"Buy quetiapine 50 mg overnight delivery, 97140 treatment code."By: Danielle Marie Brander, MD - Assistant Professor of Medicine
- Member of the Duke Cancer Institute
 https://medicine.duke.edu/faculty/danielle-marie-brander-md
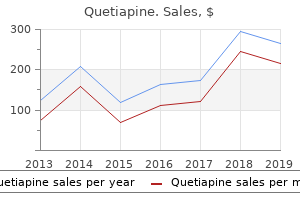
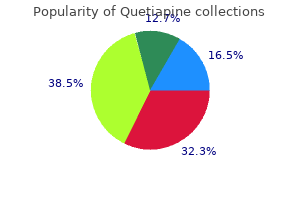
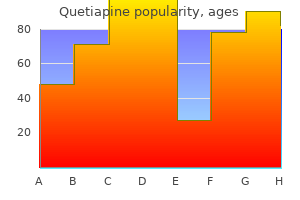
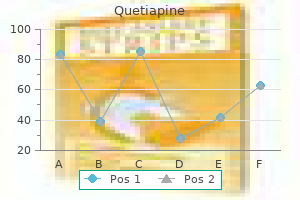
Discount 200mg quetiapine mastercardDoes lamotrigine use in being pregnant increase orofacial cleft threat relative to different malformations? A study displaying an affiliation between in utero publicity to gastric acidsuppressing medication and childhood allergy and asthma requires confirmation. Most likely, the observed defects were the result of many elements, together with presumably the severity of the disease and concurrent use of different medication. In addition, the studies lacked the sensitivity to detect minor anomalies because of the absence of standardized examinations. Late-appearing main defects may also have been missed due to the timing of some data collection. If lansoprazole is required or if inadvertent exposure does occur early in gestation, the identified threat to the embryofetus appears to be low. It is also utilized in combination with amoxicillin and/or clarithromycin for Helicobacter pylori eradication to scale back the danger of duodenal ulcer recurrence. In addition, constructive results have been seen with lansoprazole in the in vitro human lymphocyte chromosomal aberration assays, however the Ames mutation assay and different genotoxic animal checks have been negative (1). In a research printed in 1990, lansoprazole at a dose of fifty or 300 mg/kg was not teratogenic in pregnant rats, however a decrease in fetal weight occurred (2). Schardein additionally cited a 1990 research, which seems to be much like the one cited above, that discovered no evidence of teratogenicity in rats and rabbits (3). The molecular weight (about 369) is low sufficient that passage to the fetus should be expected. A 1998 noninterventional, observational cohort examine described the outcomes of pregnancies in ladies who had been prescribed 1 of 34 newly marketed drugs by common practitioners in England (4). In 831 (78%) of the pregnancies, a newly marketed drug was thought to have been taken during the 1st trimester, with birth defects famous in 14 (2. Two of those infants had delivery defects: an atrial septum defect and an undescended testicle (see Omeprazole for added particulars of this examine (5). In comparability with controls, the adjusted (for maternal age, start order, gestational age, and smoking, however not for alcohol abuse) relative dangers for the three outcomes had been congenital malformations 1. A 2005 study by the European Network of Teratology Information Services reported the outcomes of pregnancies exposed to omeprazole (N = 295), lansoprazole (N = 62), or pantoprazole (N = 53) (8). In the pantoprazole group, the median duration of remedy was 14 days (range 723 days) and the dose used was forty mg/day. One infant exposed early in gestation (week 2 for 8 days) had congenital toxoplasmosis. A 2007 case report described the use of lansoprazole in a lady with Zollinger-Ellison syndrome (9). In the first trimester, she underwent a left lobectomy of the liver to remove a gastrin-secreting neuroendocrine tumor. Ultrasound scans revealed a single umbilical artery and bilateral choroid plexus cysts with no other malformations. At the time of the report, the girl was in her second being pregnant and receiving the same oral remedy (9). A population-based observational cohort study shaped by linking knowledge from three Swedish nationwide healthcare registers over a 10-year interval (19952004) was reported in 2009 (10). The authors proposed three potential mechanisms for his or her findings: (a) exposure to increased amounts of allergens could trigger sensitization to digestion-labile antigens within the fetus; (b) maternal Th2 cytokine pattern might promote an allergy-prone phenotype in the fetus; and (c) maternal allergen-specific IgE might cross the placenta and sensitize fetal immune cells to food- and airborne allergens. Several limitations of the examine that might have affected their findings have been identified, including a basic improve in childhood asthma however not necessarily an increase in allergic asthma (10). An accompanying editorial mentioned the strengths and weaknesses of the research (13). A massive retrospective cohort research from Israel masking 19982009 was published in 2012 (16). Moreover, additional analysis revealed that publicity through the 3rd trimester was not related to elevated threat of perinatal mortality, untimely supply, low delivery weight, or low Apgar scores (16). The molecular weight (about 369) is low enough that excretion into breast milk should be anticipated. Because of the carcinogenicity noticed in animals, and the potential for suppression of gastric acid secretion within the nursing toddler, the use of lansoprazole during lactation is greatest prevented. Medications used to treat nausea and vomiting of pregnancy and the risk of chosen birth defects. The indication for the drug suggests that human being pregnant expertise might be very limited. In the acid setting of the higher gastrointestinal tract, lanthanum ions are released to bind dietary phosphate from meals throughout digestion. However, lanthanum is sure to bone and is slowly released with an estimated half-life of two. When the highest dose was given from implantation through lactation, offspring had delayed eye opening, reduction in body weight achieve, and delayed sexual development (preputial separation and vaginal opening). In long-term research, lanthanum carbonate was not carcinogenic in rats but was related to an increased incidence of glandular abdomen adenomas in male mice. Moreover, even the minimal amounts that may be excreted would bind with milk phosphate, resulting in a nonabsorbable complex. The effect of this binding on toddler bone growth is unknown however is probably not clinically vital. Although the near absence of human being pregnant experience prevents an entire evaluation of the embryofetal danger, the drug must be averted in being pregnant. Pregnant rats got doses during organogenesis and thru lactation that produced systemic exposures that had been about 6. At this exposure, 91% of the pups died by the 4th day after start, however this dose also caused maternal toxicity. There were no teratogenic results at the highest publicity, but minor anomalies noticed were left-sided umbilical artery, cervical rib, and precocious ossification. In rabbits, maternal toxicity was observed at doses leading to exposures that had been about 0. Decreased fetal physique weights and minor skeletal variations have been noted at both doses, and abortions were observed on the greater dose (1). There were no effects on mating or fertility in feminine and male rats given doses producing exposures that had been 6. However, in feminine rats, this exposure during breeding and through the primary 6 days of gestation was related to a major decrease within the number of stay fetuses. Although the high plasma protein binding will inhibit transfer, the molecular weight (about 926 for the nonhydrated form) and the extended half-life suggest that embryofetus publicity will occur. A 44-year-old girl with breast cancer conceived while being treated in a section I clinical trial with lapatinib (2). During the earlier 10 years, she had been treated with numerous antineoplastic brokers, including cyclophosphamide, doxorubicin, fluorouracil, paclitaxel, trastuzumab, and vinorelbine. She additionally had undergone a left modified radical mastectomy, regional radiation, and 10 years of tamoxifen. When cancer was discovered in her proper breast, she was enrolled within the scientific trial. She was initially handled with lapatinib 1500 mg/day, but the dose was decreased by 50% due to diarrhea and rash.
Generic 300mg quetiapine overnight deliveryThe traditional dose consumed was 800 mcg (two 200-mcg tablets orally plus two tablets vaginally), however some ladies may have taken as much as 9200 mcg (46 tablets) (8). Five infants with congenital malformations who had been uncovered through the 1st trimester to misoprostol in unsuccessful attempts at abortion had been described in a 1991 case report (9). The complete dose was 1200 mcg in two of the mothers and 400600 mcg in the other three circumstances. The five infants had an unusual defect of the frontotemporal area of the cranium consisting of an asymmetric, well-circumscribed anomaly of the skull and overlying scalp, exposing the dura mater and underlying cerebrum. Surgical correction of the defect was attempted within 4 days of birth in every of the circumstances, however one toddler died of severe infection. Although the authors conceded that a later-acting agent was instructed by the character of the defect, three of the mothers denied any additional makes an attempt to terminate their pregnancies after the use of misoprostol (9). In a later publication, two of the authors described more fully the defects of the scalp and skull in three of the newborns (10). Two further reviews describing the use of misoprostol as an abortifacient by Brazilian ladies appeared in 1993 (11,12). In Rio de Janeiro throughout a 9month period of 1991, of 803 women admitted to hospitals with abortion complications, 458 (57%) had self-administered misoprostol to induce abortion (11). The median dose used was 800 mcg (range 20016,800 mcg) with 65% taking it orally, 29% orally and vaginally, and 6% vaginally solely. The most regularly cited causes by the women for in search of medical care have been vaginal bleeding (80%) and uterine cramps (78%). Morbidity among the many 458 women included heavy bleeding (19%) (1% required blood transfusion), an infection (17%), curettage required (85%), uterine perforation after curettage (1%), and systemic collapse (1%). In Fortaleza, Brazil, misoprostol use accounted for 444 (75%) of 593 incomplete abortions handled in a hospital by uterine evacuation throughout 1991 (12). Complications noticed in the 444 women included a hundred and forty four (32%) with infection, 1 with septic shock, 3 with hypovolemic shock, and 1 with uterine perforation. Since 1990, 29 ladies had contacted a teratogen information counseling service after unsuccessful makes an attempt at inducing abortion with misoprostol in the course of the 1st trimester. The mean dose used by these girls was 4000 mcg (20 tablets), with a range of 200 mcg (one tablet) to eleven,200 mcg (56 tablets). The girls have been monitored with ultrasonography in the course of the the rest of their pregnancies. The outcomes of the pregnancies were: spontaneous abortions (2nd trimester)-3; nonetheless pregnant-3; lost to follow-up-6; regular infants-17 (one with preauricular tag). Of the 17 normal infants, 8 were examined by the authors, four have been examined by pediatricians not associated with the authors, and in 5 cases verbal data was obtained from the mothers (13). The absence of data for the 9 (31%) cases, nonetheless, lessens the power to interpret this report. Seven cases of limb defects involving the palms and toes following 1st trimester use of misoprostol (dose range 6001800 mcg) as an unsuccessful abortifacient have been described in a 1993 report (14). Four of the infants demonstrated bilateral palsy of cranial nerves, leading to a prognosis of Mцbius sequence (6th and seventh nerve palsies). In the seven pregnancies with sufficient element, misoprostol publicity was thought to have occurred between 30 and 60 days following conception. The investigators attributed the anomalies to misoprostol-induced vascular disruption (14). In a 1993 invited editorial on the strengths and weaknesses of case reports, the publication of the above analysis was thought to be valid as a result of the association with delivery defects was biologically plausible and there were different reviews supporting a causal association (15). A brief report (16) and summary (17) suggested that a attainable mechanism for Mцbius syndrome was flexion of the embryo within the space of cranial nuclei 6 and seven that resulted in vascular disruption of the area bent. The cranial nuclei 6 and 7 are situated in a region of the embryo that would be bent if there was pressure in a cephalocaudal direction. The hypothesis proposed that flexing of the region would result in decreased blood flow and hemorrhage and/or cell demise of the cranial nuclei. It was hypothesized that misoprostol-induced uterine contractions early in gestation, earlier than there was adequate amniotic fluid to cushion the embryo, would cause the flexing if the embryo was accurately positioned. Experiments in rat embryos confirmed that hemorrhage would occur on this area after mechanical flexion within the proposed direction. The authors concluded that attempted abortion with misoprostol was related to an elevated threat of Mцbius syndrome (18,19). Although the mom had had hen pox at 12 weeks, there was no evidence within the placenta or fetus of viral infection. The Latin-America Collaborative Study of Congenital Malformations discovered 12 misoprostol-exposed newborns among 5708 malformed and 5708 nonmalformed matched controls (21). Each of the exposures concerned unsuccessful makes an attempt by the ladies to induce abortion. Four of the infants had been within the control group, but the maternal dose (1000 mcg) was identified in just one case. Significant associations with two different malformations that had not been reported beforehand were holoprosencephaly (5. However, the authors recommended warning in interpreting these latter defects as causal associations. They concluded that there was a causal association between the four vascular disruption defects and the usage of misoprostol as an abortifacient (22). Of notice, a 1996 report provided detailed descriptions of three cases of arthrogryposis. The explanation for the defect was thought to be vascular disruption resulting in nerve harm that led to fetal akinesia and subsequent contractures (23). There have been 25 circumstances of Mцbius syndrome, 24 cases of discount of phalanges, and 227 instances with isolated malformations. A single misoprostol pill (strength not specified) had been inserted vaginally for four days, however only some vaginal bleeding had occurred on day four. A 1998 research proposed that the abnormalities observed in youngsters uncovered in utero during the 1st trimester to misoprostol have been induced by uterine contractions that caused vascular disruption within the fetuses, including ischemia of the brain-stem (26). Five children had a distinctive arthrogryposis, without cranial nerve injury, that was confined to the legs. Severe amyoplasia of the legs was confirmed in 5 youngsters by electromyography, and two of the instances had poor anterior horn cell activity. Eight had hydrocephalus associated with elevated stress that required shunt placement to relieve. One baby had an omphalocele, but no proof of cranial nerve defects of arthrogryposis (26). A 1997 summary and 1999 full report described a prospective, observational cohort examine of 86 misoprostol-exposed pregnancies compared with 86 pairmatched controls (27,28). All of the women had known as a teratogen information service regarding pregnancy publicity to both misoprostol or nonteratogenic brokers. There were no statistical variations between the teams in the rates of major (2/67 vs. The pattern dimension had restricted energy because it was solely able to detect an eightfold enhance within the threat of major malformations (28).
Diseases - Bickel Fanconi glycogenosis
- Enamel hypoplasia cataract hydrocephaly
- Chronic obstructive pulmonary disease
- Bacterial food poisoning
- Holoacardius amorphus
- Dyskinesia
- Meier Rotschild syndrome
- Wells syndrome
- Enolase deficiency type 2
- Congenital mitral malformation
Buy quetiapine 50 mg overnight deliveryThe use of nimodipine together with magnesium sulfate was not beneficial because of the danger for maternal heart block (6). The four liveborn infants have been delivered by cesarean section as soon as maternal blood strain was managed. One mother died of extreme postpartum problems, and another developed multiorgan illness secondary to severe preeclampsia/eclampsia (7). A 1998 abstract described an ongoing international, multicenter, randomized, managed trial comparing the results of nimodipine and magnesium sulfate in the prevention of eclampsia (8). Maternal hypotension brought on by nimodipine is a possible, however yet unreported, complication that might jeopardize the fetus. An in vitro research has examined the potential use of nimodipine as a tocolytic agent (10). Thus, extra data on the potential for nimodipine-induced maternal hypotension could additionally be forthcoming. In a 1996 case report, a 36-year-old lady at 3 weeks postpartum experienced a transient medical syndrome of paresthesias (arm and face) related to motor dysphasia (11). The symptoms resolved, but perioral dysesthesia and motor dysphasia recurred after cerebral angiography. Over a 24-hour interval, she obtained a complete dose of forty six mg (1 mg/hr for two hours, then 2 mg/hr). Milk samples have been collected (5060 mL/collection) by the affected person each 34 hours throughout nimodipine remedy and blood samples have been drawn about each 6 hours. Assuming a milk intake of a hundred and fifty mL/kg/day, the authors estimated that the toddler would have received 0. Nimodipine as a substitute for magnesium sulfate in the management of severe preeclampsia: maternal and fetal results (abstract). Widespread cerebral ischaemia handled with nimodipine in a affected person with eclampsia. The use of nimodipine in a affected person with eclampsia: colour move Doppler demonstration of retinal artery rest. The haemodynamic and respiratory results of intravenous nimodipine used within the remedy of eclampsia. Kaya T, Cetin A, Cetin M, Sarioglu Y Effects of endothelin-1 and calcium channel blockers on. Other calcium channel blockers have been extensively used in human being pregnant as antihypertensives and tocolytics without proof of main congenital defects or fetal toxicity (see Nicardipine, Nifedipine, and Verapamil). The elimination half-life (about 712 hours) of this agent permits for once-daily dosing. No teratogenicity was observed in rats and rabbits, but fetotoxicity, more than likely due to maternal toxicity, did occur in each species. In this specific study, management monkeys additionally had elevated rates of abortion and mortality (1). The molecular weight (about 388) is low sufficient that placental transfer should be anticipated. No reviews describing the usage of nisoldipine during human pregnancy have been positioned. A 1992 abstract did report the profitable use of the agent in 12 girls for the therapy of severe postpartum pregnancy-induced hypertension (2). The molecular weight (about 388) is low sufficient that excretion into breast milk should be expected. Other calcium channel blockers are excreted in milk and are classified as suitable with breastfeeding by the American Academy of Pediatrics (see Diltiazem, Nifedipine, and Verapamil). Although the animal knowledge are suggestive of low threat, the absence of human being pregnant experience prevents an evaluation of danger that the drug represents to an embryo or fetus. However, until human being pregnant data can be found, publicity to the agent must be averted within the 1st trimester, if attainable. The molecular weight of one of many active metabolites, tizoxanide (about 265), is low enough for placental passage, however the intensive plasma protein binding will limit the amount of drug transferred to the embryo or fetus. The molecular weight of one of many lively metabolites, tizoxanide (about 265), is low sufficient to be excreted into breast milk, but the in depth plasma protein binding (>99. In vitro analysis of actions of nitazoxanide and, tizoxanide towards anaerobes and cardio organisms. Nitazoxanide for the remedy of intestinal protozoan and helminthic infections in Mexico. Nitazoxanide in the remedy of cryptosporidial diarrhea and other intestinal parasitic infections associated with acquired immunodeficiency syndrome in tropical Africa. Nitazoxanide, a possible drug for eradication of Helicobacter pylori with no cross-resistance to metronidazole. Nitazoxanide, a nitrothiazolide antiparasitic agent with anti-vacuolating toxin exercise. Pharmacokinetics of nitazoxanide after single oral dose administration in 6 healthy volunteers. Although the incidence is unknown, the uncommon reports of this toxicity combined with the recognition of the drug for urinary tract infections in pregnant girls recommend that the risk is rare. Neither impaired fertility, teratogenicity, nor different fetal antagonistic results had been noticed in rats and rabbits treated with nitrofurantoin earlier than and through gestation (1,2). In a surveillance study of Michigan Medicaid recipients involving 229,one hundred and one accomplished pregnancies performed between 1985 and 1992, 1292 newborns had been uncovered to nitrofurantoin through the 1st trimester (F. Specific data were obtainable for six defect classes, including (observed/expected) 15/12 cardiovascular defects, half of oral clefts, 0/2 spina bifida, 4/4 polydactyly, 3/2 limb reduction defects, and 5/3 hypospadias. One producer (Norwich-Eaton Laboratories) has collected greater than 1700 case histories describing the utilization of this drug throughout various stages of being pregnant (95 references) (personal communication, 1981). In a broadcast study, a retrospective evaluation of ninety one pregnancies by which nitrofurantoin was used yielded no evidence of fetal toxicity (3). In a 1995 report, 22 studies of nitrofurantoin use in being pregnant were evaluated for a meta-analysis (5). These outcomes demonstrated no vital correlation between nitrofurantoin use in early gestation and congenital malformations (5). In contrast to the above reports, a 2003 casecontrol research, using data from three Swedish health registers, was conducted to determine drug use in early pregnancy that was associated with cardiac defects (6). A 2009 report from the National Birth Defects Prevention Study estimated the association between antibacterial agents and greater than 30 selected birth defects (7). The authors carried out a population-based, a number of website, case control examine of girls who gave delivery to an toddler with certainly one of >30 chosen defects. The outcomes had been identified in a 10-state delivery defect surveillance program and involved 13,one hundred fifty five circumstances and 4941 controls chosen from the same geographical regions. Exposure to an antibacterial was determined by an in depth phone interview performed inside 24 months after the estimated date of delivery. Significant associations (total number of exposed casescontrols; number of associations) additionally were found for penicillins (716 293; 1), erythromycins (20278; 2), cephalosporins (12847; 1), quinolones (4214; 1) and tetracyclines (366; 1).
Generic quetiapine 100 mg without a prescriptionThe manufacturer classifies the drug as contraindicated due to the toxicity noticed in three animal species. The defects included umbilical hernia, gastroschisis, imperforate anus, alterations in heart form and size, limb malrotations, skeletal malformations of the tail, and delayed ossification of cranial, vertebral and pelvic bones. Defects included umbilical hernia, medially rotated or quick limbs, absent or fused digits on paws, cleft palate, open eye lids, low-set ears, and kinked tail (1). In a 2-year dietary carcinogenicity study in mice, lomitapide triggered significant increases of liver adenomas and small intestine carcinomas in males and mixed adenomas and carcinomas in females. In 2-year research in rats, there have been no statistically vital drug-related increases in tumor incidences. The molecular weight (about 790) and high plasma protein binding suggest that exposure of the embryofetus might be restricted, however the long terminal half-life may allow the drug to cross. However, if a mother receiving the drug chooses to breastfeed, the toddler should be monitored for the most common (incidence 28%) adverse effect seen in adults. These results include diarrhea, nausea, vomiting, dyspepsia, and stomach ache (1). No revealed reports linking the usage of loperamide with congenital defects have been located. Reproduction research with rats and rabbits at doses up to 30 instances the human dose have revealed no evidence of impaired fertility, teratogenicity, or different fetal harm (1). In a surveillance examine of Michigan Medicaid recipients involving 229,one hundred and one completed pregnancies conducted between 1985 and 1992, 108 newborns had been exposed to loperamide in the course of the 1st trimester (F. In a 1999 abstract, the being pregnant outcomes of 89 women exposed to loperamide within the 1st trimester had been in contrast with matched controls (2). There were no significant variations between the groups when it comes to major and minor malformations, spontaneous abortions, elective abortions, preterm supply, and start weights. However, in 21 moms who took loperamide all through gestation, start weights tended to be lower (200 g) (ns) (2). Simultaneous plasma and milk samples had been collected 12 hours after the primary dose, and 6 and 24 hours after the second dose. Small amounts of loperamide oxide had been measured in some of the plasma samples, however the imply loperamide oxide milk concentrations had been <0. The American Academy of Pediatrics classifies loperamide as suitable with breastfeeding (4). The animal information are suggestive of average risk as a outcome of the exposure for lopinavir was lower than the human therapeutic exposure. The agent is simply obtainable in a hard and fast combination (200 mg lopinavir/50 mg ritonavir per capsule; eighty mg lopinavir/20 mg ritonavir per mL oral solution). The plasma ranges of ritonavir are very low; subsequently, the antiviral activity of the combination is as a end result of of lopinavir. Plasma protein binding of lopinavir is excessive (98%99%), primarily by 1-acid glycoprotein, but some is certain to albumin. The average half-life of lopinavir over a 12-hour dosing interval is 56 hours (1). Developmental toxicity (decreased pup survival) additionally was observed in a perinatal and postnatal rat research at doses producing exposures equal to or larger than about zero. Consistent with the molecular weight (about 629) and lipid solubility, lopinavir crosses the human placenta. A 2006 study using the ex vivo human cotyledon perfusion model discovered that placental switch of lopinavir (combined with ritonavir) was appropriate with passive diffusion, even within the presence of physiologic concentrations of human albumin (2). The quantity getting into the fetal compartment was properly above the 50% inhibitory focus (2). The Antiretroviral Pregnancy Registry reported, for January 1989 through July 2009, prospective knowledge (reported before the outcomes had been known) involving 4702 live births that had been uncovered during the 1st trimester to a quantity of antiretroviral agents (5). There have been 1794 outcomes exposed to lopinavir (526 in the 1st trimester and 1268 within the 2nd/3rd trimesters) in combination with different antiretroviral brokers. There had been 39 delivery defects (9 in the 1st trimester and 30 within the 2nd/3rd trimesters). In reviewing the delivery defects of potential and retrospective (pregnancies reported after the outcomes were known) registered circumstances, the Registry concluded that, except for isolated instances of neural tube defects with efavirenz exposure in retrospective reports, there was no other sample of anomalies (isolated or syndromic) (5). Because pregnancy is a threat factor for hyperglycemia, there was concern that these antiretroviral agents would exacerbate this threat. An summary published in 2000 described the outcomes of a research involving 34 pregnant ladies handled with protease inhibitors compared with forty one controls that evaluated the affiliation with diabetes (7). Two critiques, one in 1996 and the other in 1997, concluded that each one ladies currently receiving antiretroviral therapy ought to continue to receive remedy throughout being pregnant and that remedy of the mom with monotherapy should be thought-about inadequate therapy (8,9). The identical conclusion was reached in a 2003 evaluate with the added admonishment that therapy have to be steady to forestall emergence of resistant viral strains (10). The molecular weights of lopinavir (about 629) and ritonavir (about 721), combined with their lipid solubility, recommend that the drugs might be excreted into human breast milk, although the in depth plasma protein binding (98%99%) ought to restrict this excretion. Placental transfer of lopinavir/ritonavir within the ex vivo human cotyledon perfusion mannequin. Determination of lopinavir and nevirapine by high-performance liquid chromatography after solid-phase extraction: application for the assessment of their transplacental passage at supply. Antiretroviral Pregnancy Registry International Interim Report for 1 January 1989 via 31 July 2009. Moreover, a major increase in loratadine-induced congenital malformations would be uncommon, as no different antihistamine has been shown to be a serious human teratogen. If an oral antihistamine agent is required throughout being pregnant, first-generation brokers similar to chlorpheniramine or tripelennamine must be considered. Previous reviews revealed before the availability of the studies mentioned beneath concluded that loratadine and cetirizine had been acceptable alternate options, besides during the 1st trimester, if a first-generation drug was not tolerated (13). Treatment of pregnant rats from gestational day 7 through postpartum day 4 with doses as much as 26 occasions the human medical exposure revealed no evidence of antiandrogenic exercise, as demonstrated by a lack of impact on androgen-dependent growth in male offspring (5). The molecular weight (about 383) is low enough that passage to the fetus must be anticipated. A 1998 noninterventional, observational cohort examine described the outcomes of pregnancies in ladies who had been prescribed a quantity of of 34 newly marketed medicine by basic practitioners in England (6). The outcomes of those pregnancies included 2 elective abortions and sixteen normal, time period infants (6). A 2002 examine found no elevated risk of teratogenicity or other pregnancy or new child problems for antihistamines when utilized in early being pregnant for the therapy of nausea and vomiting (N = 12,394) and allergy (N = 5041) (7). A collaborative 2003 report gathered information from four teratology data providers (Canada, Israel, Italy, and Brazil) pertaining to 1st trimester loratadine exposures in 161 pregnancies (8). The stay birth rate, gestational age at delivery, and start weight in the two groups were related. There were five congenital malformations (kidney defect, aortic valve stenosis, unspecified chromosomal abnormalities, bilateral inguinal hernia, and congenital hip dislocation) within the loratadine group and six in the controls. The research population consisted of 563 male infants with hypospadias and 1444 male infants with no main delivery defects. During forty eight hours, the imply amounts of loratadine and metabolite recovered from the milk have been four. The American Academy of Pediatrics classifies loratadine as appropriate with breastfeeding (11).
Buy generic quetiapine on-lineHowever, the ibritumomab tiuxetan therapeutic regimen contains radioactive elements. If inadvertent being pregnant does occur, the woman must be informed of the potential for embryofetal harm. The therapeutic routine includes indium-111 ibritumomab tiuxetan and yttrium-90 ibritumomab tiuxetan, prepared immediately earlier than administration, and previous rituximab (see also Rituximab). In sufferers receiving the therapeutic routine, the imply effective half-life for yttrium-90 activity in blood was 39 hours (1). The ibritumomab tiuxetan therapeutic routine may cause severe, infusionrelated toxicity, together with hypotension and other adverse effects. Neither have research been conducted for carcinogenicity, mutagenicity, or results on fertility. Moreover, the ibritumomab tiuxetan therapeutic regimen results in a big radiation dose to the testes. Although it has not been studied, the therapeutic routine does have the potential to cause poisonous results on the male and female gonads (1). Rituximab, a component of the therapeutic routine, does cross the placenta, no less than at time period (see Rituximab). The effects of this potential exposure on a nursing infant are unknown, but immunosuppression and different extreme adverse effects, including those from radiation, are potential complications. Persistent pulmonary hypertension of the new child could occur if these brokers are used within the third trimester close to delivery (13). No evidence of developmental abnormalities was observed in copy studies in rats and rabbits at doses slightly less than the utmost human scientific dose (8). The manufacturer has received info by a voluntary reporting system on the utilization of ibuprofen in 50 pregnancies (9). Five infants with defects were observed, including an anencephalic infant exposed through the 1st trimester to ibuprofen and Bendectin (doxylamine succinate and pyridoxine hydrochloride), petit mal seizures progressing to grand mal convulsions, cerebral palsy (the fetus had additionally been exposed to other drugs), a hearsay report of microphthalmia with nasal cleft and mildly rotated palate, and tooth staining (M. Seven of the pregnancies had been electively terminated, 3 had unknown outcomes, and eight of the pregnancies had been progressing at the time of the report. In a surveillance examine of Michigan Medicaid recipients involving 229,one hundred and one accomplished pregnancies carried out between 1985 and 1992, 3178 newborns had been exposed to ibuprofen in the course of the 1st trimester (F. Specific data have been out there for six defect classes, including (observed/expected) 33/30 cardiovascular defects, 7/5 oral clefts, 3/2 spina bifida, 11/9 polydactyly, 5/5 limb discount defects, and 4/8 hypospadias. The prevalences of congenital malformations in infants of those ladies and the reference group had been N = 46, 4. There was no evidence of a particular grouping of defects or of a doseresponse relationship for adverse birth end result. Moreover, the affiliation was stronger if the initial use of medication was round conception of in the occasion that they were used for >1 week. There was no drug specificity for cardiac malformations, but 5 of the six circumstances of orofacial clefts had been exposed to naproxen (12). A 2003 casecontrol study was carried out to establish drug use in early being pregnant that was associated with cardiac defects (13). Cases (cardiovascular defects with out identified chromosome anomalies) have been drawn from three Swedish well being registers (N = 5015) and controls consisting of all infants born in Sweden (19952001) (N = 577,730). The data supported a vascular hypothesis for the pathogenesis of gastroschisis (14). A population-based being pregnant registry (N = 36,387) was developed by linking three databases in Quebec (see Naprosyn for other research details). Case infants had been those with any congenital anomaly identified in the first yr of life and had been compared with matched controls. There additionally was a major affiliation for anomalies of the respiratory system 9. There were no significant associations for oral clefts or defects involving other major organ systems. Among these brokers, the one significant affiliation was for ibuprofen prescriptions in the 1st trimester and congenital defects (p <0. The use of ibuprofen as a tocolytic agent has been related to decreased amniotic fluid volume (1719). Of the 17 ladies, ibuprofen, 12002400 mg/day, was used alone in three pregnancies and was combined with ritodrine in one. One lady who was treated with ibuprofen for 44 days returned to a traditional amniotic fluid quantity after the drug was stopped (time for reversal not specified) (17). Terbutaline and magnesium sulfate have been combined with ibuprofen at numerous times for tocolysis. Oligohydramnios in every sac (pockets <1 cm) was documented by ultrasonogram on the twentieth day of therapy and ibuprofen therapy was stopped. Therapy was restarted 5 days later when regular fluid quantity for the three fetuses was observed, however oligohydramnios was once more evident after 4 days and ibuprofen was discontinued. Tocolysis was then maintained with terbutaline and normal fluid volumes have been observed 5 days after the second course of ibuprofen. No cases of true oligohydramnios had been noticed, although three instances of low-normal fluid occurred that resolved after discontinuation of ibuprofen. Periodic Doppler echocardiography throughout remedy revealed a non-dose-related delicate constriction of the ductus arteriosus in four (6. Ductal constriction was observed in three of the fetuses within 1 week of starting ibuprofen. Normal echocardiograms have been obtained in all four cases inside 1 week of discontinuing therapy (19). Ibuprofen is usually used by pregnant girls, based on a 2003 study that recognized the medicines taken by a rural inhabitants (20). Among 578 individuals, 86 (15%) took ibuprofen during pregnancy, including 20 in the course of the third trimester. Ibuprofen was the fourth most commonly used over-the-counter medication (after acetaminophen, calcium carbonate, and cough drops) (20). The authors acknowledged that further research were needed as a end result of most of those associations had not been reported from other databases (21). A 2013 research evaluated the impact of extended use of ibuprofen and acetaminophen throughout pregnancy on the neurodevelopment of 3-year-old samesex sibling pairs (22). The cases came from the prospective Norwegian Mother and Child Cohort Study (see Acetaminophen for examine details and results with acetaminophen). Prenatal acetaminophen was associated with significantly poorer outcomes than nonexposed siblings. In contrast, ibuprofen prenatal publicity was not associated with antagonistic neurodevelopment outcomes (22).
Purchase quetiapine with american expressA second Registry report, published in 2006 overlaying the years 19952003, analyzed the relationship between antidepressants and major malformations or cardiac defects (3). In 2006, the manufacturer reported the findings of a retrospective cohort research utilizing United States United Healthcare information (2). There had been 5956 infants of moms allotted paroxetine or different antidepressants during the 1st trimester, including 815 for paroxetine. For 453 ladies who stuffed such a prescription in the 2nd and 3rd months of pregnancy, 31 (6. A 2007 examine evaluated the affiliation between 1st trimester publicity to paroxetine and cardiac defects by quantifying the doseresponse relationship (6). There were 101 infants with main congenital defects, 24 involving the heart, among the 1403 women utilizing only one type of antidepressant through the 1st trimester. A study revealed in 2007 was performed to decide if paroxetine exposure within the 1st trimester was associated with congenital malformations (25). Exposure to the antidepressants was based on drug dispensing and timing was primarily based on estimated dates of conception for singleton and multigestations. Using knowledge collected in 19952004, the research cohorts included 1020 infants exposed to paroxetine monotherapy or polytherapy in the 1st trimester, and a subset of 815 infants exposed solely to paroxetine monotherapy in the 1st trimester. The comparability cohorts, uncovered to different antidepressants, had been 4936 uncovered to monotherapy or polytherapy, and a subset of 4198 infants exposed solely to monotherapy in the 1st trimester. A variety of research limitations have been mentioned, similar to lacking knowledge from charts that could not be assessed and the inability to document actual consumption of the antidepressants. The investigators concluded that the findings instructed a attainable modest increased occurrence of congenital defects compared with different antidepressants (25). There have been 9849 case infants with main malformations and 5860 management infants with out malformations. Additional studies are required however, even when confirmed, absolutely the risks are small because the estimated prevalence of the defects also is small. The variety of girls using every agent was seventy three fluoxetine, 36 sertraline, 19 paroxetine, 7 citalopram, and three fluvoxamine. A 2008 retrospective casecontrol study from the province of Quebec concerned 2329 girls who had used antidepressants, 189 (8. No association was discovered between the period of antidepressant use during the 1st trimester and major congenital defects (29). Women taking paroxetine (N = 348) or fluoxetine (N = 253) within the 1st trimester had been in contrast with girls exposed to nonteratogens (N = 1467). In addition, data was obtained from 5 revealed database research concerning 2061 circumstances of 1st trimester publicity to paroxetine. The prospective casecontrol examine concerned 235 ladies who took the agents through the 1st trimester and who gave start in the years 20002007 at one center. Although there was a twofold higher risk for cardiac defects, all the defects within the uncovered group had been thought-about mild (32). Their mother had used paroxetine 5 mg/day in the course of the first 2 months of being pregnant and 20 mg/day in the final three weeks. At delivery, facial dysmorphism, consisting of hypertelorism, proptosis, hypoplastic nasal pyramid, and wide nostrils have been noted. Neurobehavioral and motor indicators had been noted on the 2nd day of life (hyperactivity, irritability, jitteriness, hyperextension of the trunk and limbs with worsening dyspnea during handling). At 6 months of life, the twins had enough psychomotor improvement with no neurobehavioral or respiratory signs (33). In a population-based casecontrol research from the Netherlands, 678 instances (fetuses and children with isolated heart defects) were in contrast with 615 controls (fetuses and youngsters with a genetic disorder with no coronary heart defect) (34). A 2010 meta-analysis of epidemiological research evaluated 1st trimester exposures to paroxetine and congenital defects, particularly cardiac defects (35). The investigators analyzed revealed information from 1992 to 2008 and, in some situations, concerned additional info that was requested and obtained from the unique authors. The meta-analysis found little proof of publication bias or general statistical heterogeneity. However, the increased prevalence of aggregated defects might have resulted, partially, from the elevated prevalence of cardiac defects (35). Immediately following this meta-analysis have been two refined commentaries, one supporting an association between paroxetine and cardiac defects (36) and one opposing such an affiliation (37). A prospective cohort examine evaluated a large group of pregnancies uncovered to antidepressants within the 1st trimester to decide if there was an affiliation with major malformations (38). In addition to the 149 paroxetine instances, the opposite circumstances have been 113 bupropion, 184 citalopram, 21 escitalopram, sixty one fluoxetine, fifty two fluvoxamine, sixty eight mirtazapine, 39 nefazodone, sixty one sertraline, 17 trazodone, and 154 venlafaxine. There had been 5 main anomalies in the paroxetine group: bilateral pulmonary hypoplasia, ventricular septal defect, clinodactyly, cleft lip and palate, and an omphalocele. There were no main defects in the pregnancies exposed to bupropion, escitalopram, or trazodone (38). The signs within the four infants included jitteriness, irritability, lethargy, myoclonus, vomiting, and hypothermia. In one toddler, serum levels of paroxetine and desipramine on days 5 and 15 of age have been 48 and 70 ng/mL, respectively, and <10 and <10 ng/ mL, respectively. In a second infant, the serum paroxetine concentration on day 2 was 66 ng/mL, whereas trazodone was undetectable. Two infants have been hypoglycemic (one shortly after delivery and one at 40 hours of age), however each moms had gestational diabetes mellitus. The withdrawal symptoms in a single toddler resolved over a few days, but some signs in the different three were nonetheless apparent at discharge on days 5, 22, and 24 of age, respectively (39). Male infants uncovered to paroxetine (N = 3; 10 forty mg/day), citalopram (N = 1; 30 mg/day), or fluoxetine (N = 1; 20 mg/day) during gestation exhibited withdrawal signs at or within a quantity of days of delivery and lasting up to 1 month. Symptoms included irritability, constant crying, shivering, increased tonus, eating and sleeping problems, and convulsions (40). The untimely toddler was bottle-fed and did properly through the first few days, but then grew to become irritable, torpid, hypertonic, apathetic, and jittery. The pregnancy outcomes of 55 girls taking paroxetine (median dose 20 mg/day) within the third trimester have been reported in 2002 (42). Twelve neonates had problems requiring short-term intensive remedy and prolonged hospitalization. The problems, all resolving within 12 weeks, included respiratory distress (N = 9; 3 preterm infants), hypoglycemia (N = 2), and jaundice (N = 1). Twenty-seven women in the comparison group had used paroxetine (median dose 20 mg/day) in the 1st and 2nd trimesters, however not within the 3rd trimester. There had been no significant variations between the groups by means of gestational age at delivery, premature births, birth weight and size or, at follow-up, in sex distribution or acquire in weight and size (expressed at percentage). There was one major defect in each group: small asymptomatic ventricular septal defect (exposed); bilateral lacrimal duct stenosis that required surgery (control). The check outcomes for mental growth were comparable within the groups, but significant variations within the topics included a slight delay in psychomotor improvement and lower habits motor high quality (tremulousness and fine motor movements) (43). He was discharged residence at 48 hours of age, however was readmitted 2 days later because of lethargy and the absence of cry.
Candlewick (Mullein). Quetiapine. - What is Mullein?
- Use on the skin for wounds, burns, hemorrhoids, bruises, frostbite, and other uses.Use by mouth for earaches, colds, flu, asthma, diarrhea, migraines, gout, tuberculosis, croup, cough, sore throat, inflammation of the airways such as bronchitis, and other conditions.
- Dosing considerations for Mullein.
- Are there safety concerns?
- How does Mullein work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96569
Cheap quetiapine 200 mg overnight deliveryGeneral reproduction, perinatalpostnatal and teratology studies of nitrofurantoin macrocrystals in rats and rabbits. Foetal security of nitrofurantoin macrocrystals therapy throughout being pregnant: a retrospective evaluation. Pyelonephritis in pregnancy: a potential randomized trial to forestall recurrent illness evaluating suppressive remedy with nitrofurantoin and shut surveillance. The security of nitrofurantoin, in the course of the first trimester of being pregnant: meta-analysis. Hemolytic reactions to nitrofurantoin in patients with glucose-6-phosphate dehydrogenase deficiency: principle and apply. Efficacy of long-term antimicrobial prophylaxis after acute pyelonephritis in being pregnant. The effect of therapeutic dosages of nitrofurantoin (Furadantin) upon spermatogenesis in man. Prospective follow-up of antagonistic reactions in breast-fed infants exposed to maternal treatment. The animal research in one species used systemic exposures that most likely had been a lot higher than these obtained in humans from topical application and, more than likely, have little scientific significance. Nitrofurazone is indicated as adjunctive remedy for sufferers present process treatment for extreme burns when bacterial resistance to different agents is a real or potential downside. It is also indicated for sufferers present process pores and skin grafting when contamination with resistant micro organism may cause graft rejection (1,2). In mice, reproduction studies with systemic nitrofurazone induced a low frequency of limb reduction defects in a single examine (3,4), however not in another (3). In rabbits, doses up to 30 occasions the similar old human dose (assumed to be primarily based on weight) had been embryocidal (5). The molecular weight (about 198) and lipid solubility counsel that the drug will cross the placenta if it is absorbed, however the scientific significance of this is unknown. The Collaborative Perinatal Project monitored 50,282 motherchild pairs, 234 of whom had publicity to nitrofurazone in lunar months 14 (6). Structural anomalies had been observed in seven instances, one major and 6 minor defects. The molecular weight (about 198) and lipid solubility suggest that the drug will be excreted into milk, however the clinical significance of this is unknown. However, the variety of ladies handled throughout pregnancy is limited, especially in the course of the 1st trimester. Nitroglycerin seems to be a safe, efficient, rapid-onset, short-acting tocolytic agent. The use of transdermal nitroglycerin patches may also prove to be efficient when longer periods of tocolysis are required. With any route of administration, however, extra studies are required to determine the most secure effective dose. The drug, a rapid-onset, short-acting vasodilator, has been used to management severe hypertension during cesarean section (1,2). The use of nitroglycerin sublingually for angina throughout pregnancy with out fetal harm has also been reported (3). Recent investigations, discussed below, have explored using nitroglycerin as each an emergency and a routine tocolytic agent. Reproductive studies in rats and rabbits have been conducted with nitroglycerin (46). The Collaborative Perinatal Project recorded seven 1st trimester exposures to nitroglycerin and amyl nitrite plus eight other patients exposed to different vasodilators (7). From this small group of 15 patients, four malformed kids have been produced, a statistically vital incidence. Because of the lack of particular information and the small variety of patients, no conclusions as to the relative safety of nitroglycerin within the 1st trimester could be produced from this examine. When volume growth was combined with nitroglycerin therapy, a marked resistance to the hypotensive effect of the drug was observed. Recovery occurred after nitroglycerin therapy was terminated and then restarted at a decrease dose. In three different fetuses, a lack of beat-to-beat variability (average variability <5 beats/minute) was famous. Therapy was continued and no abnormalities had been noticed in the umbilical blood gases or Apgar scores. An summary revealed in 1996 described using transdermal nitroglycerin patches (releasing 10 mg in 24 hours) within the therapy of gestational hypertension (10). The 24-hour imply systemic and diastolic blood pressures have been significantly decreased (5% and 7%, respectively). In a 1995 research, 12 women with severe preeclampsia obtained an infusion of nitroglycerin beginning at zero. The mean systolic blood stress decreased from 161 to 138 mmHg, whereas diastolic pressure decreased from a mean of 116 to 103 mmHg. The umbilical artery pulsatility index modified considerably however not the uterine pulsatility index, implying vasodilation in the umbilical circulation and avoidance of antagonistic impairment of fetoplacental perfusion (11). A progressive flattening of fetal heart price beat-to-beat variability was noticed in all six sufferers. Prevention of an increase in imply arterial stress of >20% was achieved in solely two of the ladies, and all had nausea, retching, and vomiting that was apparently not dose-related. Maternal diastolic blood pressure was maintained above 50 mmHg while on nitroglycerin and, apparently, no fetal distress was noticed. In addition, gentle chest pain occurring during labor was efficiently treated with sublingual nitroglycerin in one of many girls. Both sufferers survived and eventually delivered infants apparently unaffected by the treatment. The use of nitroglycerin during cesarean part to enable supply of babies entrapped by a contracted uterus has been described in two case stories (18,19). In the first case, the top of a baby presenting as a double footling breech was trapped within the hypertonic upper phase (18). The Apgar scores of the 3090-g, term toddler had been 5 and 9 at 1 and 5 minutes, respectively. In the second case, a woman acquired a 100-mcg bolus of nitroglycerin to quickly relax a contracted uterus and to allow the successful supply of her twins (19). Other than a systolic blood strain lower (preoperative pressure one hundred twenty mmHg; after nitroglycerin 85 mmHg) that responded quickly to ephedrine, no different opposed results from nitroglycerin were encountered in the mother or her newborns. The uterus relaxed palpably within 20 seconds and the fetus was repositioned to permit for vaginal delivery. A lower within the maternal blood stress was famous (145/100 to 130/75 mmHg, then stabilizing at 130/85 mmHg within 2 minutes), but the heart rate and oxygen saturation remained unchanged. The premature toddler was delivered vaginally shortly after rupture of the membranes and start of an oxytocin infusion. Two 400-mcg boluses got, resulting in uterine leisure inside 30 seconds. Three cases of whole breech extraction, with inside podalic version in two, of the second twin were aided by means of nitroglycerin spray (0.
50 mg quetiapine for saleIn a surveillance research of Michigan Medicaid recipients involving 229,101 accomplished pregnancies conducted between 1985 and 1992, 20 newborns had been exposed to rifampin through the 1st trimester (F. No controlled research have linked the use of rifampin with congenital defects (9,10). One report described nine malformations in 204 pregnancies that went to term (11). The malformations had been anencephaly (one case), hydrocephalus (two cases), limb malformations (four cases), renal tract defects (one case), and congenital hip dislocation (one case) (11). Rifampin has been implicated as one of the agents answerable for hemorrhagic disease of the newborn (6). In one of the three infants affected, solely laboratory evidence of hemorrhagic disease of the newborn was current, however in the other two, clinically evident bleeding was observed. Prophylactic vitamin K1 is really helpful to forestall this critical complication (see Phytonadione). Rifampin may intrude with oral contraceptives, resulting in unplanned pregnancies (see Oral Contraceptives) (15). These quantities have been thought to represent a very low risk to the nursing toddler (18). The American Academy of Pediatrics classifies rifampin as compatible with breastfeeding (19). Haemorrhagic illness of the new child in the offspring of rifampicin and isoniazid handled mothers. Bericht ueber 2 faelle von normaler fetaler entwicklung nach rifampicin therapie in der fruehsch wangerschaft. Preliminary observations on using a model new semi-synthetic rifamycin by-product in gynecology and obstetrics. Human pregnancy experience is proscribed to three circumstances, two of which ended in 1st trimester spontaneous abortions. Although comorbid conditions had been current and should have brought on the losses, the outcomes are sufficiently regarding to warrant caution in prescribing rifapentine early in being pregnant. Until further information are forthcoming, rifapentine is greatest averted during the 1st trimester. The elimination half-lives of rifapentine and its lively metabolite are each about 13 hours (1). Reproduction studies with rifapentine in rats and rabbits produced teratogenic and poisonous results in each species. Embryo and fetal poisonous results included increases in resorption charges, postimplantation losses, and stillbirths, and decreased fetal weight. Major anomalies noticed within the offspring of pregnant rabbits administered doses 0. The molecular weight (about 877) is low sufficient that publicity of the embryo and fetus most likely occurs. In addition, the extended elimination half-lives of the parent compound and its energetic metabolite improve the chance for passage of the brokers into the fetal compartment. In a medical research by the manufacturer, three ladies became pregnant whereas receiving rifapentine, 600 mg twice weekly (combined with isoniazid, ethambutol, pyrazinamide, and pyridoxine) and three grew to become pregnant throughout follow-up (1,2). The first affected person had a positive serum being pregnant check at baseline and subsequently obtained a single 600-mg dose of rifapentine earlier than being dropped from the examine. The second affected person, with a historical past of alcohol abuse, acquired 10 doses of rifapentine 600 mg over 42 days before exclusion from the research. She was handled over 85 days with 22 rifapentine 600-mg doses and had a 1st trimester spontaneous abortion sixteen days after the last dose. When taken in the previous few weeks of being pregnant, rifapentine might cause hemorrhage in each the mother and newborn secondary to vitamin K deficiency (1). Patients receiving rifapentine ought to be suggested to change to nonhormonal strategies of contraception (1). Because energetic untreated tuberculosis represents a higher danger to the fetus than does remedy, quick initiation of drug remedy is normally beneficial, regardless of the gestational stage (36). An earlier statement by the World Health Organization beneficial a 6-month regimen of isoniazid (plus pyridoxine), rifampin, and pyrazinamide as first-line treatment in being pregnant (6). The molecular weight of rifapentine (about 877) and the prolonged half-lives of the father or mother compound and the lively metabolite (both about thirteen hours) counsel that these agents shall be excreted into milk. Breast milk may be discolored as a outcome of rifapentine produces a red-orange discoloration of physique fluids. Rifampin, a intently related antibiotic with a similar molecular weight (about 823), is excreted in low quantities into breast milk. The American Academy of Pediatrics classifies rifampin as suitable with breastfeeding (see Rifampin). The animal replica data suggest threat, but the amount absorbed from the gastrointestinal tract was not quantified. In people, the very small quantities absorbed systemically counsel that the embryofetal threat is low, if it exists at all. Although inadvertent exposure early in gestation seems to characterize a low threat, the safest course, because of the animal knowledge, is to avoid the antibiotic within the 1st trimester. Until human being pregnant data are available, ladies must be recommended that the absence of human being pregnant expertise prevents an correct assessment of the embryo fetal threat. It is a derivative of rifamycin that has antibacterial activity in opposition to a broad spectrum of grampositive and gram-negative bacteria, including aerobic, anaerobic, and enteropathogens (2,3). The effects included cleft palate, agnathia, jaw shortening, hemorrhage, partially open eye, small eyes, brachygnathia, incomplete ossification, and elevated thoracolumbar vertebrae. The molecular weight (about 786) is low enough for passive switch, but solely a very small quantity of the antibiotic is absorbed into the systemic circulation. After a 400-mg dose in wholesome nonpregnant topics, the mean most plasma concentrations had been within the vary of 410 ng/mL (1). A 2005 evaluation concluded that the dearth of absorption and the security profile in nonpregnant adults advised that rifaximin was safe in pregnancy for the remedy of infectious diarrhea (2). The molecular weight (about 786) is low sufficient for excretion into breast milk, but only very small quantities of the antibiotic are absorbed into the systemic circulation. The effects of this exposure on a nursing infant are unknown, but seem to be negligible. Rifaximin, a peculiar rifamycin by-product: established and potential medical use outdoors the gastrointestinal tract. The protein brought on developmental toxicity (structural anomalies and death) in two animal species. If the agent is given shortly before or throughout being pregnant, the lady ought to be counseled as to the potential embryofetal threat. It is indicated for the remedy of cryopyrin-associated periodic syndromes, together with familial chilly auto-inflammatory syndrome and Muckle-Wells syndrome in adults and youngsters 12 years of age.
Buy quetiapine 100mg lineIn a 1979 report, metronidazole was utilized in fifty seven pregnancies including 23 during the 1st trimester (9). Three of the 1st trimester exposures resulted in spontaneous abortion (a normal incidence), and in the remaining 20 births, there have been 5 congenital anomalies: hydrocele (two), congenital dislocated hip (female twin), metatarsus varus, and psychological retardation (both mother and father mentally slow). The Collaborative Perinatal Project monitored 50,282 motherchild pairs, 31 of whom had 1st trimester publicity to metronidazole (28). Two mothers, treated with metronidazole in the course of the 5th7th weeks of gestation for amebiasis, gave delivery to infants with midline facial defects (29). One of the infants had holotelencephaly and one had unilateral cleft lip and palate. A mother treated for trichomoniasis between the 6th and seventh weeks of gestation gave birth to a male infant with a cleft of the onerous and taste bud, optic atrophy, a hypoplastic, quick philtrum, and a Sydney crease on the left hand (30). The mom was also taking an antiemetic medication (Bendectin) on an "as wanted" foundation. In this identical report, the authors, from information obtained from the Michigan Medicaid program between 1980 and 1983, cited 1020 other instances in which metronidazole use in the 1st trimester for therapy of vaginitis was not linked with birth defects. In an extra sixty three circumstances, use of the agent for this indication was linked to a birth defect diagnosis. In a continuation of the study cited immediately above, 229,a hundred and one completed pregnancies of Michigan Medicaid recipients were evaluated between 1985 and 1992 (F. Of this group, 2445 newborns had been uncovered to metronidazole during the 1st trimester. Specific data have been obtainable for six defect classes, together with (observed/expected) 23/24 cardiovascular defects, 1/1 spina bifida, 4/7 polydactyly, 2/4 limb reduction defects, 7/6 hypospadias, and 8/4 oral clefts. Using information from the Tennessee Medicaid program, pregnancy outcomes of ladies (N = 1307) who had crammed a prescription for metronidazole between 30 days before and one hundred twenty days after the onset of their final normal menstrual interval had been compared with those of women who had not filled such a prescription (32). Data have been out there for 1322 uncovered (1318 live births; four stillbirths) and 1328 nonexposed (1320 reside births; 8 stillbirths) infants. Similar outcomes had been obtained when congenital malformations had been analyzed by particular sorts, including those of the central nervous system, coronary heart, gastrointestinal tract, musculoskeletal system, urogenital system, respiratory tract, chromosomal, and by a quantity of organ techniques. The investigators concluded that using metronidazole was not associated with an increased danger for start defects (32). A examine printed in 1995 performed a meta-analysis of seven research (from a total of 32 references identified in their search) that met their criteria for assessing the security of metronidazole use in human pregnancy (33). Based on these findings, the investigators concluded that using metronidazole through the 1st trimester was not related to an elevated danger of congenital defects (33). A second meta-analysis, comparable in design to the research above, evaluated the danger for start defects after using metronidazole early in being pregnant (34). A complete of 5 studies, one unpublished casecontrol examine and four published cohort studies, met the inclusion criteria. A large ethnically homogeneous population-based dataset (Hungarian Case Control Surveillance of Congenital Abnormalities, 19801991) was utilized in a study published in 1998 to consider whether the use of metronidazole within the 1st trimester was related to congenital anomalies (35). Minor abnormalities and congenital abnormality syndromes of known origin had been excluded. However, based mostly on the prevalence of isolated cleft lip (with or without cleft palate) of their population and the prevalence of publicity to metronidazole through the 2nd and third months of being pregnant, their evaluation advised that even a real affiliation would only enhance the prevalence of the defect from one hundred cases/100,000 births to 103 cases/100,000 births. Moreover, the finding was not confirmed when the comparison was made with the whole control group (35). In a second study from the above group, the teratogenic potential of vaginal metronidazole plus miconazole therapy during the 2nd and 3rd months of pregnancy was evaluated using the 19801996 dataset of the Hungarian Case Control Surveillance of Congenital Abnormalities (36). They in contrast 22,843 girls who had new child infants or fetuses with congenital anomalies (cases) with 38,151 pregnant women who had newborns without defects (controls). A population-based cohort examine on using metronidazole throughout being pregnant from 1991 to 1996 was carried out in Denmark and reported in 1999 (37). An estimated 35,000 pregnancies were used in the danger evaluation for the specific outcomes of congenital abnormalities, low delivery weight (<2500 g), and preterm birth (<37 weeks). Data on the use of metronidazole had been decided from a prescription database and categorised as both publicity from 30 days earlier than conception to the top of the 1st trimester (group 1) or in the course of the 2nd and 3rd trimesters (group 2). A complete of 138 prescriptions to the agent were obtained by 124 girls during the examine interval. Based on prevalence charges of congenital anomalies in the uncovered (group 1) and control teams of two. The two birth defects in group 1 were transposition vasorum with ventricular septum defect and hypertelorism. After adjustment for maternal age, delivery order, gestational age, and smoking, there was no difference in imply delivery weight between those uncovered and the controls. The investigators acknowledged the major limitations of their examine: low statistical energy as a result of the small number of exposed subjects; the lack to management for potentially confounding components; and the ignorance on spontaneous abortions and fetuses aborted for prenatal prognosis of malformations. They concluded, nevertheless, that their outcomes confirmed no proof of main teratogenicity and no indication for the termination of pregnancies due to publicity to metronidazole (37). Metronidazole has been proven to markedly potentiate the fetotoxicity and teratogenicity of alcohol in mice (38). A 2001 potential, controlled cohort study evaluated the pregnancy outcomes of 217 ladies uncovered to metronidazole (86. The women had consulted a Teratogen Information Service regarding their exposure to the drug. A matched management group consisted of 612 women who had referred to as about nonteratogenic exposures. There have been no statistical differences between the groups when it comes to spontaneous abortions (7. A variety of reports have described the utilization of metronidazole in pregnant girls with bacterial vaginosis in makes an attempt to cut back the incidence of preterm births (4050). Compared to the placebo group (N = 36), the pregnancy outcomes of the active drug group (N = 44) included significantly fewer admissions for preterm labor (27% vs. Another prospective randomized, double-blind, placebo-controlled research first printed in summary kind in 1993 (43) and then in full in 1995 (44) described the effect of a 7-day course of oral metronidazole (750 mg/day) combined with a 14-day course of oral erythromycin base (999 mg/day) in pregnant ladies at increased threat for preterm delivery (based on a historical past of spontaneous preterm delivery or prepregnancy body weight less than 50 kg). A complete of a hundred and ten girls (26%) within the active group delivered preterm (<37 weeks) in contrast with sixty eight girls (36%) within the placebo group (p = 0. However, the rates of preterm delivery in these without bacterial vaginosis were almost similar (22% within the lively drug group vs. In distinction, in these with bacterial vaginosis, the charges of preterm supply have been 31% for the lively drug group in contrast with 49% in these receiving placebo, p = 0. The constructive association with anti-infective treatment existed both for ladies with a history of preterm delivery (39% vs. A 1997 randomized, placebo-controlled examine additionally found that the useful impact of a 2-day course of oral metronidazole (400 mg twice daily) on prolonging pregnancy was restricted to those ladies with bacterial vaginosis and a previous historical past of spontaneous preterm delivery (45). Another 1997 randomized, double blind, placebo-controlled research administered a mix of metronidazole and ampicillin to 59 ladies and placebo to 51 girls (46).
Buy cheap quetiapine 300mgReported malformations aside from limb reduction included: defective abdominal muscle tissue (1 case); diaphragmatic hernia (2 cases); exencephaly, cleft palate, adrenal hypoplasia (1 case); cleft palate (2 cases); and renal cystic degeneration (1 case) (46). In a surveillance examine of Michigan Medicaid recipients involving 229,a hundred and one completed pregnancies carried out between 1985 and 1992, 75 newborns had been uncovered to imipramine in the course of the 1st trimester (F. No anomalies have been noticed in three different defect classes (oral clefts, polydactyly, and limb discount defects) for which specific data had been out there. The outcomes of these pregnancies have been 1 elective abortion, three spontaneous abortions, 25 normal newborns, and 2 infants with congenital defects. The defects (all exposed in the 1st trimester or longer) have been six fingers on right hand, and an omphalocele (16). Neonatal withdrawal symptoms have been reported with the use of imipramine during being pregnant (1719). Symptoms noticed in the infants during the 1st month after birth had been colic, cyanosis, rapid breathing, and irritability. Urinary retention within the neonate has been related to maternal use of nortriptyline (chemically associated to imipramine) (20). A 2002 prospective research in contrast two teams of motherchild pairs uncovered to antidepressants throughout gestation (46 exposed to tricyclics-12 to imipramine; forty to fluoxetine) with 36 nonexposed, not depressed controls (21). Assuming a therapeutic serum degree of 200 ng/mL, an infant consuming a thousand mL of breast milk would ingest a every day dose of about zero. Concentrations of imipramine in fore- and hindmilk ranged from 34 to 408 ng/mL and from 48 to 622 ng/mL, respectively. The American Academy of Pediatrics classifies imipramine as an agent whose impact on the nursing infant is unknown however may be of concern (25). Although the combined data counsel that the potential for human developmental toxicity is low, the info are too restricted for a more complete assessment. Until such information can be found, the safest course is to avoid imiquimod in pregnancy, but if exposure does occur, the danger to the embryo and/or fetus seems to be low. Small amounts of imiquimod are absorbed systemically and are eradicated slowly with a half-life of about 20 hours. In patients with actinic keratoses handled for 16 weeks, peak serum drug concentrations have been 0. The quantity absorbed systemically appears to be more associated to the surface area treated than to the dose (1). In vitro studies conducted with imiquimod have shown that it stimulates the manufacturing of the cytokines interferon-, interleukin-1, interleukin-1, interleukin-6, and interleukin-8 (2). Because placental trophoblasts additionally express many of these similar cytokines, an in vitro research was conducted to determine if imiquimod exposure during pregnancy might alter normal placental operate. The fetal results included elevated resorptions, decreased physique weight, delays in skeletal ossification, and bent limb bones. When these doses were continued throughout pregnancy, parturition, and lactation, no effects were noticed on growth or postnatal growth. However, bent limb bones in the fetuses had been famous, as they have been with exposure throughout organogenesis, in the absence of maternal toxicity. Multiple exams with imiquimod revealed no proof of mutagenic or clastogenic potential (1). The low molecular weight (about 240) and long elimination half-life after systemic absorption (about 20 hours) recommend that the drug will attain the embryo and/or fetus. However, as a end result of the systemic concentrations are very low, the actual publicity seems to be clinically insignificant. Because there was superb scientific response, she was prescribed further treatment, but the girl was lost to follow-up till she delivered vaginally at 41 weeks. A 2006 report described the outcomes of seven pregnancies exposed to topical imiquimod, all ending in live births with a mean start weight of 3528 g (4). The drug had been used for genital warts in four cases and for warts of the hand, face, or foot in three. Doses of the 5% cream ranged from once day by day to 4 occasions per week with durations starting from 1 to 10 weeks (average 5 weeks). Two ladies used the drug in the 1st trimester, one in the 2nd trimester, two within the 2nd and third trimesters, and two in the third trimester solely (4). Two studies reported the utilization of imiquimod for the treatment of anogenital warts in a complete of 21 pregnant women (5,6). The relatively low molecular weight (about 240) and long elimination half-life (about 20 hours) counsel that the drug will be excreted into breast milk. However, the amount absorbed systemically and available for excretion into milk may be very low and doubtless is clinically insignificant. Therefore, although the chance to a nursing infant is unknown, use of imiquimod by the mom seems to be appropriate with breastfeeding. Treatment of exterior genital warts with 5% imiquimod cream throughout being pregnant: a case report. Topical imiquimod 5% cream remedy for exterior anogenital warts in pregnant girls: report of four instances and evaluation of the literature. When hepatitis B occurs during pregnancy, an increased fee of abortion and prematurity may be observed (1). It is indicated for postexposure prophylaxis of hepatitis A and measles (rubeola) and within the prevention of significant infections in patients with immunoglobulin deficiencies. American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. Four subclasses of IgG and two totally different antibodies within the preparation additionally crossed to the fetus in an analogous manner (2). Others have discovered that the placental transfer of exogenous IgG is determined by the dose and period of therapy and, presumably, on the method of IgG preparation (3). The indications included hypogammaglobulinemia similar to frequent variable immunodeficiency, autoimmune ailments similar to persistent immune thrombocytopenic purpura, and alloimmune issues such as extreme Rh-immunization disease and alloimmune thrombocytopenia. No opposed results have been observed within the fetus or newborns in any of the above reports, however warning has been advised in its use to prevent spontaneous abortion (11). Transplacental passage of intravenous immunoglobulin within the last trimester of pregnancy. Intravenous immunoglobulin therapy of pregnant sufferers with recurrent being pregnant loss brought on by antiphospholipid antibodies and Rh immunization. Intravenous immunoglobulin therapy for recurrent abortions brought on by antiphospholipid antibodies. Congenital heart block: successful prophylactic treatment with intravenous gamma globulin and corticosteroid remedy. High-dose intravenous gamma globulin: does it have a role in the remedy of severe erythroblastosis fetalis? Because rabies is almost 100% fatal if contracted, both the immune globulin and the vaccine must be given for postexposure prophylaxis (1). No threat to the fetus from the immune globulin has been reported (see additionally Vaccine, Rabies [Human]) (13).
References - Gonzalez-Cadavid NF: Mechanisms of penile fibrosis, J Sex Med 6(Suppl 3):353n362, 2009.
- Mandal AK, Sharma SK, Vaidyanathan S, et al: Ureterovaginal fistula: summary of 18 yearsi experience, Br J Urol 65(5):453n456, 1990.
- Henderson FC, Geddes JF, Vaccaro AR, et al: Stretch-associated injury in cervical spondylotic myelopathy: new concept and review, Neurosurgery 56(5):1101n1113, discussion 1101n1113, 2005.
|
|

