"Safe 40 mg zerit, silent treatment."By: Lilja Bjork Solnes, M.B.A., M.D. - Program Director, Diagnostic Radiology Residency
- Assistant Professor of Radiology and Radiological Science
 https://www.hopkinsmedicine.org/profiles/results/directory/profile/5251718/lilja-solnes
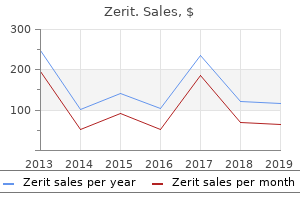
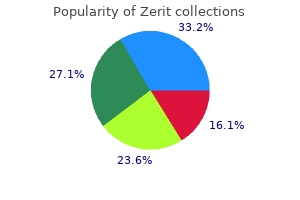
Zerit 40 mg with mastercardUnique to predictive models, this nomogram may be used a priori to calculate a D90 dose that doubtless achieves a desired end result with additional validation. Many of the side effects seen with brachytherapy are related to radiation publicity of the urethra, bladder, and rectum. These unwanted aspect effects can have critical quality-of-life implications, and brachytherapy requires knowledgeable consent from the affected person. In a potential evaluation of the standard of lifetime of sufferers undergoing primary therapy for prostate most cancers, Sanda et al. Long-term outcomes of retropubic everlasting 125iodine implantation of the prostate for clinically localized prostatic most cancers. A modified method allowing interactive ultrasound-guided three-dimensional transperineal prostate implantation. Postimplantation dosimetric evaluation of everlasting transperineal prostate implantation: improved dose distributions with an intraoperative computer-optimized conformal planning approach. Urinary morbidity following ultrasoundguided transperineal prostate seed implantation. Increased risk of rectal cancer after prostate radiation: a population-based research. Increased risk of colon most cancers after external radiation therapy for prostate cancer. Second primary cancer after radiotherapy for prostate cancer�a seer analysis of brachytherapy versus external beam radiotherapy. Permanent prostate brachytherapy: Dosimetric results and analysis of a learning curve with a dynamic dose-feedback method. Permanent implants using Au-198, Pd-103 and I-125: radiobiological considerations based on the linear quadratic mannequin. Freedom from progression for sufferers receiving 125I versus 103Pd for prostate brachytherapy. Threedimensional conformal exterior beam radiotherapy in contrast with everlasting prostate implantation in low-risk prostate cancer primarily based on endorectal magnetic resonance spectroscopy imaging and prostate-specific antigen level. Given its cost�benefit benefit over dearer radiation therapy modalities, brachytherapy should be the first modality for males requiring radiation therapy for prostate most cancers. Radical prostatectomy versus watchful waiting in localized prostate most cancers: the Scandinavian prostate most cancers group-4 randomized trial. Long-term results of conformal radiotherapy for prostate cancer: impact of dose escalation on biochemical tumor control and distant metastases-free survival outcomes. Targeted focal remedy: a minimally invasive ablation technique for early prostate most cancers. The function of external beam radiotherapy with I-125/Pd-103 brachytherapy for prostate carcinoma. Multicenter analysis of impact of high biologic efficient dose on biochemical failure and survival outcomes in patients with Gleason score 7�10 prostate most cancers treated with permanent prostate brachytherapy. Brachytherapy and Proton Beam Therapy for Treatment of Clinically-Localized, Low Risk Prostate Cancer: Institute for Clinical and Economic Review. The high quality of therapy is decided by the imaging used to plan and ship the treatment. As a outcome, enhancements within the supply of radiation therapy have been primarily based on advances in imaging modalities and the flexibility to incorporate these in to the planning and delivery of therapy. In addition, computer expertise has made it easier to incorporate an growing number of custom-made beams, which permit the radiation dose to be additional concentrated within the area of curiosity. Traditional radiation treatments usually use broad margins to accommodate potential movement or uncertainties throughout a treatment course. With more precise treatments, the dose to a target structure could be increased whereas lowering the dose to a neighboring crucial structure. Certain areas, such as the mind, are notably amenable to these varieties of therapies because movement is minimal or could be easily controlled. Many other parts of the physique are vulnerable to motion with lack of sub-centimeter accuracy with, for instance, casual respiration. In addition, tumors can change, either shrinking or actually rising in the course of the remedy course. These actions and adjustments result in decreased accuracy and either underdosing the goal or overdosing nearby important buildings. However, this course of is at present within the early levels and may be labor intensive. These strategies permit for dose escalation, which has been proven to enhance the finish result of localized prostate most cancers. Despite larger doses, the elevated accuracy permits for tighter margins to be used, leading to low morbidity. Recently, printed randomized trials evaluating the mortality outcomes of a screened group versus a nonscreened group confirmed conflicting results [3, 4]. Therefore, the advice emphasizes an informed discussion of the dangers and benefits of prostate most cancers screening prior to biopsy, and the choice of lively surveillance as a substitute of treatment for sure sufferers with prostate cancer. There are comparatively few basic contraindications to the usage of radiation therapy for therapy of definitive illness. These embrace prior treatment with pelvic radiation remedy and presence of active autoimmune disease, particularly scleroderma and lupus. Risk stratification Once the diagnosis of prostate cancer is made, a staging work-up ensues to have the ability to present extra prognostic information for risk stratification, which can help in management choices. Surgical lymph node staging can also be 1378 Section 7 Image-Guided Diagnostics and Therapeutics: Lower Tract Table 114. Other factors that contribute to higher acute toxicity include a greater variety of needles used to do the implant and the use of hormonal therapy [12]. On the other hand, sure intermediate-risk patients are likely to be candidates for brachytherapy alone. These information counsel that most intermediate-risk patients have a low danger of micrometastatic illness within the pelvis. Even though the risk of extracapsular disease is greater in these sufferers, these areas could also be adequately covered by an implant, since most extracapsular illness is situated inside 5 mm of the prostate capsule. Therefore, additional pathologic components, similar to number or share of optimistic cores, may be useful to determine whether or not a mixture treatment ought to be used. The 5-year progression-free survival was 74% for patients undergoing radiation remedy versus 52% present process remark [15]. Similar findings had been reported in a multi-institutional randomized medical trial evaluating adjuvant radiation remedy of 60�64 Gy to remark with a median follow-up of 10. Without an enchancment in survival, the controversy regarding whether or not or not to use adjuvant radiation therapy continues.
Generic zerit 40 mg on-lineRobot assisted partial nephrectomy versus laparoscopic partial nephrectomy for renal tumors: a multi-institutional analysis of perioperative outcomes. Effects of intermittent versus steady renal arterial occlusion on hemodynamics and function of the kidney. Ischemia with intermittent reperfusion reduces functional and morphologic harm following renal ischemia within the rat. Ischemic preconditioning and intermittent clamping increase the tolerance of fatty liver to hepatic ischemia-reperfusion injury in the rat. Effects of ischemic liver preconditioning on hepatic ischemia/ reperfusion injury within the rat. Positive margins in laparoscopic partial nephrectomy in 855 cases: a multiinstitutional survey from the United States and Europe. Multiple studies have reported vital advantages with the laparoscopic strategy in comparison with the standard open strategy. This minimally invasive approach provides patients less postoperative ache, a shorter hospital stay, a quicker return to regular activities, and a better beauty result. In the previous decade, robotic expertise has been introduced to help laparoscopic procedures. With a threedimensional (3D) display to enhance depth perception and instruments containing a "wrist" joint to enhance dexterity, robot help may offer benefits over standard laparoscopy, doubtlessly decreasing the technical complexity of the process and enabling less skilled surgeons to deliver minimally invasive surgical procedure to their patients. Occasionally, symptomatic adrenal cysts and myelolipomas could additionally be eliminated laparoscopically. Nonfunctioning adrenal lesions bigger than 4�5 cm or tumors that have shown growth in measurement on serial imaging may also be excised laparoscopically. The use of laparoscopy within the management of larger malignant masses is somewhat controversial. The lack of a real capsule around the adrenal gland tremendously increases the chance of local invasion of these extremely aggressive tumors. This makes complete excision and adherence to basic oncologic principles a tough task, even throughout open surgical approaches. In gentle of those difficulties, many surgeons advocate an open strategy to identified adrenal malignancies or for large lesions (>8 cm). In spite of those fears, there have been a quantity of reports of effective and complete laparoscopic surgical excision of malignant masses [2, 3]. Prospective, randomized managed trials are missing, nevertheless, and could additionally be gradual in coming due to the relative rarity of these tumors (0. In addition, stimulation studies, similar to low- and high-dose dexamethasone suppression exams, and plasma renin activity can be applied when acceptable. In patients with main hyperaldosteronism, spironolactone is given preoperatively. In sufferers with Cushing syndrome, serum glucose degree needs careful monitoring and glucocorticoid replacement may be needed. For sufferers with pheochromocytoma, control of blood stress and cardiac arrhythymias is crucial. This usually entails starting alpha-adrenergic blockade 2 weeks previous to surgical procedure, with the next addition of beta-blockade within the presence of arrhythmias. Some endocrinologists advocate using the tyrosine hydroxylase inhibitor metyrosine as preoperative medical blockade, but this routine can be tough to tolerate owing to unwanted effects. Contraindications General contraindications to a laparoscopic strategy embrace those sufferers with an uncorrected coagulopathy, peritonitis, intestinal obstruction, and extreme cardiopulmonary illness. However, it has to be noted that the general morbidity and mortality is independent of the scale of the tumor [8]. Although the resection of malignant pheochromocytomas by laparoscopic strategy has been reported, there are nonetheless inadequate data on the long-term follow-up of these patients [3, 7, 9, 10]. Obesity has been advised to be a relative contraindication to a laparoscopic method to the adrenal gland. While newer investigators have famous that obesity is associated with longer operating room instances and slight increases in complication charges, most authors feel that obese patients are simply managed because the surgeon gains operative expertise and advances along the learning curve [11]. Finally, significant earlier belly surgical procedure is often a relative contraindication to transperitoneal laparoscopy if adhesions are so dense as to create an unacceptably high danger of inadvertent enterotomy. In this occasion, the surgeon can go for a retroperitoneal strategy, either through a regular flank incision or through retroperitoneal laparoscopy [12]. Preoperative management A full step-by-step dialogue of the analysis of a patient with an adrenal lesion is past the scope of this chapter. Clearly, each affected person requires an assessment of any lesion from a radiologic perspective as well as a full metabolic analysis. Preoperative preparation A mechanical and antibiotic bowel preparation is given to all sufferers. This helps decompress the intestines to Chapter eighty five Laparoscopic and Robotic Adrenalectomy 1027 facilitate publicity throughout dissection and allows for conservative repair of any inadvertent bowel injury. Nitrous oxide can result in bowel distention and ought to be averted throughout this process. In addition, a nasogastric tube and urinary catheter are inserted to decompress the abdomen and bladder prior to creation of the pneumoperitoneum. As always, close intraoperative monitoring of vital signs through the utilization of invasive strains is crucial. This contains arterial strains, central traces, and large-bore catheters for speedy fluid infusion. Anesthesiologists also wants to be prepared for rapid and drastic shifts in blood pressure (intraoperative hypertension and hypotension after removal of the adrenergic lesions) and should have vasoactive medicines drawn and prepared for immediate infusion. At the end of the procedure, a specimen entrapment bag is used to retrieve the adrenal tissue. This system may be cumbersome and requires talent to maintain the mouth of the bag open while passing the specimen in to its interior. In all circumstances, open surgical devices should be available in the working room in the occasion a conversion to an open process is critical. Surgical strategies the respective merits of a transperitoneal versus a retroperitoneal laparoscopic approach to the adrenal gland have been broadly mentioned within the literature. Most surgeons acknowledge the inherent difficulties of the decreased operating space with a retroperitoneal route, but espouse the advantages that come with avoidance of the peritoneal cavity and its risk of adhesions and trocar-site hernias. Importantly, retroperitoneal entry permits for the fast mobilization and early ligation of the adrenal vein (especially on the left side). It is important to notice, nonetheless, that the retroperitoneal parts of some of these collection have been performed after the transperitoneal instances, making it difficult to differentiate between the significance of surgeon experience versus the importance of operative method. Nevertheless, there are at present no series that specifically handle the advantages of 1 approach over the other when utilized to laparoscopy of the adrenal gland. Instrumentation Standard laparoscopic equipment as described in earlier chapters is utilized in all approaches to the adrenal gland.
Safe 40 mg zeritOne affected person had a big hemorrhage requiring a 3-unit blood transfusion [160]. The supply of this prolonged drainage was not detailed additional and was said to resolve spontaneously without any described intervention. Another potential complication, not reported within the literature, which has occurred following laparoscopic diverticulectomy is a persistent urine leak or urinoma improvement in the flank (T. This results from both insufficient suture Instrumentation the instrumentation required for nephropexy is listed in Table 81. Steps of the procedure Step 1: Creation of the pneumoperitoneum and preliminary entry access this step is similar to that outlined for laparoscopic nephrectomy utilizing either the transperitoneal or retroperitoneal approach. Care should be exercised in these instances on initial entry with the Veress needle within the decrease quadrant as the kidney could be displaced in to this space in some cases of extreme mobility. Usually air-planing the desk barely away from the working surgeon will cause the kidney to roll in to a extra normal location. Step 2: Secondary port placement this step is equivalent to that outlined for laparoscopic nephrectomy utilizing both the transperitoneal or retroperitoneal strategy with the exception that solely the periumbilical port must be a 10/12-mm port to Chapter 81 Renal Surgery for Benign Disease 983 Table 81. Alternatively, the same port sizes and configuration for laparoscopic nephrectomy could be utilized for this process, permitting use of the 10-mm laparoscope if desired. Step three: Exposure of the retroperitoneum this step is equivalent to that outlined for laparoscopic nephrectomy utilizing either the transperitoneal or retroperitoneal approach. The Genzyme liver retractor is inserted by way of the lateral-most port and is utilized by the assistant surgeon to elevate the liver edge to expose the coronary ligament. Care should be exercised when transecting the infrahepatic peritoneal attachments to the liver to go away sufficient of a shelf-like edge beneath which the higher pole of the kidney may be inserted and two securing sutures to the renal capsule placed as described by Elashry et al. Appropriate positioning of the kidney within the retroperitoneum is facilitated by inserting the affected person in to a deep Trendelenburg place and air-planing the desk away from the operating surgeon. The contact region between the sting of the kidney and the retroperitoneal fat is noted and the Harmonic shears are utilized to take away the entire fat overlying this area, so the broad fascial surface of the quadratus musculature is available for suturing (see Video 81. The lack of intervening fat allows for better visualization during suture placement by way of the quadratus fascia and renal capsule, and creates better contact between the surfaces of those buildings. Differing thickness of fats bolsters can even end in poor contact factors, stress at the remaining sutures, tear outs, and subsequent failure of the process. This is very necessary when tying down the sutures on the convexity of the decrease pole. The kidney is first held in to place by the assistant and, beginning along the lateral border of the higher pole, the positioning for fascial and renal capsular suture placement is then mentally visualized and the assistant relaxes retraction of the kidney sufficient to permit higher publicity of those surfaces. The sutures are then positioned first via the quadratus fascia and then by way of the capsule of the kidney. A second suture is then positioned approximately 1� inches lower on the convexity of the kidney, and a Surgicel bolster is then positioned between the quadratus fascia on this space and the capsule of the kidney. The assistant then retracts the kidney in to its applicable place and the sutures are sequentially tied down over the bolster as described above (see Video eighty one. The course of is then repeated till the kidney is firmly fastened to the quadratus fascia. Nephropexy sutures are spaced roughly 1� inches apart, so a total of two sutures are tied down over every bolster. Each suture is cut in to a 7-inch length, which is perfect for throwing a single intracorporeal suture. The higher pole of the kidney is secured to the cut edge of the infrahepatic peritoneal edge by inserting two sutures, first through the peritoneum and then via the adjoining region of renal capsule. This step is the explanation why it is very important reduce the peritoneum low sufficient to leave an enough shelf beneath which the higher pole may be inserted and sutured. Care must be exercised to place these renal capsular sutures simply where the convexity becomes the anterior floor of the higher pole, as more posterior placement will pressure the kidney in to slight anterior rotation. While these sutures are being positioned, the patient remains within the deep Trendelenburg position with full lateral rotation to help maintain the kidney in its anatomic position. The assistant makes use of the Genzyme liver retractor to elevate the liver edge to expose this region for suture placement. The needle is handed initially from outside-to-inside via the infrahepatic peritoneal edge, and is pulled through to the appropriate size prior to passage through the capsule of the kidney to forestall sawing via this delicate structure (see Video eighty one. The needle is scythed just below the capsule for as long a size because the arc of the needle will enable. Care must be exercised to keep away from entry in to the substance of the renal parenchyma, which can lead to vigorous and protracted bleeding, making visualization in the course of the operation difficult. A second suture is then placed in identical trend approximately 1� inches medial to the primary. Prior to tying both suture, a 2-inch Surgicel bolster is placed between the capsule of the kidney and the reduce infrahepatic peritoneal edge (see Video 18. This not only aids in hemostasis, but stimulates tissue reaction and clotting between the two structures with eventual fibrous fixation. Once these sutures are placed, the operative assistant removes the Genzyme retractor and replaces it with a blunt instrument such because the irrigator�aspirator. Two sutures are positioned at a time by way of the quadratus fascia and renal capsule, and are tied over rolled Surgicel bolsters. Chapter 81 Renal Surgery for Benign Disease 985 with a preformed loop on the tip [58]. The suturemounted needle is handed initially by way of the capsule of the kidney, then via the quadratus fascia, and the needle is introduced via the loop to allow cinching in to place. The cephalad-to-caudal method for suture placement and securing of the kidney permits fixation to occur first within the areas of least tension and proceeds toward the realm of most rigidity within the lower pole. Previously, an absorbable Polyglactin mesh had been utilized for his or her initial six patients; nonetheless, this was ultimately deserted after a affected person developed symptomatic recurrent mobility three months following surgical procedure [59]. Step 6: Exiting the stomach and port closure After tying the final suture, the operating table is returned to its neutral place and the kidney is visually monitored to be sure that it maintains its mounted place within the retroperitoneum. Final inspection of the areas of dissection for hemostasis, exiting the abdomen, and port website closure are then carried out in equivalent fashion to that described for laparoscopic nephrectomy. The patient is usually discharged residence on postoperative day 1 or 2 and is instructed to refrain from all "vertical jarring" actions such as jogging, horseback riding, and so on. Results the long-term results of four of the larger published sequence of laparoscopic nephropexy (Table 81. A comparison of 23 laparoscopic to 12 prior open nephropexy procedures performed at a single institution demonstrated only slightly longer mean operative time of sixty one min versus forty nine min, however reductions of postoperative ache medication (15 mg vs 38 mg morphine equivalent), imply hospital keep (3. Postoperative care the immediate postoperative look after sufferers having undergone nephropexy is similar to that described following laparoscopic easy nephrectomy, with the next exceptions. The affected person is usually stored in a supine place in a single day to prevent rigidity at the securing sutures and to allow clotting to begin in the area of the Surgicel bolsters. Postoperative immobilization following open nephropexy procedures has ranged from 1. Ambulation is initiated the following day and as soon as the affected person has demonstrated steady mobility, the Foley catheter is eliminated. If bowel sounds are present, the food plan can often be advanced rapidly because of the restricted mobilization of the bowel. Another potential risk when utilizing a permanent mesh would be the danger of 986 Section 6 Laparoscopy and Robotic Surgery: Laparoscopy and Robotics in Adults Table eighty one.
Order zerit 40 mg overnight deliveryThis might be defined by the widespread use of a guiding cannula for renal biopsy [23, 47]. An arteriovenous fistula ought to be thought-about in instances of persistent bleeding [49]. When the renal biopsy is carried out by a posterior method, pneumothorax has been reported in 14�29% of cases, though clinically significant pneumothorax is uncommon (<1%) [44, 48]. To additional minimize the risk of a pneumothorax, the puncture should be carried out in expiration and the needle ought to be positioned subcostally. Some higher pole tumors may be punctured utilizing the paravertebral approach, which includes the injection of saline in the paravertebral area to displace the pleura laterally [50]. Although no statistical comparability was out there, these figures counsel an bettering trend within the diagnostic efficiency of the biopsy. Biopsy failures outlined as "the lack to acquire an amount of tissue adequate for diagnosis" had been excluded from the accuracy evaluation. Consequently, in clinical apply, the physician has to remember that diagnostic yield is different from accuracy, as the biopsy failures accounted still for 9% and 5. The sum of technical failures plus indeterminate biopsies ("no definitive prognosis possible using the obtainable strategies") was 19% and 10% within the respective durations. In abstract, biopsy has a excessive accuracy within the trendy period, however nondiagnostic biopsies nonetheless account for an general 10% in general sequence no matter the tumor dimension. When considering these outcomes, some limitations of the evaluation, most of which have been identified by the authors, have to be talked about. First, the research included in this evaluation in contrast the biopsy outcomes to numerous different gold standards. These index tests varied from pathologic examination of the specimen after surgical excision to radiologic follow-up of nonextirpated tumors [7]. For instance, within the interval earlier than 2001, surgery and consequently surgical specimen obtainable for comparison was famous in only 49. The variety of instances with surgical specimen out there for comparison increased to 54% in the second research period. Third, heterogeneity amongst collection in both durations when it comes to selection standards, technical issues. All the above talked about causes could also be sources of bias in the interpretation of the analysis, and overestimation Results From the 1970s onwards, many studies have been carried out on the diagnostic accuracy of renal mass biopsy. They divided the research chronologically between those carried out before and from 2001 onwards. Before 2001, 27 research have been thought-about, in two of which "ex vivo" tumor biopsy was carried out. These outcomes are clearly inadequate to justify the systematic use of percutaneous biopsy within the diagnostic setting. However, comparison with trendy knowledge is precluded as different needles, mostly 21G and 22G, were used, and in two of those studies biopsy was guided by old ultrasound devices. After 2001, solely three extra reviews can be found in the literature during which the percutaneous renal mass biopsy has been compared in all circumstances with the surgical specimen [54, 59, 60] (Table a hundred and ten. The sensitivity of percutaneous core biopsy to detect malignancy confirmed at surgical specimen varies from ninety one. The fee of nondiagnostic biopsies was very low in these three fashionable research, in the range of 2. In an try and clarify the outcomes, we additional examined these collection the place pathologic affirmation was obtained in the type of a surgical specimen in 100% of instances, whether or not ex vivo or in the clinical setting, including with a preoperative percutaneous biopsy. Results of biopsy of small renal plenty are also considered individually, as results from general series is in all probability not extrapolatable to these lots. Ex vivo biopsies Several research have evaluated the accuracy of the ex vivo (in bench) biopsy for the diagnosis of renal tumors [6, 20, 21, 30, 31, forty one, forty two, 54, 55]. The accuracy of surgical excision (nephrectomy or partial nephrectomy) biopsies taken underneath direct vision were compared to the definitive pathologic diagnostic of the surgical specimen in 100 percent of the cases. In many of the studies pathologists evaluating the biopsy have been blinded to the definitive histopathologic results. The fee of nondiagnostic biopsies various from 2% to 20% with a trend to be greater than in the trendy percutaneous biopsy research [22]. This fact may be explained by the lack of visualization of the entire tumor, as can happen throughout imaging or within the absence of needle stabilization during percutaneous puncture. When deciphering the outcomes of in-bench biopsy research, it has to be taken in to account that this ex vivo setting is just partially comparable to scientific apply, the place percutaneous biopsies will be the commonplace. A fee of biopsy failure as high as 37% has been reported in renal plenty smaller than three cm versus 9% in tumors larger than three cm [52]. The fee of nondiagnostic biopsies can also be Percutaneous biopsy compared with 100% surgical specimens the variety of research on the accuracy of percutaneous renal mass biopsy based mostly on 100% comparability of the Chapter 110 Renal Mass Biopsy 1335 Table a hundred and ten. Fuhrman nuclear grade was correct in 68%, with a lower concordance than for subtype (60�100%), as was the case in larger renal plenty [62�64]. The fee of nondiagnostic biopsy varies from 0% to 23% in these collection of percutaneous ablation [71�74] and from 0% to 30% when tumor biopsy is carried out throughout laparoscopic ablation [75�80]. At least throughout laparoscopy-assisted ablation, modification of the biopsy method, by activating the firing mechanism of the biopsy gun externally to the target tissue, led to a higher diagnostic yield in a small scientific series [77]. The criteria classifying a biopsy as nondiagnostic or benign varies between groups, which may explain the broad range of nondiagnostic or benign results. As an instance, regular renal tissue, fibrotic tissue or necrotic tissue are distinctly classed as benign by some and nondiagnostic by others [78, 80]. In reality, the stricter the nondiagnostic standards are, the higher the nondiagnostic price of the biopsy. Tumor biopsies can be taken instantly after ablation to decrease risk of bleeding or tract seeding. Success after ablation remedy is especially decided utilizing cross-sectional imaging with distinction. Therefore, some centers have performed an extra postablation biopsy to assess the success of the ablation. The 6-months postcryoablation biopsy was persistently negative in all nonenhancing masses. The results for cryoablation were superior, with a sensitivity and specificity of seventy seven. However, in the fashionable sequence an total accuracy of 94% in identifying the correct histologic subtype was reported [22]. This concern remains a problem for the pathologist, especially when limited tissue is available, as is the case with biopsies. In all of the discordant cases, the actual grade found in postoperative pathology was within one grade of the grade discovered at biopsy. This info has not solely diagnostic functions but may impact follow-up policy.
Diseases - Howel Evans syndrome
- Radiation induced meningioma
- Chromosome 7, partial monosomy 7p
- Trisomy 12 mosaicism
- Fish poisoning
- Ectrodactyly recessive form
- M?bius axonal neuropathy hypogonadism
- Occlusive Infantile ateriopathy
- Cyclic neutropenia
Cheap zerit master cardThe continued contact of urine with the vulva from diapers used to include the identical causes excoriation of the pores and skin and vulvitis. The constant dribble of urine emanates unhealthy odor and the affected person becomes a social outcast. Some patients are divorced by their husbands as a result of their inability to have a wholesome sexual relationship. Socially, 45% of the ladies interviewed felt ostracized and 50% have been economically impoverished by job loss consequent to their growing the fistula. Therefore, psychologic assist and sometimes pharmacotherapy turn into essential earlier than embarking on definitive surgical procedure. A urine sample for tradition should be obtained using a catheter inserted by way of the urethra or a sterile speculum inserted in the vagina. Any indwelling catheter should be eliminated and tissue edema must be allowed to subside completely, particularly in fistulas occurring after delivery. Improving the overall situation and diet of the affected person, correcting anemia, and treating vulval excoriations are important features for good therapeutic after surgery. In patients in a hypoestrogenic state, topical software of estrogen lotions for a couple of weeks may improve the quality of vaginal tissues. Preoperative evaluation the affected person usually presents with incontinence of urine that usually follows supply or pelvic surgical procedure. Usually the affected person stories leakage of urine instantly after removing of the catheter following the surgery or obstetric event, but the leakage can begin after several days or perhaps a few weeks later. Sometimes, particularly in the presence of an isolated ureterovaginal fistula or a small excessive vesicovaginal fistula, the affected person might have a standard voiding pattern along with steady incontinence. Digital vaginal examination helps to determine the fistula and to rule out coexisting pathologies in the pelvis. It additionally helps assess the accessibility of the fistula for reconstruction by way of the vagina, extent of fibrosis and related scarring, and quality of vaginal tissue. A per speculum vaginal examination is needed to precisely identify the presence, number, and site of the fistula. The three-tampon take a look at described by Moir helps distinguish a vesicovaginal fistula from a ureterovaginal fistula [2]. Cystoscopy is necessary in each case to assess the variety of fistulas, and their size, location, and relationship to the ureteral orifices and bladder neck. It also helps assess the bladder capability, detect any calculus or foreign body such as suture material, and the presence of any irritation of the bladder mucosa. A biopsy of the fistula could also be essential in instances treated earlier for gynecologic malignancies to rule out presence of cancer. Twelve % of vesicovaginal fistulas may be related to ureteral abnormalities [3]. In case of suspected ureterovaginal fistula or a distal ureteral stricture on imaging, a retrograde ureteropyelo- Classification of vesicovaginal fistulas Vesicovaginal fistulas can be classified as simple or complex. The following fistulas are thought of as advanced: � Large fistulas; � Fistulas involving the ureteric orifice, bladder neck or urethra; � Previous failed repairs; � Postradiotherapy fistulas; � Underlying malignancy or granulomatous infections. Based on their anatomic location, fistulas can be categorised as trigonal or supratrigonal, as seen on cystoscopy, and juxtacervical, high vaginal or mid-vaginal based on the anatomic location on the anterior vaginal wall. Treatment choices for vesicovaginal fistula repair A interval of conservative administration by extended catheterization for 4�6 weeks may be attempted in fistulas following hysterectomy, but solely small fistulas are likely to heal. A determination to begin conservative administration have to be weighed towards the good results of early repair, particularly in posthysterectomy fistulas. Minimally invasive methods like fulguration of the fistula tract are successful only in a small proportion of cases with small fistulas. There are a quantity of anecdotal reports indicating profitable use of biologic sealants like fibrin glue and cyanoacrylic glue for small vesicovaginal fistulas lower than 1 cm [4, 5]. Medical administration of those fistulas has been attempted with long-acting gonadotrophin-releasing hormone analogs to induce reversible menopause with some success [6, 7]. However, 1070 Section 6 Laparoscopy and Robotic Surgery: Laparoscopy and Robotics in Adults strains, interposition of vascularized tissue (omentum, peritoneum or Martius flap), and sufficient postoperative bladder drainage. In case the ureteral orifice is concerned or within the presence of a coexistent ureterovaginal fistula or stricture, ureteral reimplantation is required. Attention should also be paid to the continence mechanism when the fistula entails the urethra or bladder neck or where the bladder capability is compromised. With the high success rate associated with surgical repairs, consideration must even be given to sustaining the vaginal luminal measurement during reconstruction to retain sexual function [13]. Continence procedures, like a pubovaginal sling in circumstances of in depth urethral involvement, augmentation cystoplasty for a small bladder, or vaginoplasty for vaginal stenosis, could also be required in choose cases. A few ureterovaginal (or ureterouterine) fistulas with a patent distal ureter may be amenable to endourologic management by endoscopic ureteral stenting [8]. In the presence of active infection and sepsis, a interval of antibiotic therapy and urinary diversion within the type of a percutaneous nephrostomy on the affected side could additionally be important to control an infection earlier than contemplating definitive reconstruction. Timing of surgical procedure for vesicovaginal fistula Traditionally, a waiting period of 3 months or extra after the antecedent occasion has been adopted before embarking on fistula repair. The advantages of early restore are obvious and embody shortening of the duration of morbidity and psychosocial stress brought on by urinary incontinence, and reduction in the worth of managing incontinence. Several stories have shown that fistula repair may be performed within 6 weeks with safety and efficacy [9, 10]. This may be justified because the extent of trauma to the bladder and the vagina is troublesome to assess at the time of the occasion. Nevertheless, it might be famous that a big sequence from Nigeria has reported a high success fee with early restore even in obstetric fistulas [12]. Surgical approaches to repair and indications for an stomach strategy Surgical restore of a vesicovaginal fistula may be performed through the vaginal or abdominal routes. The absolute indications for an abdominal approach are when the vesicovaginal fistula is associated with: � Involvement of the ureteral orifice by the fistula; � A small capability bladder requiring augmentation; � Vaginal stenosis from postsurgical scarring or previous radiation; � Involvement of the cervix or uterus; � Coexistent ureterovaginal fistula or ureteral stricture requiring ureteral reimplantation. Vesicouterine or vesicocervical fistulas can only be repaired through the stomach route. A massive supratrigonal vesicovaginal fistula or a previously failed vaginal restore are relative indications for belly repair. The advantages of the vaginal strategy include less postoperative pain, less postoperative ileus, avoidance of the complications of a laparotomy, and better cosmesis. Recently, laparoscopic and robot-assisted laparoscopic methods have been used to lower the morbidity of an abdominal restore of a vesicovaginal fistula. These methods have some great advantages of decreasing the morbidity of surgical procedure by lowering postoperative pain, early resumption of feeding, early ambulation, shorter hospital keep, and higher cosmesis as compared to open surgery. These techniques are challenging and there exists a steep learning curve, especially for the purely laparoscopic method. Robotic help thus tremendously facilitates laparoscopic restore of vesicovaginal fistula. Operating strategy of robot-assisted laparoscopic restore of a vesicovaginal fistula the procedure is carried out underneath basic anesthesia.
Purchase cheap zerit on lineLocating these calculi can be tough because the vertebrae may act as an impediment and there may be related vertebral anomalies in some sufferers. Prone position and "blast path" could need to be used to goal these awkwardly positioned calculi [13]. A better stone-free end result can be achieved when a second-generation lithotripter is used [11]. It is necessary to emphasize that there have been no prospective research comparing the different treatment modalities in this group of sufferers. Renal colic, 704 Section 5 Stone Management in Urology: Management of Stones in Abnormal Situations delicate hematuria, and urinary tract infection are considered gentle and could also be handled conservatively and medically. The renal pelvis is ventrally orientated and typically, the decrease poles are related by isthmus which may be fibrous or viable renal tissue. The long axis of the kidney is orientated within the sagittal aircraft, such that the posterior calyces are oriented dorsomedially and the frontal row factors dorsolaterally. Thirty % of horseshoe kidneys have a single renal artery on both side [15], but the blood supply is variable with accessory vessels arising from any a half of the belly aorta, bifurcation or iliac arteries, and inserting in to the renal hilum. Taking all the above anatomic options in to consideration, percutaneous access of horseshoe kidney is comparatively safe and is usually approached via the most superior calyx. Inadvertent harm to the pleura is rare with an upper pole puncture in a low-lying horseshoe kidney. The posterior calyx is comparatively easily accessible with a direct puncture in a dorsoventral direction and the puncture site extra medially situated in comparability to a usually oriented kidney. The primary principle of achieving an atraumatic puncture of the renal calyx must be adhered to if potential, whatever the modality used. However, the superior calyx is often the chosen puncture web site for staghorn calculi or stones inside a quantity of calyces. Ultrasound can be used to guide puncture in to the superior calyx if the accumulating system is hydronephrotic or predilated with fluid/contrast retrogradely. However, the lower pole can additionally be typically poorly delineated and as a consequence, the view of the calyx may be suboptimal to guide entry puncture [17]. After putting a ureteric catheter, the patient is then turned in to the inclined position with the C-arm positioned vertically. The pelvicalyceal system is distended with distinction and the C-arm may be rotated +30� to -30� to evaluate the calyceal anatomy. When the needle is transferring with respiration, the C-arm is then rotated obliquely to an angle such that the size of the needle is visualized and the needle is advanced beneath fluoroscopic steerage. The needle ought to be advanced ideally to puncture the epicenter of the calyx and the needle tract must be in the orientation of the infundibulum. As the tract may be longer for horseshoe kidneys, longer devices could also be necessary. As the decrease pole and pelvis are more anteriorly dealing with than is usual, a regular lower pole lateral entry may damage the big anterior division arteries or accent branches from the iliac artery [18]. A rigid nephroscope is used to take away the calculi, using both an ultrasonic or lithoclast lithotripter to disintegrate the stones. Stones may be eliminated sequentially via the tract with varied stone-grasping gadgets. This is then clamped and if the affected person is asymptomatic, the nephrostomy is be eliminated on the ward. Retrorenal or posterolateral displacement of the bowel can be related to horseshoe kidney and the bowel could occasionally act as an obstacle to percutaneous entry. It is paramount on this case that the patient can tolerate a prolonged prone place. Once access is obtained, a nephrostomy tube may be left in situ for subsequent entry and the tract can be dilated as described above under common anesthesia. Extracorporeal shock wave lithotripsy in anomalous kidneys: 11-year expertise with two second-generation lithotripters. Risk elements for the formation of a steinstrasse after extracorporeal shock wave lithotripsy: a statistical mannequin. Horseshoe kidney: Does it actually have any negative impact on surgical outcomes of percutaneous nephrolithotomy Ureteroscopy Retrograde digital flexible ureteroscopy is becoming a extra regularly used modality, especially for stones less than 15 mm in diameter utilizing the holmium laser for stone disintegration. However, reported case numbers are small and retrospective, and there may be points referring to ureteric access requiring prestenting. These instances will typically require use of an entry sheath and postoperative stent insertion. To date, such cases have typically been managed in specialist stone centers that can supply the complete range of a stone administration service [20]. Determining the incidence of horseshoe kidney from radiographic data at a single establishment. Kidney fusion anomalies revisited: medical and radiological analysis of 209 circumstances of crossed fused ectopia and horseshoe kidney. Horseshoe kidney: a new concept on its embryogenesis based mostly on the study of a 16-mm human embryo. Vesicoureteral reflux and ureteropelvic junction obstruction in youngsters with horseshoe kidney: therapy and end result. Given the rarity of a pelvic kidney, it often is an unsuspected finding in sufferers presenting with imprecise or atypical belly symptoms. Only on further evaluation with radiographic examination is an ectopic kidney recognized because the trigger [2]. Because of structural and architectural anomalies that can accompany a pelvic kidney, situations such as chronic obstruction and nephrolithiasis are frequent. The variation in anatomy of a pelvic kidney creates anomalous vascular patterns and altered spatial relations with adjoining pelvic organs. Blood vessels which are not able to reach the migrating kidney will degenerate. A pelvic kidney lies posterior to the peritoneum, anterior to the sacrum, and caudal to the aortic bifurcation. Hypotheses embody abnormalities of the ureteral bud and metanephric blastema, genetic variants, teratogenic effects, and anomalous vasculature physically blocking ascent [4]. Nephrolithiasis Renal growth During weeks 6 and 9 of human improvement, the kidney ascends from a pelvic place to the lumbar region in a site just inferior to the adrenal glands. As the kidney migrates cephalad, the ectopic kidney is thought to be no extra prone to illness than the usually positioned kidney, except for the presence of calculi and hydronephrosis [3]. A horseshoe kidney has a 20% reported incidence of associated calculi; nonetheless, the incidence of stones in pelvic kidneys has not been established [5]. While renal calculi in horseshoe kidneys have demonstrated metabolic abnormalities predisposing to stone formation, similar to hypovolemia, hypercalcuria, and hypocitraturia, no obtainable research have specifically analyzed metabolic abnormalities in renal calculi of pelvic kidneys [5]. It is the anterior position of the renal pelvis, malrotation of the kidney, high insertion of the ureter, anomalous renal vasculature, or a combination of those elements that can impair the drainage of urine and partially hinder the pelvic kidney. Although the pelvic kidney is situated within the retroperitoneum, loops of bowel lie between the anterior stomach wall and the kidney.
Order zerit discountA rightangled dissector or other dissecting forceps can be useful for this function. Care should be taken throughout withdrawal of the applier as the utilized clip may be pulled again and out of position if undue traction is inadvertently transferred to the clip. If a clip is misplaced, Maryland or DeBakey forceps could additionally be used to slowly take away it by backing it straight off the clipped vessel or tissue. For smaller vessels, sometimes one to two clips are used on both the proximal and distal sides of the area to be divided. Surgical clips Laparoscopic clip appliers are available and routinely used for many laparoscopic procedures requiring the ligation of small veins, arteries or lymphatics. There are two primary categories of clip supplies used in the laparoscopic setting: titanium and nonabsorbable polymer. Instrumentation and software of titanium clips Titanium clips can be found in both straight and rightangled variations and are sometimes disposable, multiple load, single-use units carrying between 15 and 30 clips per instrument. The advantages of those gadgets lie of their capacity to allow for rapid application of a quantity of clips without the necessity to cross the instrument out and in of a trocar. This both decreases the time involved in vessel ligation and eliminates the potential for dislodging a clip on pass-through of the trocar valve. Closure of the clips occurs from distal to proximal, which helps stop the desired vessel from being pushed forward and out of the apposing arms of the partaking clip because the jaws close. The titanium clips themselves are also sometimes textured along the inner floor with ridges and depressions to decrease the chance of becoming dislodged as a result of either subsequent dissection following ligation or arterial pressure inside the ligated vessel. A rotational capability of 360� allows for ergonomic hand positioning, translating in to ease of use and improved accuracy of clip placement. Some clip appliers also reload clips through an computerized mechanism, eliminating a step within the application of a number of clips in rapid succession. When utilizing titanium clips to ligate larger vessels, corresponding to the principle renal artery, three to 5 clips should be used on the proximal aspect prior to division (courtesy of SurgiQuest Inc. These clips incorporate a locking mechanism such that the tips of the two arms can engage and lock through multiple tissue layers. This mechanism provides tactile suggestions such that the surgeon can sense if the clip has correctly engaged by feeling the transmitted clip closure by way of the laparoscopic applier. Even with the usage of a purpose-built Hem-o-lok clip remover that helps disengage the locking mechanism, clip removal is often a problem. Similar to the titanium clip appliers, the Hem-o-lok clip appliers also have 360� rotational capacity. This often results in a clip changing into dislodged when passing in to a trocar or through the abdominal cavity. After the stapler is fired, a blade cuts between the 2 sets of staples to divide the ligated tissue. Linear surgical staplers Laparoscopic stapling units can be used for a massive number of functions. They allow for speedy ligation with or without division of tissues by deploying a number of parallel rows of metallic staples laid in a brick-like intercalated pattern to enable overlap from one row to the following. Cutting devices typically use two units of three parallel rows of staples and divide the ligated tissue between them. As their name suggests, vascular loads are excellent for ligation of vascular pedicles, such as the renal hilum during nephrectomy or bladder pedicles during cystectomy. The medium and enormous loads are helpful for securing thicker buildings corresponding to bladder or bowel. All staplers supply 360� rotation and heaps of can be found with both a straight or articulating head. The articulating head can offer a higher vary of motion and variety in angle of utility from a fixed trocar web site. Before using a laparoscopic stapling device, several elements have to be taken in to consideration. First, most staplers require a 12-mm port measurement in order to be safely handed in to the stomach, and the jaws ought to be closed when introducing and withdrawing the instrument. To avoid premature deployment of the staples or chopping blade, all stapling units incorporate a security mechanism that have to be disengaged prior to firing. The goal tissue must also be appropriately dissected free of surrounding connective tissue, of suitable thickness, and accessible to permit the arms of the staplers to be positioned precisely, with tips seen, and closed with out requiring undue pressure. Reports of stapler misfire have appeared in the literature with a malfunction incidence of approximately 1. However, many of those issues had been attributed to misuse of the gadget quite than tools failure. The surgeon should always be ready for this rare complication to keep away from excessive blood loss or conversion to an open surgical method. While this strategy provides a further step, it provides very little time to the overall operation. Doing so might end in both incomplete ligation or avulsion of the target vessel because the staples are fired. After firing the system, the jaws should be reopened previous to withdrawing the device from the target area, and the staple line may be inspected to guarantee an intact ligation and hemostasis. In some situations, a further reload could additionally be required to complete the pedicle ligation. The jaws of the reload could also be closed to incorporate and overlap the unique staple line if essential without compromising the flexibility of the gadget to hearth and reduce. Minimizing the variety of clips in an area where the utilization of a laparoscopic stapler may be anticipated (such because the renal hilum) will lessen the possibility of encountering issue with clips when maneuvering the stapler in to place. Comparison of laparoscopic performance in vivo with performance measured in a laparoscopic simulator. Laparoscopic coaching on bench models: higher and more price effective than operating room experience Initial laparoscopic primary expertise coaching shortens the learning curve of laparoscopic suturing and is cost-effective. Future directions the instruments for laparoscopic reconstruction have improved dramatically over the past 20 years and will surely proceed to turn into increasingly ergonomic and refined with time. While robotic surgical procedure has launched wristed devices in to the minimally invasive area, these tools are additionally starting to be used more frequently in the pure laparoscopic surroundings. Single-site surgery has demonstrated the potential of intracorporeal triangulation and could additionally be one other step on the path toward further discount of surgical morbidity. All successful urologic laparoscopy starts with the establishment of pneumoperitoneum, adopted by main and secondary trocar placement. This chapter will address strategies for each closed and open peritoneal access, anterior belly wall anatomy, common issues, method, and rationale for secondary trocar configuration and issues. Anterior abdominal wall anatomy A thorough knowledge of the anterior abdominal wall anatomy is crucial for secondary trocar placement. This will decrease the potential for vascular harm, hernia formation, or loss of entry. The abdominal wall muscles are organized in to two separate groups: anterolateral and posterior. The anterolateral group of stomach muscle tissue is split in to two subgroups primarily based on the orientation of the muscle fibers.
Order zerit 40mg fast deliveryEffect of prolonged pneumoperitoneum on intraoperative urine output throughout laparoscopic gastric bypass. A potential randomized comparison of the metabolic and stress hormonal responses of laparoscopic and open cholecystectomy. Preoperative dexamethasone improves surgical end result after laparoscopic cholecystectomy: A randomized double-blind placebo-controlled trial. Residual pneumoperitoneum: A cause of postoperative ache after laparoscopic cholecystectomy. Nonsteroidal antiinflammatory medicine for postoperative pain administration after lumbar spine surgical procedure: a meta-analysis of randomized managed trials. Gabapentin and postoperative pain-a systematic evaluation of randomized managed trials. Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. Small dose ketamine infusion improves postoperative analgesia and rehabilitation after total knee arthroplasty. Intraoperative small dose ketamine enhances analgesia after outpatient knee arthroscopy. Intraoperative infusion of dexmedetomidine reduces perioperative analgesic necessities. The impact of pre-anesthetic administration of intravenous dexmedetomidine on postoperative pain in patients receiving patient-controlled morphine. Positive endexpiratory pressure improves respiratory perform in overweight however not in normal topics throughout anesthesia and paralysis. Rhabdomyolysis of gluteal muscular tissues leading to renal failure: A doubtlessly fatal complication of surgery in the morbidly obese. Changes in pulmonary mechanics during laparoscopic gastroplasty in morbidly obese sufferers. Comparison of pulmonary operate and postoperative ache after laparoscopic versus open gastric bypass: a randomized trial. Pain after laparoscopic cholecystectomy: Characteristics and effect of intraperitoneal bupivacaine. Chapter 69 Anesthetic Considerations throughout Laparoscopic and Robotic Surgery 809 131. Dexmedetomidine improves postoperative ache administration in bariatric surgical patients. Local anesthetic infiltration for postoperative pain relief after laparoscopy: A qualitative and quantitative systematic evaluation of intraperitoneal, port-site infiltration and mesosalpinx block. Pain after laparoscopic cholecystectomy: the effect and timing of incisional and intraperitoneal bupivacaine. The scientific efficacy and pharmacokinetics of intraperitoneal ropivacaine for laparoscopic cholecystectomy. Preventing postoperative ache by native anesthetic instillation after laparoscopic gynecologic surgery: A placebo-controlled comparability of bupivacaine and ropivacaine. Prevention of postoperative nausea and vomiting � a multimodal resolution to a persistent drawback. Postoperative nausea and vomiting after discharge from outpatient surgical procedure facilities. Patient satisfaction after anesthesia and surgery: outcomes ofa potential survey of 10,811 patients. Massive subcutaneous emphysema and sudden airway compromise after postoperative vomiting. Subcutaneous emphysema following severe vomiting after rising from basic anesthesia. A simplified risk rating for predicting postoperative nausea and vomiting:conclusions from cross-validations between two centers. Volatile anaesthetics could also be the primary trigger for early but not delayed postoperative vomiting: a randomized managed trial of factorial design. Omitting antagonism of neuromuscular block: impact on postoperative nausea and vomiting and risk of residual paralysis. Efficacy, doseresponse, and adverse results of droperidol for prevention of postoperative nausea and vomiting. Low dose haloperidol prevents postoperative nausea and vomiting after ambulatory laparoscopic surgical procedure. Incidence and severity of postoperative nausea and vomiting are comparable after metoclopramide 20 mg and ondansetron eight mg given by the top of laparoscopic cholecystectomies. Ondansetron/ promethazine mixture or promethazine alone reduces nausea and vomiting after middle ear surgery. Comment: promethazine opposed occasions after implementation of a medicine shortage interchange. The effect of timing of dexamethasone administration on its efficacy as a prophylactic antiemetic for postoperative nausea and vomiting. Propofol anaesthesia and postoperative nausea and vomiting:a quantitative systematic evaluate of randomized controlled studies. A prospective randomized double-blinded study of the effect of intravenous fluid therapy on adverse outcomes on outpatient surgery. Recovery after propofol with and without intraoperative fentanyl in patients present process ambulatory gynecologic laparoscopy. The use of nonpharmacologic techniques to prevent postoperative nausea and vomiting: a meta-analysis. A surgical safety checklist to reduce morbidity and mortality in international inhabitants, N Eng J Med 2009:360:491�499. The efficacy and safety of transdermal scopolamine for the prevention of postoperative nausea and vomiting:a quantitative systematic evaluation. Patient-tailored antiemetic remedy with 5-hydroxytryptamine sort three receptor antagonists based on cytochrome P-450 2D6 genotypes. As such, these procedures had been sometimes quick in period, associated with minimal morbidity, and most commonly performed in wholesome, younger females. With the introduction of the laparoscopic cholecystectomy in 1990 and nephrectomy in 1991, the removing of larger stable organs became feasible and laparoscopy advanced from the realm of diagnostic to therapeutic procedures [2, 3]. Since that point, the skill and instrumentation of the laparoscopic surgeon has significantly expanded, which in turn has increased the complexity and period of these procedures. Modern day laparoscopic and robotic surgeries address a broad spectrum of pathologic circumstances in sufferers with diversified states of health. As a consequence, the impression of prolonged pneumoperitoneum has turn out to be a central issue for these patients both throughout and following surgical procedures. This chapter addresses the physiologic results of pneumoperitoneum and the potential problems arising from it. Insufflation brokers Early in the evolution of laparoscopy, pneumoperitoneum was established using either room air or oxygen [4]. However, the potential for important opposed sequelae referring to venous air embolism, intra-abdominal explosion, and combustion with oxygen and room air soon terminated their roles in a medical setting. The consensus among laparoscopic surgeons was that the ideal insufflation agent ought to be readily available, inexpensive, noncombustible in nature, and rapidly soluble in plasma [5].
References - Klaus E, Englert H, Hropot M, et al: K+-channel openers inhibit the KCl-induced phasic-rhythmic contractions in the upper urinary tract, Eur J Pharmacol 183:673, 1990.
- Tatar B, Oksay T, Selcen Cebe F, et al: Management of vesicovaginal fistulas after gynecologic surgery, Turk J Obstet Gynecol 14(1):45n51, 2017.
- Mimori T, Yoshitaka I, Nakashima R, Yoshifuji H. Autoantibodies in idiopathic infl ammatory myopathy: an update on clinical and pathophysiological signifi cance. Curr Opin Rheum 2007; 19: 523n9. Neri R, Mosca M, Stampacchia G, et al. Functional and isokinetic assessment of muscle strength in patients with idiopathic infl ammatory myopathies. Autoimmunity 2006; 39(3): 255n9. Noss EH, Hausner-Sypeck Dl, Weinblatt ME. Rituximab as therapy for refractory polymyositis and dermatomyositis. J Rheumatol 2006; 33: 1021n6. Saito E, Koike T, Hashimoto H, et al. Effi cacy of high dose intravenous immune globulin therapy in Japanese patients with steroid resistant polymyositis and dermatomyositis. Mod Rheum 2008; 18: 34n44.
- Lieberman PH et al: Evaluation of malignant lymphomas using three classifications and the Working Formulations. Am J Med 81: 365, 1986.
- Stott DJ, Falconer A, Miller H, et al: Urinary tract infection after stroke, QJM 102:243n249, 2009.
|
|