horn neurons increase their receptive fields such that adjacent neurons become aware of stimuli (whether noxious or not) to which they were beforehand unresponsive. Enhancement of flexion reflexes is observed each ipsilaterally and contralaterally. Secondary Hyperalgesia Neurogenic inflammation, additionally called secondary hyperalgesia, plays an necessary role in peripheral sensitization following injury. It is manifested by the triple response of Lewis: a pink flush across the web site of harm (flare), local tissue edema, and sensitization to noxious stimuli. Capsaicin utilized topically in a gel, cream, or patch depletes substance P, diminishes neurogenic irritation, and is beneficial for some patients with postherpetic neuralgia. Both prostaglandins and nitric oxide facilitate the discharge of excitatory amino acids within the spinal wire. Inhibition Transmission of nociceptive enter in the spinal twine may be inhibited by segmental activity in the twine itself, as properly as by descending neural activity from supraspinal centers. These two phenomena help a "gate" principle for pain processing within the spinal cord as initially hypothesized by Melzack and Wall. Activation of glycine receptors also will increase Cl� conductance throughout neuronal cell membranes. At least two receptors are recognized: A1, which inhibits adenyl cyclase, and A2, which stimulates adenyl cyclase. Supraspinal inhibition-Several supraspinal buildings ship fibers down the spinal cord to inhibit pain in the dorsal horn. Stimulation of the periaqueductal gray space within the midbrain produces widespread analgesia in humans. Axons from these tracts act presynaptically on primary afferent neurons and postsynaptically on second-order neurons (or interneurons). These pathways mediate their antinociceptive motion through 2-adrenergic, serotonergic, and opiate (, and) receptor mechanisms. These pathways clarify the analgesic efficacy of antidepressants that block reuptake of catecholamines and serotonin. Inhibitory adrenergic pathways originate primarily from the periaqueductal gray area and the reticular formation. Norepinephrine mediates this action by way of activation of presynaptic or postsynaptic 2 receptors. These opioids act presynaptically to hyperpolarize major afferent neurons and inhibit the discharge of substance P; they also seem to cause some postsynaptic inhibition. Exogenous opioids preferentially act postsynaptically on the second-order neurons or interneurons in the substantia gelatinosa.
Order paxil online pillsThe disease is autosomal dominant, with an incidence of 1:8000, and often turns into clinically apparent within the second to third decade of life, but it has additionally been reported as a paraneoplastic dysfunction in association with thymoma. Myotonia is the principal early manifestation; muscle weak point and atrophy become more outstanding as the disease progresses. This weakness and atrophy often affect cranial muscle tissue (orbicularis oculi and oris, masseter, and sternocleidomastoid), and in contrast to most myopathies, distal muscular tissues greater than proximal muscular tissues. Multiple organ methods are involved in myotonic dystrophy, as evidenced by presenile cataracts, premature frontal baldness, hypersomnolence with sleep apnea, and endocrine dysfunction resulting in pancreatic, adrenal, thyroid, and gonadal insufficiency. Respiratory involvement results in decreased important capability, and continual hypoxemia may cause cor pulmonale. Cardiac manifestations, which are sometimes current before other medical signs appear, may include cardiomyopathy, atrial arrhythmias, and varying levels of heart block. The myotonia is usually described by sufferers as a "stiffness" that will reduce with continued activity-the so-called "warm-up" phenomenon. Antimyotonic treatment may embrace mexiletine, phenytoin, baclofen, dantrolene, or carbamazepine. Limb-Girdle Dystrophy Limb-girdle muscular dystrophy is a heterogeneous group of genetic neuromuscular illnesses. Limb-girdle syndromes embody extreme childhood autosomal recessive muscular dystrophy and different incompletely defined autosomal recessive syndromes corresponding to Erb (scapulohumeral type) and Leyden�Mobius (pelvifemoral type) dystrophies. Most patients current between childhood and the second or third decade of life with slowly progressive muscle weak point which will involve the shoulder girdle, the hip girdle, or both. Cardiac involvement is relatively uncommon however might present as frequent arrhythmias or congestive heart failure. Respiratory problems, such as hypoventilation and recurrent respiratory infections, might happen. Duchenne and Becker Muscular Dystrophies the anesthetic management of these patients is sophisticated not only by muscle weak spot but additionally by cardiac and pulmonary manifestations. Intraoperative positioning may be difficult by kyphoscoliosis or by flexion contractures of the 8 extremities or neck. Inhalational anesthetics have been related to rhabdomyolysis and hyperkalemia in sufferers with Duchene muscular dystrophy in circumstances where no succinylcholine was employed. Marked respiratory and circulatory depression could also be seen with risky anesthetics in patients with superior disease, and regional or native anesthesia could also be preferable in these patients. Patients with very important capacities lower than 30% of predicted are at greatest danger and infrequently require short-term postoperative mechanical air flow. Myotonic Dystrophy Patients with myotonic dystrophy are at elevated threat for perioperative respiratory and cardiac complications. Most perioperative issues arise in sufferers with severe weakness and in those circumstances in which surgeons and anesthesiologists are unaware of the analysis. The prognosis of myotonic dystrophy has been made in some sufferers in the course of investigating prolonged apnea following basic anesthesia. Patients with myotonic dystrophy are sometimes sensitive to even small doses of opioids, sedatives, and inhalation and intravenous anesthetic agents, all of which may trigger sudden and prolonged apnea. Succinylcholine is relatively contraindicated as a result of it could precipitate intense myotonic contraction of the diaphragm, chest wall, or laryngeal muscular tissues, making ventilation difficult or unimaginable. Other drugs that act on the motor end-plate, such as neostigmine, and physostigmine, can worsen myotonia. Postoperative shivering may induce myotonic contractions in the recovery room, and doses of meperidine can often stop such shivering and should preempt myotonic contractions. Induction of anesthesia without complications has been reported with a variety of brokers together with inhalation brokers and propofol. An affiliation between myotonic dystrophy and malignant hyperthermia has been suggested however not established. The principal postoperative complications of myotonic dystrophy are prolonged hypoventilation, atelectasis, aspiration, and pneumonia. Patients undergoing upper abdominal surgery or those with severe proximal weak spot usually tend to experience pulmonary complications. Close postoperative monitoring for arrhythmias ought to be accompanied by aggressive pulmonary hygiene with bodily remedy and incentive spirometry. Other Forms of Muscular Dystrophy Patients with facioscapulohumeral and limb-girdle muscular dystrophy generally have normal responses to anesthetic brokers. Many sufferers have very well-developed musculature as a outcome of near constant muscle contraction. Antimyotonic remedy contains phenytoin, mexiletine, quinine sulfate, or procainamide. Other medicines which have been used embody tocainide, dantrolene, prednisone, acetazolamide, and taurine. Paramyotonia congenita is a very uncommon autosomal dominant disorder characterized by transient stiffness (myotonia) and, often, weak point after exposure to chilly temperatures. The stiffness worsens with activity, in contrast to true myotonia, thus the time period paramyotonia. Serum potassium concentration might rise following an attack much like hyperkalemic periodic paralysis (discussed next). Medications which were used to block the cold response include mexiletine and tocainide. Anesthetic management of patients with myotonia congenita and paramyotonia is complicated by an irregular response to succinylcholine, intraoperative myotonic contractions, and the need to avoid hypothermia. Infiltration of muscular tissues in the operative subject with a dilute local anesthetic might alleviate refractory myotonic contraction. Among sufferers with these type of myotonia, none have been reported with optimistic in vitro exams for malignant hyperthermia. Excised muscle in these sufferers does, however, show a prolonged myotonic contraction when exposed to succinylcholine. Excessive muscle contraction during anesthesia, subsequently, doubtless represents aggravation of myotonia and never malignant hyperthermia. Symptoms often start in childhood, with episodes lasting a few hours and sometimes sparing respiratory muscle involvement. The weak point often lasts less than 1 h however can final a number of days, and frequent assaults may result in progressive, long-term weak spot in some patients. Muscle strength and serum potassium concentrations are often regular between assaults. The episodes of weakness are as a end result of a loss of muscle fiber excitability secondary to partial depolarization of the resting potential. This partial depolarization prevents the technology of action potentials and thereby precipitates weak point. Periodic paralysis is classed into main genetic channelopathies and secondary acquired types. The genetic sorts are because of dominantly inherited mutations in the voltage-gated sodium, calcium, or potassium ion channels. Different defects in the identical channel can cause completely different medical footage, whereas mutations in several channels might have comparable medical footage.
Discount 10 mg paxil with amexIntraoperative Management Selection of anesthetic brokers should be tailor-made to every patient. The decreased lung compliance ends in high peak inspiratory pressures during positive-pressure air flow and increases the chance of barotrauma and volutrauma. Right ventricular operate could additionally be challenged because of to will increase in pulmonary vascular resistance secondary to permissive hypercapnia. The inflammatory course of may be primarily confined to the lungs or could additionally be part of a generalized multiorgan process. Causes embrace hypersensitivity pneumonitis from occupational and environmental pollution, drug toxicity (bleomycin and nitrofurantoin), radiation pneumonitis, idiopathic pulmonary fibrosis, autoimmune illnesses, and sarcoidosis. Preoperative Considerations Patients usually current with dyspnea on exertion and generally a nonproductive cough. Physical examination could reveal fantastic (dry) crackles over the lung bases, and, in late phases, proof of right ventricular failure. The chest radiograph progresses from a "ground-glass" appearance to distinguished reticulonodular markings, and, lastly, to a "honeycomb" look. Treatment is directed at abating the illness process and preventing further exposure to the causative agent (if known). If the affected person has persistent hypoxemia, oxygen therapy may be started to prevent, or attenuate, proper ventricular failure. Preoperative Management Preoperative analysis ought to concentrate on the underlying illness process and the degree of pulmonary impairment. A important capability of less than 15 mL/kg is indicative of severe dysfunction (normal is >70 mL/kg). Protective ventilation methods employed in ventilated patients within the intensive care unit must be continued via to the operating room. Nitric oxide could also be used to reduce pulmonary vascular resistance and reduce the work of the right ventricle. Following anticoagulation, blood is drained from venous cannulae and delivered to a membrane oxygenator. Oxygenated blood can then both be returned both to the venous system, if cardiac function is preserved, or pumped into the arterial circulation, bypassing the center and lungs. They embody pleural effusions, pneumothorax, mediastinal lots, kyphoscoliosis, pectus excavatum, neuromuscular issues, and elevated intraabdominal strain from ascites, pregnancy, or bleeding. Anesthetic concerns are similar to those mentioned for intrinsic restrictive issues. Pulmonary Embolism Preoperative Considerations Pulmonary embolism outcomes from the entry of blood clots, fats, tumor cells, air, amniotic fluid, or international material into the venous system. Clots from the lower extremities, pelvic veins, or, much less commonly, the right side of the guts are often accountable. Pulmonary emboli acutely enhance pulmonary vascular resistance by lowering the cross-sectional space of the pulmonary vasculature, causing reflex and humoral vasoconstriction. Localized or generalized reflex bronchoconstriction additional increases areas with low (V/Q) ratios. The affected space loses its surfactant inside hours and will turn into atelectatic inside 24 to forty eight h. Pulmonary infarction happens if the embolus includes a large vessel and collateral blood move from the bronchial circulation is inadequate for that part of the lung (incidence <10%). In beforehand wholesome individuals, occlusion of more than 50% of the pulmonary circulation (massive pulmonary embolism) is important earlier than sustained pulmonary hypertension is seen. Patients with preexisting cardiac or pulmonary illness can develop acute pulmonary hypertension with occlusions of lesser magnitude. A sustained improve in proper ventricular afterload can precipitate acute proper ventricular failure and hemodynamic collapse. If the patient survives acute pulmonary thromboembolism, the thrombus often begins to resolve within 1 to 2 weeks. Diagnosis Clinical manifestations of pulmonary embolism include sudden tachypnea, dyspnea, chest ache, or hemoptysis. Symptoms are sometimes absent or mild and nonspecific until massive embolism has occurred. Arterial blood gas evaluation usually exhibits mild hypoxemia with respiratory alkalosis (the latter as a result of an increase in ventilation). The chest radiograph is often regular, however may present an space of oligemia (radiolucency), a wedge-shaped density with an infarct, atelectasis with an elevated diaphragm, or an asymmetrically enlarged proximal pulmonary artery with acute pulmonary hypertension. Cardiac signs embrace tachycardia and broad mounted splitting of the S2 coronary heart sound; hypotension with elevated central venous strain is usually indicative of right ventricular failure. The electrocardiogram incessantly reveals tachycardia and will show indicators of acute cor pulmonale, similar to new proper axis deviation, right bundlebranch block, and tall peaked T waves. Computed tomography angiography is carried out emergently when pulmonary embolism is suspected. Echocardiography can additionally be used to help within the analysis underneath emergent conditions in unstable sufferers perioperatively. Sometimes clot could be seen in the proper coronary heart and pulmonary artery confirming the analysis. At other times, solely the signs of right ventricular overload are seen (eg, tricuspid regurgitation, right ventricular dilation). The left ventricle may be relatively under-loaded secondary to the inadequate delivery of blood across the pulmonary circulation as a consequence of the embolus. Treatment and Prevention the best remedy for perioperative pulmonary embolism is prevention. The use of intermittent pneumatic compression of the legs may decrease the incidence of venous thrombosis in the legs, but not in the pelvis or the guts. After a pulmonary embolism, parenteral anticoagulation prevents the formation of latest blood clots or the extension of current clots. All patients ought to start warfarin therapy concurrent with beginning parenteral remedy, and the 2 ought to overlap for no less than 5 days. The international normalized ratio also needs to be throughout the therapeutic vary (>2. Thrombolytic therapy is indicated in patients with huge pulmonary embolism and hypotension. Recent surgical procedure and energetic bleeding are contraindications to anticoagulation and thrombolytic remedy. In these cases, an inferior vena cava filter may be placed to forestall recurrent pulmonary emboli. Pulmonary embolectomy may be lifesaving for hemodynamically unstable patients with large embolism in whom thrombolytic remedy is contraindicated or ineffective. Preoperative Management Patients with acute pulmonary embolism could present within the working room for placement of an inferior vena cava filter, or, not often, for pulmonary embolectomy. In most instances, the patient will have a historical past of pulmonary embolism and presents for unrelated surgical procedure; on this group of sufferers, the risk of interrupting anticoagulant therapy perioperatively is unknown.
Cheap 40 mg paxil visaThe jaw-thrust maneuver, particularly when combined with light optimistic airway strain by way of a tight-fitting face mask, usually breaks laryngospasm. Insertion of an oral or nasal airway is also helpful in ensuring a patent airway down to the level of the vocal cords. Secretions, blood, or other international material in the hypopharynx must be suctioned to forestall recurrence. Refractory laryngospasm must be handled with a small dose of intravenous succinylcholine (10�20 mg in adults) and positive-pressure air flow with 100% oxygen. Endotracheal intubation may often be essential to reestablish ventilation; emergent cricothyrotomy or transtracheal jet air flow is indicated if intubation is unsuccessful in such instances. Glottic edema following airway instrumentation is an important reason for airway obstruction in infants and younger youngsters because of the relatively small airway lumen. Significant pharyngeal and glottic edema and irritability, with friable, oozing oropharyngeal mucosa, is widespread in sufferers undergoing head and neck radiation remedy. Postoperative wound hematomas following thyroid, carotid artery, and other neck procedures can quickly compromise the airway, and opening the wound instantly relieves tracheal compression in most cases. Rarely, a gauze "throat pack" may be unintentionally left within the hypopharynx following oral surgery and may trigger instant or delayed full airway obstruction. Decannulation of a recent tracheostomy is hazardous as a result of recannulation may be very tough or unimaginable when the wound has not but healed right into a well-formed observe. When a tracheostomy has been carried out throughout the earlier 4 weeks, intentional substitute of a tracheostomy cannula ought to only be performed with a surgeon at the bedside and with a tracheostomy instrument set, along with different appropriate troublesome airway tools, immediately out there. Hypoventilation Hypoventilation, which is generally outlined as a Paco2 higher than forty five mm Hg, is common following general anesthesia. Significant hypoventilation might present clinical indicators when the Paco2 is greater than 60 mm Hg or arterial blood pH is lower than 7. Mild to average respiratory acidosis may trigger tachycardia, hypertension, and cardiac irritability by way of sympathetic stimulation, however more extreme acidosis produces circulatory despair (see Chapter 50). If important hypoventilation is suspected, assessment and management is facilitated by capnography or arterial blood gasoline measurement, or each. Opioid-induced respiratory melancholy characteristically produces a sluggish respiratory fee, often with giant tidal volumes. The affected person is somnolent, but often aware of verbal and physical stimulus and able to breathe on command. Proposed mechanisms include variations within the intensity of stimulation throughout restoration and delayed release of the opioid from peripheral tissue compartments because the patient rewarms or begins to move. Regardless of the trigger, generalized weakness, uncoordinated actions ("fish out of water"), shallow tidal volumes, and tachypnea are often obvious. The prognosis of inadequate neuromuscular blockade reversal may be made with a nerve stimulator in unconscious patients; head carry and grip energy can be assessed in awake and cooperative patients. Splinting due to incisional pain, diaphragmatic dysfunction following upper stomach or thoracic surgery, belly distention, and tight abdominal dressings are other components that may contribute to hypoventilation. Marked hypoventilation and respiratory acidosis may end up when these components are superimposed on an impaired ventilatory reserve because of preexisting pulmonary, neuromuscular, or neurological illness. Treatment of Hypoventilation Treatment should usually be directed at the underlying trigger, however marked hypoventilation all the time requires assisted or controlled ventilation till causal factors 7 are identified and corrected. Hypoventilation with obtundation, circulatory melancholy, and extreme acidosis (arterial blood pH <7. If intravenous naloxone is used to reverse opioid-induced respiratory despair, titration in small increments (80 mcg in adults) usually avoids issues and minimizes reversal of analgesia. Antagonism of opioid-induced melancholy with large doses of naloxone typically leads to sudden pain and marked improve in sympathetic tone. The latter can precipitate a hypertensive disaster, pulmonary edema, and myocardial ischemia or infarction. If residual muscle paralysis is current, sugammadex (if rocuronium or vecuronium has been administered) or a further cholinesterase inhibitor may be administered. Inadequate reversal in spite of a full dose of sugammadex or a cholinesterase inhibitor necessitates controlled ventilation underneath shut statement until adequate restoration of muscle power occurs. Mild to reasonable hypoxemia (Pao2 50�60 mm Hg) in younger wholesome patients may be nicely tolerated initially, however with growing length or severity, the initial sympathetic stimulation typically seen is changed with progressive acidosis and circulatory despair. Hypoxemia may also be suspected from restlessness, agitation, tachycardia, or atrial or ventricular dysrhythmias. Arterial blood gas measurements may be performed to confirm the prognosis and information therapy. A lower in cardiac output or an increase in oxygen consumption (as with shivering) will intensify hypoxemia. Diffusion hypoxia (see Chapter 8) is an unusual cause of hypoxemia when recovering patients are given supplemental oxygen. Hypoxemia due exclusively to hypoventilation without obstruction can additionally be unusual in patients receiving supplemental oxygen, unless marked hypercapnia or a concomitant enhance in intrapulmonary shunting is present. The lack of lung quantity is often attributed to microatelectasis, as atelectasis is commonly not recognized on a chest radiograph. Postoperative pulmonary edema may current with wheezing or less generally with pink frothy fluid within the airway. The risk of a postoperative pneumothorax should all the time be thought of following central line placement, supraclavicular or intercostal blocks, belly or chest trauma (including rib fractures), neck dissection, thyroidectomy (especially if the thyroid dissection extends into the thorax), tracheostomy, nephrectomy, or other retroperitoneal or intraabdominal procedures (including laparoscopy), particularly if the diaphragm could have been penetrated or disrupted. Patients with subpleural blebs or massive bullae can also develop pneumothorax during positive-pressure ventilation. Treatment of Hypoxemia Oxygen remedy, with or without positive airway strain, and aid of any current airway obstruction with airway maneuvers, an oral or nasal airway, or oropharyngeal suctioning, present the cornerstones of treatment for hypoxemia. Routine administration of 30% to 60% oxygen is usually sufficient to prevent hypoxemia with even average hypoventilation and hypercapnia. Importantly, medical signs of hypoventilation and hypercapnia may be masked by routine oxygen administration. Patients with underlying pulmonary or cardiac illness might require higher concentrations of oxygen; oxygen therapy must be guided by Spo2 or arterial blood gas measurements. The chest radiograph (preferably with the patient positioned sitting upright) is efficacious in assessing lung volume and coronary heart size and in demonstrating pneumothorax, atelectasis, pulmonary infiltrates. However, in instances of pulmonary aspiration, infiltrates are often initially absent. If pneumothorax is suspected, a chest radiograph taken at end-expiration helps spotlight the pneumothorax by offering the greatest distinction between lung tissue and adjoining air in the pleural area. In the intubated patient with hypoxemia, a chest radiograph must be used to confirm correct endotracheal tube position. Transthoracic ultrasonography can be a valuable software for rapid, accurate assessment of endotracheal tube placement and analysis of lobar consolidation, pleural effusion, and pneumothorax.
Discount paxil genericOnce the needle has handed through the fascia iliaca, cautious aspiration is carried out and 30 to forty mL of local anesthetic is injected. This block usually anesthetizes each the femoral nerve and lateral femoral cutaneous nerves, since the local anesthetic is deposited beneath the fascia iliaca between the two nerves that run in the same plane between the fascia and underlying muscle. It may be anesthetized as a complement to a femoral nerve block or as an isolated block for limited anesthesia of the lateral thigh. As there are few vital buildings in proximity to the lateral femoral cutaneous nerve, issues with this block are exceedingly uncommon. Obturator Nerve Block A block of the obturator nerve is normally required for complete anesthesia of the knee and is most frequently performed in combination with femoral and sciatic nerve blocks for this function. This nerve exits the pelvis and enters the medial thigh by way of the obturator foramen, which lies beneath the superior pubic ramus. After identification of the pubic tubercle, a long (10-cm) block needle is inserted 1. Redirecting laterally and caudally, the needle is advanced an additional 2 to four cm till a motor response (thigh adduction) is elicited and maintained below 0. Following careful aspiration for the nonappearance of blood, 15 to 20 mL of local anesthetic is injected. Hence, the posterior lumbar plexus block has one of the highest complication charges of any peripheral nerve block; these embody retroperitoneal hematoma, intravascular local anesthetic injection with toxicity, intrathecal and epidural injections, and renal capsular puncture with subsequent hematoma. Modern posterior lumbar plexus blocks deposit native anesthetic throughout the body of the psoas muscle. Contact pubic tubercle (1), then redirect laterally and caudally (2) until a motor response is elicited. A line is first drawn through the lumbar spinous processes, and both iliac crests are identified and related with a line to approximate the level of L4. The posterior superior iliac spine is then palpated and a line is drawn cephalad, parallel to the first line. If obtainable, ultrasound imaging of the transverse course of may be helpful to estimate lumbar plexus depth. A long (10- to 15-cm) insulated needle is inserted on the level of intersection between the transverse (intercristal) line and the intersection of the lateral and center thirds of the two sagittal lines. The needle is advanced in an anterior direction till a femoral motor response is elicited (quadriceps contraction). If the transverse course of is contacted, the needle should be withdrawn slightly and "walked off " the transverse process in a caudal path, maintaining the needle within the parasagittal airplane. The needle should by no means be inserted greater than 3 cm previous Femoral nerve, lateral cutaneous nerve of thigh, obturator nerve Sciatic nerve, posterior femoral cutaneous nerve Needle insertion level Lateral femoral cutaneous n. Local anesthetic volumes greater than 20 mL will enhance the risk of bilateral unfold and contralateral limb involvement. Adductor Canal Block the adductor canal block is used for analgesia of the knee and medial leg; single injection or steady strategies can be utilized. The quadriceps muscle tissue are affected to a lesser diploma by an adductor canal block than by a femoral block, which may facilitate ambulation following knee surgical procedure. Bounded by the sartorius muscle and vasto-adductor membrane medially, the vastus medialis anteriorly, and the adductor muscles posteriorly, the adductor canal contains a number of nerves that present sensory innervation to the knee. Ultrasound the patient is positioned supine with the knee barely bent and the leg externally rotated. A lengthy (10-cm) block needle is placed 2 to three cm lateral to the transducer and superior in-plane to the triangular space deep to the sartorius muscle and vasto-adductor membrane and lateral to the artery. After cautious aspiration for nonappearance of blood, 15 to 20 mL of native anesthetic is injected. Trans-Sartorial Technique the saphenous nerve may be accessed proximal to the knee, simply deep to the sartorius muscle. Ultrasound may be used to identify the saphenous vein near the tibial tuberosity and facilitate a perivascular method, with infiltration in regards to the vein. Distal Saphenous Technique the medial malleolus is recognized, infiltrating 5 mL of local anesthetic in a line operating anteriorly across the ankle (see "Ankle Block," below). Sciatic Nerve Block the patient is positioned supine with the leg externally rotated. A high-frequency linear transducer is positioned in a transverse orientation on the mid-thigh. A long needle is inserted from medial to lateral (in-plane) or angled cephalad (outof-plane) and 5 to 10 mL of local anesthetic deposited inside this fascial plane. Blockade of the sciatic nerve might occur anyplace along its course and is indicated for surgical procedures involving the hip, thigh, knee, decrease leg, and foot. The posterior femoral cutaneous nerve is variably anesthetized as properly, relying on the method. Proximal Saphenous Technique A short block needle is inserted 2 cm distal to the tibial tuberosity and directed medially, infiltrating 5 to A. Posterior (Classic or Labat) Approach the affected person is positioned laterally with the facet to be blocked within the nondependent position. Next, a line is drawn from the greater trochanter to the sacral hiatus and the intersection point is marked; this is the initial needle insertion level. The needle is superior through the gluteal muscular tissues (a motor response of those muscular tissues could also be encountered) until plantar- or dorsiflexion is elicited (plantarflexion or foot inversion is preferred for surgical anesthesia). Before continuing with this block, which carries a danger of vascular puncture (femoral artery and vein), patient-specific dangers must be considered (eg, coagulopathy and vascular grafting). In addition, if combining this block with the femoral nerve block in an unanesthetized patient, performing the sciatic block first is beneficial to avoid passing the block needle via a beforehand anesthetized femoral nerve. A second line is drawn parallel to the first that traverses the larger trochanter (intertrochanteric line). Next, these two traces are linked with a third line drawn from the point between the medial one-third and lateral two-thirds of the first line, at a 90� angle, and prolonged caudally to intersect with B. Anterior Approach After leaving the sciatic notch, the sciatic nerve descends behind the lesser trochanter to a position posterior to the femur. Lateral or prone positioning could current a challenge for some sufferers requiring a sciatic nerve block (ie, aged sufferers, pediatric sufferers beneath basic anesthesia). A long (10- to 15-cm) needle is inserted by way of this intersection and directly posterior until foot inversion or plantarflexion is elicited (dorsiflexion is suitable for postoperative analgesia). Often with this method, the femur is contacted before the needle reaches the sciatic nerve. When this happens, the needle ought to be withdrawn 2 to 3 cm, the patient ought to be requested to internally rotate the leg, and then the needle must be advanced. Ultrasound-With the patient positioned supine and the leg externally rotated, a low-frequency curvilinear transducer is placed transversely over the medial thigh, approximately on the stage of the lesser trochanter. The femur, femoral vessels, adductor muscles, and gluteus maximus are identified in crosssection. The elliptical, hyperechoic sciatic nerve is found within the fascial plane between adductors and gluteus muscular tissues, posterior to the femur. Using an extended (10-cm) needle, the nerve is approached in-plane (anterior to posterior) or out-of-plane (cephalad to caudad), taking care to keep away from femoral vessels, till the needle tip lies in this muscle aircraft and a neighborhood anesthetic injection can be noticed as hypoechoic spread surrounding the sciatic nerve. Subgluteal Approach A subgluteal approach to the sciatic nerve is a useful alternative to the standard posterior strategy as a result of the landmarks are often extra easily recognized and less tissue is traversed.
References - Levesque PE, Bauer SB, Atala A, et al: Ten-year experience with the artificial urinary sphincter in children, J Urol 156:625n628, 1996.
- Gettman MT, Lotan Y, Roerhborn CG, et al: Cost-effective treatment for ureteropelvic junction obstruction: a decision tree analysis, J Urol 169:228, 2003.
- Gonzalez-Zulueta M, Bender CM, Yang AS, et al: Methylation of the 5? CpG island of the p16/CDKN2 tumor suppressor gene in normal and transformed human tissues correlates with gene silencing, Cancer Res 55:4531n4535, 1995.
- Pradeep PV, Mishra AK, Aggarwal V, et al: Adrenal cysts: an institutional experience, World J Surg 30(10):1817n1820, 2006.
|
|