"Purchase cheap oratane, acne gel prescription."By: Dawn Sowards Brezina, MD - Assistant Professor of Medicine
 https://medicine.duke.edu/faculty/dawn-sowards-brezina-md
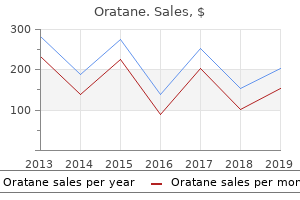
Purchase 20 mg oratane mastercardFascial Planes e partitions and oor of the pelvis are coated by the endopelvic, or parietal, fascia. With this info, surgeons must individualize the remedy and care of every patient. History e affected person with rectal cancer normally presents to the surgeon after a de nitive endoscopic analysis. Speci c signs might help the surgeon in deciding on the optimal approach to therapy. Information pertaining to anal sphincter function is invaluable when one is considering a low anastomosis. Preoperative sexual function is essential to know as a result of one should discuss the dangers of the process and possible diminution of sexual function postoperatively. A complete medical history ought to be aimed at figuring out other medical circumstances, such as cardiopulmonary, renal, and diet, that will require further evaluation earlier than surgical intervention and permit appropriate risk stratication. For sufferers with a cardiac historical past or symptoms, a stress test and cardiology evaluation are indicated. Women should undergo an entire pelvic examination so as to decide vaginal invasion or spread to the ovaries. Accurate preoperative staging is gaining rising significance as combined-modality remedy and sphincter-preserving surgical approaches are thought of. Ureteral involvement by the tumor can be assessed and permits for planning of ureteral stent placement preoperatively. Rigid proctoscopy can additionally be essential to the evaluation of sufferers with rectal cancer because it demonstrates the proximal and distal levels of the mass from anal verge; extent of circumferential involvement; orientation within the lumen; and relationship to the vagina, prostate, or peritoneal re ection. Furthermore, a mass will often be described as being a sigmoid or rectosigmoid tumor on exible colonoscopy, and, when the affected person is evaluated in the o ce with rigid sigmoidoscopy, the lesion is usually found to be a lot lower and in fact is often a real rectal cancer that quali es for neoadjuvant chemoradiotherapy. A full colonoscopy to the cecum is essential to rule out synchronous cancers, which occur 2�8% of the time. Localized cancers involving only the mucosa and submucosa usually can be distinguished from tumors that penetrate the muscularis propria or lengthen by way of the rectal wall into the perirectal fat. Staging by scientific examination, radiology, and pathology aids in planning therapy, evaluating response to remedy, evaluating the outcomes of varied remedy regimens, and figuring out prognosis. Depth of invasion (T stage) of the primary tumor is a vital prognostic variable as increasing depth of invasion is correlated with an increasing likelihood of lymph node metastases. For instance, early-stage cancers extending into the muscularis mucosa (T1) will have a 10�13% incidence of metastasizing to perirectal lymph nodes. Large arrow demonstrates ngerlike projections of carcinoma invading into the mesorectal fat. Super cially invasive, small cancers could additionally be managed e ectively with local excision. Yet others current with regionally superior tumors adherent to adjoining structures such because the sacrum, pelvic sidewall, vagina, uterus, cervix, prostate, or bladder, requiring an even more in depth operation. After establishing the diagnosis and completing the staging workup, a decision is made whether or not to pursue immediate resection or administer preoperative chemoradiotherapy. Bowel Preparation e high bacterial load in the intestinal tract requires preoperative bowel decontamination to cut back the incidence of infectious issues. Prior to the routine use of mechanical bowel preparation and preoperative antibiotics, the reported price of infection following colorectal surgery was 60%. In two separate surveys of North American colorectal surgeons, nearly two-thirds most well-liked the polyethylene glycol electrolyte solutions because of the reliability of the cleansing outcomes. Studies have proven that mechanical bowel preparation provides little, if any, extra bene t to lowering the perioperative an infection rate. However, we nonetheless suggest to our sufferers that a mechanical bowel preparation be carried out largely because it allows for simpler manipulation of the colon and rectum with both open and laparoscopic surgical procedure. Poorly di erentiated cancers have a worse long-term prognosis than well- or moderately di erentiated tumors. Other components that portend a poor prognosis include direct tumor extension into adjacent constructions (T4 lesions); lymph node metastases; lymphatic, vascular, or perineural invasion; and bowel obstruction. Following a doubtlessly healing resection, the 5-year survival rate varies according to illness extent22,23 (Table 40-4). However, these survival gures may enhance with the elevated use of adjuvant remedy. Instead of an oral antibiotic preparation most surgeons use perioperative systemic antibiotics. A typical option to cowl each aerobic and anaerobic intestinal micro organism is cefazolin and metronidazole administered intravenously simply prior to the skin incision. Postoperative antibiotic prophylaxis usually is continued for 24 hours, though the perioperative dose is more important. Some surgeons do "double" prophylaxis with oral and systemic antibiotics in all surgeries below the peritoneal re ection. Perioperative systemic antibiotic protection is broadened in sufferers with high-risk cardiac lesions corresponding to prosthetic heart valves, a earlier history of endocarditis, or a surgically constructed systemic-pulmonary shunt and with intermediate-risk cardiac lesions such as mitral valve prolapse, valvular heart disease, or idiopathic hypertrophic subaortic stenosis. Vancomycin is substituted for ampicillin if the patient is allergic to penicillin or cephalosporin. Goals of Surgery for Rectal Cancer e major goal of surgical therapy for rectal most cancers is complete eradication of the primary tumor along with the adjoining mesorectal tissue and the superior hemorrhoidal artery pedicle. For tumors positioned in the extraperitoneal rectum, resection margins are limited by the bony con nes of the pelvis and the proximity of the bladder, prostate, and seminal vesicles in men and vagina in women. Although locoregional recurrence could additionally be inevitable, local recurrence, remedy, mortality, anastomotic leaks, and colostomy rates after rectal most cancers surgical procedure are associated to surgical approach as nicely as to the expertise and volume of the person surgeon and establishment. Data from a randomized, potential trial conducted by the National Surgical Adjuvant Breast and Bowel Project demonstrated no signi cant di erences in survival or local recurrence when comparing distal rectal margins of lower than 2, 2�2. Furthermore, the size of mesorectum past the primary tumor that should be removed is believed to be between three and 5 cm because tumor implants usually are seen no further than four cm from the distal fringe of the tumor throughout the mesorectum. Many of those reviews are restricted, small, single-institution research, often combining sufferers with tumors of di erent depths, including T3 lesions, positive margins, or who underwent di erent types of local remedy, such as fulguration and snare cautery. Major risk factors for native recurrence embrace constructive surgical margins, transmural extension, and poorly di erentiated histology. Anderson Cancer Center, forty six sufferers underwent transanal excision of small distal rectal most cancers followed by postoperative radiation remedy. Tumor involvement of the circumferential margin has been proven to be an impartial predictor of each native recurrence and survival. Chapter 40 Cancer of the Rectum 845 From the New England Deaconess Hospital in Boston, patients with small distal cancers (<4 cm in diameter and <10 cm from the dentate line) with no evidence of metastatic illness have been entered in a prospective examine. Patients with T2 lesions handled with local excision were given postoperative chemoradiation. Several patients have been found to have T3 lesions and all have been beneficial additional radical surgical procedure. All patients had been followed each three months for two years after which each 6 months for 5 years. Surgery alone was enough for T1 lesions, and surgical procedure combined with chemoradiation was appropriate for T2 lesions excised with negative margins.
Sterculia urens (Karaya Gum). Oratane. - How does Karaya Gum work?
- What is Karaya Gum?
- Are there safety concerns?
- Are there any interactions with medications?
- Use as a bulk-forming laxative to treat constipation.
- What other names is Karaya Gum known by?
- Stimulating sexual desire (aphrodisia).
- Dosing considerations for Karaya Gum.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96537
Oratane 30mg lineHowever, unlike procedures with planned closed packing, no e ort must be made to remove each identi in a position piece of necrotic tissue on the rst procedure; somewhat, solely tissues which are easily separated by blunt dissection ought to be dissected. Complete removal of all necrotic tissue is completed by a quantity of re-explorations and blunt debridements, limiting blood loss. After debridement, the stomach and colon may be coated with a nonadherent gauze to forestall debridement of wholesome tissue during dressing modifications. Laparotomy pads or other gauze could additionally be positioned immediately within this space, and some authors have recommended presoaking these packs in iodinated options. Some surgeons will suture the gastrocolic ligament to the pores and skin, creating an inverted cone with the base consisting of the divided gastrocolic ligament on the pores and skin stage and the purpose on the pancreatic bed. However, within the setting of acute in ammation this cavity could additionally be ill-de ned, and suturing to the skin is mostly not essential. Drainage tubes are used for strategy of closed drainage or postoperative saline lavage; for open packing method, pancreatic mattress is filled with sterile bandages. Alternatively, some have used a separate retroperitoneal incision through which to deliver packs, closing the stomach incision. Planned re-explorations are carried out in the working room at 2�3 day intervals for additional debridement. Although nearly all of necrotic tissue is debrided with the rst e ort, signi cant amounts of tissue may be eliminated on the fourth and even fth debridement procedure. In some circumstances, the open packing procedure could also be mixed with delayed closure over lavage catheters and steady closed lavage of the lesser sac and abscess cavity. Debridement and Continuous Closed Postoperative Lavage of the Lesser Sac After an preliminary pancreatic debridement, small amounts of residual necrotic tissue are inevitably present. Furthermore, the persistent soilage of the retroperitoneum with pancreatic enzymes and in ammatory mediators may contribute to persistent systemic in ammation and sepsis. Removal of residual necrotic tissue, micro organism, and biologically energetic substances is subsequently proposed to decrease persistent in ammation. Chapter fifty four Management of Acute Pancreatitis 1113 While some have advocated open packing and planned repeated operations to accomplish this goal, others report success with continuous postoperative high-volume lavage of the lesser sac. Beger et al have written extensively on the process of debridement and continuous closed postoperative lavage. Postoperative lavage is facilitated by the insertion of two to ve large double-lumen tubes. After drain placement, the gastrocolic ligament could also be sutured to type a closed compartment within the lesser sac. Continuous lavage is undertaken with hyperosmolar, potassium-free dialysate at approximately 2 L/h, although irrigation with normal saline is also employed. Comparison of Techniques Used in Pancreatic Debridement As noted earlier, the bene ts of varied strategies of pancreatic debridement and postdebridement care have been debated in the literature. No strict criteria have been proposed to adequately choose sufferers for di erent procedures, and the optimum technique of debridement has not been examined in a potential style. A variety of case collection have been reported during which patients with either pancreatic necrosis or severe acute pancreatitis have undergone pancreatic debridement followed by both closure over drains, open packing and redebridement, or closure over lavage catheters with postoperative steady lavage (see Table 54-5). As seen in this desk, reports of postoperative problems and mortality vary extensively across di erent research. Preoperative illness severity is di cult to standardize across di erent reviews, as are the factors for operative administration employed. One small single-institution retrospective research in contrast surgical outcomes in 86 patients with acute pancreatitis after debridement and closed drainage, debridement with open packing, or debridement with continuous closed postoperative lavage. Several collection in the literature have quoted a excessive rate of recurrent pancreatic sepsis and excessive price of reoperation when the technique of debridement and closure over drains is used. However, the Massachusetts General Hospital experience with the closed drainage approach reports a mortality of 6. Others have suggested that the open packing technique may be notably useful in sufferers with a larger mass of necrotic tissue. In this series, Ashley et al demonstrated that nearly all sufferers had been managed with closed drainage. Of these patients, 31 (86%) had been managed with debridement and closure over drains, 1 acquired postoperative irrigation, and 4 required open packing and planned re-exploration. Nineteen sufferers (34%) developed issues, including 9% each with pancreatic or enteric stulas, and 15% with endocrine or exocrine insu ciency. Of patients managed with closure over drains, only four (13%) wanted re-exploration due to inadequate persistent sickness and presumed insufficient debridement. When early operation is mandated, open packing or lavage could additionally be necessary to cope with the results of ongoing necrosis. If operation could be delayed, debridement with closed drainage and typically even inside drainage could additionally be adequate. Minimally Invasive Approaches Although mortality after open pancreatic debridement has decreased in recent years, many series still reveal a mortality fee of roughly 15%; in addition, the mortality in sufferers with established organ failure could exceed 75%. Given the considerable morbidity, organ failure, and mortality associated with traditional open pancreatic debridement, some investigators have instructed that minimally invasive surgical procedures could also be used efficiently with pancreatic necrosis. Avoiding open debridement has the theoretical benefit of minimizing activation of systemic in ammatory processes and decreasing respiratory and wound problems. In latest years there has been a proliferation of stories describing minimally invasive approaches in necrotizing pancreatitis. Solid pancreatic particles has traditionally been thought to be too thick for adequate evacuation with percutaneous drains; still, small research have demonstrated success with percutaneous catheter drainage as a major treatment for infected pancreatic necrosis. Several series of profitable percutaneous management in infected pancreatic necrosis have been reported in the literature. In nine other sufferers, percutaneous intervention was not the only means of therapy however allowed eventual open surgical intervention to be delayed. A latest study by Rocha et al89 by which 28 sufferers with necrotizing pancreatitis have been managed utilizing percutaneous drainage found no clear improvement in total mortality with catheter drainage. An often-unstated precept of remedy for pancreatic necrosis in the past has been the necessity to externally drain the pancreatic mattress. Necrotic tissue, pancreatic enzymes, bacteria, and in ammatory mediators within the contaminated milieu of the necrotic pancreas had been all thought to be best drained outside the physique. In this regard, some investigators have instructed endoscopic therapy for pancreatic necrosis, and have just lately summarized the outcomes. Endoscopic transmural drainage was successful in 31 (72%) sufferers with pancreatic necrosis, though 9 (29%) skilled recurrence and sixteen (37%) experienced complications. Transmural drainage was extra successful with central rather than peripheral necrosis as a outcome of close proximity of the necrotic space to the gastric wall. Seifert et al113 have described a technique of retroperitoneal endoscopy through transgastric fenestration.
Purchase cheap orataneOn the ultrasound picture, this seems to characterize a cyst (and this is what the affected person was told). However, the focal zone is a bit low, and the picture was obtained with harmonic imaging. Here is a repeat ultrasound picture obtained with out compound or harmonic imaging, which exhibits a strong mass with duct extension. Last, the time-gain curve should be adjusted so the fats lobules at all depths are the same shade of grey. Note how the superficial fats is more echogenic than the deep fat on the preliminary image. Compound imaging was additionally used to enhance contrast and improve analysis of the margins. The artifact could additionally be due to a leak within the door seal or electrical equipment close by. Here are the outcomes: Only the overall quantity of color in the picture has decreased. The indicated space increased in enhancement by 55% over baseline (open arrow) on each photographs. Screening mammography is essentially the most widely used modality for detecting breast most cancers and the only one confirmed to cut back the mortality price from the illness. It is a time once we can actually make a difference in the life of an asymptomatic girl who feels nice. You may recognize the names and faces of a variety of the ladies getting into your mammography suite for screening. These are our colleagues, neighbors, lecturers, and others who stay in or near our neighborhood. They are keen to endure the discomfort of mammography because they consider that our interpretation could provide them with the chance to have a malignancy diagnosed at a stage when treatment is extra doubtless. They are relying on us to be properly trained, as much as date, and free of distractions so that our attention and skills shall be absolutely devoted to studying their mammograms. Detection of these cancers can depend upon perception of delicate mammographic changes that happen gradually over years. Developing a consistent approach to studying screening mammograms reduces the prospect of cancers being ignored. Greater familiarity with the extra subtle presenting signs of breast most cancers will improve the most cancers detection fee. Learning about widespread errors in judgment can push up the most cancers detection fee even more. Finally, monitoring the screening performance of the general follow and of every individual radiologist supplies feedback for continual enchancment. Providing screening services in the community somewhat than deep throughout the hospital will increase the probability that women will be screened. Compliance with screening drops precipitously when the power is more than 20 miles away, even when the test is free. Having devoted screening facilities also permits for batch interpretation of research. Once an abnormal finding is detected at screening, ladies will drive a hundred miles and even negotiate their method via your parking storage to get a solution. Thankfully, the overwhelming majority of technologists are devoted and keen about our sufferers. They want to present excellent care and will work hard to obtain high-quality photographs. Review of Chapter 1, the First Question, will provide some instruments for reviewing and optimizing mammographic techniques. When sufferers are recalled because of a prime quality problem, the technologist should evaluate the case to make it a learning experience. A detailed audit of picture quality over a time frame can present further specific feedback for improvement. Review quality recalls by technologist, cause (blur, positioning, other), and consider. Bringing in an professional in mammographic positioning to work with your technologists each few years is a good funding. In medium-size to giant group practices, a subset of radiologists may be identified to batch-read screening research. This strategy is most well-liked over one which has more radiologists reading fewer studies. Radiologists who read screening mammograms should also see diagnostic sufferers and perform breast biopsy. The suggestions from seeing which recalled sufferers are subsequently dismissed, which are really helpful for biopsy, and correlating the imaging findings with pathologic findings provides the premise for persevering with improvement. Batch Versus Online Interpretation the follow of interpreting screening mammograms in batches and recalling sufferers as needed for diagnostic evaluation is far more efficient than interpreting research "online" and performing diagnostic studies throughout the same appointment. Batch interpretation also advantages your sufferers by decreasing the recall fee and rising the cancer detection rate, including the percentage of minimal and early-stage cancers. On the opposite hand, in case your affected person has restricted mobility, drove hours to have her mammogram, has issue with transportation, or might not reliably return for recall, then an immediate studying might enhance affected person compliance. Optimizing the Reading Environment "Time to read the screens" means different things to different radiologists. Whatever your personal routine, keep in mind that the mammographic indicators of malignancy may be troublesome to detect in even the most effective of situations, and that surrounding influences in the workspace can affect the standard and effectivity of interpretation. The optimal setting is a darkened quiet room the place screening studies are reviewed in batches and reported with few interruptions. Your eyes shall be at their best when background lights and laptop screens are directed away from the workstation displays and your line of sight. Computer displays or view boxes placed away from or at a 90-degree angle to the workstation screens reduce the results of extraneous gentle. Focus Equals Efficiency Is your apply involved concerning the effectivity of the radiologists Getting into the screening mindset by batch reading and minimizing distractions focuses the radiologist on discovering cancers. Interpretation of screening mammograms involves holding a visual image of a tissue sample or questioned abnormality in thoughts and relating it to findings on other pictures as you undergo the research. Having the Right Equipment Investing in digital mammography has had a constructive impression on the quality of our practices. Digital mammography additionally improves workflow and makes it easier to examine with previous mammograms. Why not make use of expertise that reportedly marks over 80% of screening cancers and should increase screening most cancers detection by over 19% The data are then reconstructed into multiple tomographic pictures which are reviewed by scrolling via the photographs on a workstation. The tomosynthesis pictures are regularly obtained with a traditional digital mammogram (dual acquisition). This technology is intended to overcome the two major limitations of mammography: false-positive findings attributable to overlapping regular and benign structures, and false-negative research brought on by obscuration of cancers by normal tissues. Tomosynthesis appears to be of biggest value in detecting and evaluating soft tissue density findings (masses, asymmetries, focal asymmetries, and architectural distortion), significantly for ladies with dense tissue.
Buy 40 mg oratane free shippingWalsh and associates randomized 113 patients, and at three years 32% of those receiving preoperative chemoradiation have been alive versus 6% of these present process surgery alone. Poor accrual resulted in untimely closure of the research with fifty six sufferers, well wanting its aim of 500 sufferers. Nonetheless, with median follow-up of 6 years, 5-year survival was 39% for the trimodality group versus 16% for the surgeryalone group. Paradoxically, there also was a development towards improved survival with the addition of radiation, although this nding was not statistically signi cant. In the past, palliative esophagectomy was typically thought necessary to restore swallowing and oral nutrition. Patients with nodal involvement, invasion by way of the esophagus, or probably even invasion into the muscularis usually endure preoperative chemoradiation, while sufferers with simple mucosal involvement typically proceed on to surgery. Tumor in ltration of the wall disrupts the normal-layered look, and extent of penetration is normally clearly visible. In addition, biopsy of deeper layers of tumor not accessible by conventional greedy forceps is feasible. If the tumor is from a node, the cytopathologist should have the ability to identify lymphoid tissue within the specimen. In addition, 15% of sufferers with no radiographic metastatic disease were discovered to have liver metastases by laparoscopic staging. Frequently, radiation might be required preoperatively to maximize margins and spare the larynx, if attainable. If the tumor is xed to the backbone or neck vessels, the procedure is aborted and palliative radiotherapy is taken into account. High-grade malignant stricture is predictive of esophageal tumor stage: risks of endosonographic analysis. A two-team method ought to be thought-about with one group at the neck, while the opposite prepares the gastric conduit. If an excessive amount of trachea has been resected to enable for this, manubrial resection will permit placement of the end tracheostomy lower in the midline. While we favor the triincisional approach for all malignant lesions (for reasons to be mentioned later), lesions within the higher thoracic esophagus generally have to be approached with this method to guarantee enough proximal margins. If the lesion is within the midthoracic esophagus, both the tri-incisional method or the Ivor Lewis approach may be sufficient. Lower esophageal tumors can be resected with either of these two approaches, or additionally with a transhiatal method or left thoracotomy and distal esophagectomy. With any resection, lodging should be made for extra resection with reconstruction if frozen margins are concerned with tumor. Transhiatal Versus Transthoracic Techniques Numerous retrospective analyses have been carried out comparing the transhiatal to the transthoracic (mainly Ivor Lewis) approach. Rindani and associates reviewed 44 trials involving either Ivor Lewis or transhiatal esophagectomy that were revealed in the English language between 1986 and 1996. Di erences were seen within the anastomotic leak rate (16% transhiatal vs 10% Ivor Lewis), stricture price (28% transhiatal vs 16% Ivor Lewis), and incidence of recurrent nerve harm (11% transhiatal vs 5% Ivor Lewis). Hulscher and colleagues additionally performed a meta-analysis of fifty research printed between 1990 and 1999 involving transthoracic and transhiatal resection. Pulmonary complications (19 vs 13%), in-hospital mortality (9 vs 6%), and operative time (5 vs four. Overall longterm survival was related between the two teams (23% for transthoracic and 21. For those patients with nodal disease, nevertheless, none of the transhiatal sufferers was alive at 18 months, whereas 30% of the transthoracic sufferers had been alive at 18 months. Chu and coworkers randomized 39 sufferers with lowerthird esophageal cancers to both Ivor Lewis or transhiatal resection. Intraoperative hypotension occurred in 60% of transhiatal sufferers however only in 5% of transthoracic sufferers. No signi cant di erence was seen in tumor recurrence or survival in the course of the transient follow-up period. A study evaluating transhiatal resection to transthoracic, tri-incisional en bloc resection for distal adenocarcinoma of the esophagus or cardia was carried out within the Netherlands. One hundred and six sufferers had been randomized to transhiatal resection and 114 patients to transthoracic resection. Respiratory complications including atelectasis and pneumonia have been higher within the transthoracic group (57 vs 27%). Although statistical signi cance was not reached, 39% of the transthoracic group was alive at 5 years, whereas solely 29% of the transhiatal group survived 5 years. Placement of the anastomosis within the cervical place appears to improve the risk of recurrent laryngeal nerve harm, anastomotic leak, and stricture. Chapter 18 Surgical Procedures to Resect and Replace the Esophagus 393 An replace of this examine following with a full 5-year follow-up continued to present no statistically signi cant general survival in both approach. It should also be noted that not like the meta-analyses, the randomized trials showed no di erence in recurrent nerve injury or anastomotic leak. Wong famous intraoperative hypotension in 60% of transhiatal dissections, however in solely 5% of transthoracic dissections. It permits for dissection of the intrathoracic esophagus beneath direct imaginative and prescient with complete nodal resection and brings the anastomosis to the neck, allowing for maximal proximal margins and minimizing the chance of an intrathoracic leak. Under common anesthesia, bronchoscopy is performed to rule out tracheal or bronchial (most generally left major bronchial) involvement with tumor. Esophagogastroduodenoscopy is carried out to localize the tumor and rule out disease of the abdomen or duodenum. Division of the intercostal muscles anteriorly and posteriorly often permits enough rib spreading without the necessity to remove a small portion, or shingle, a rib. Dissection of the esophagus begins at a point away from tumor and any associated scarring, and the esophagus is encircled with a Penrose drain. Traction on the Penrose drain allows for cautery dissection encompassing all adjoining nodes. Dissection cranial to this stage entails the vagus nerves; the vagus nerves are peeled o and away from the esophagus to avoid damage to the recurrent vagus branches. An endostapling device is used to divide the azygos vein near its caval connection. A 28F straight chest tube is inserted via a separate stab incision and directed to the apex of the chest. Dissection between the trachea and esophagus have to be accomplished with care and with low cautery dissection to keep away from harm to the membranous trachea. Another Penrose drain is used to acquire traction on the lower esophagus and dissection continues caudally. All tissue between the pericardium, aorta, and azygos vein is dissected and included into the specimen.
Order oratane overnightMore lately, laparoscopic lavage and drainage have been taken up with enthusiasm by a number of teams with some promising results. Abdominal pain is the commonest symptom, a ecting 70% of patients, while 10% are asymptomatic. Treatment is beneficial early, ideally soon after presentation, due to the high complication rate. Surgical treatment might both require a diverticulectomy or segmental resection, and the outcome is usually good. Contrast enemas are significantly helpful for demonstrating the presence and course of an enteric stula. Barium ought to be avoided in the emergency setting, as the consequences of barium-induced peritonitis are catastrophic. It is extremely operatordependent, however it may be used to insert drains and to measure the response of the abscess to drainage. It is regular apply following resolution of the rst episode of diverticulitis to assess the colon for extent of disease and to exclude colorectal malignancy. Care must be taken to wait for full decision of the attack as an in amed colon is simple to perforate; additionally, at times colonoscopy may be very di cult or unimaginable as a result of in ammatory adhesions. Classi cation of Diverticulitis e Hinchey classi cation is a useful grading system for diverticulitis. Management e majority of sufferers with acute diverticular disease could be managed conservatively with intravenous antibiotics. A combination of metronidazole and cipro oxacin or a broad-spectrum antibiotic corresponding to meropenem or amoxicillin and clavulanate (Augmentin) is mostly used. Even then, caution must be exercised, as a signi cant minority of patients whose principal symptom is continual ache will continue to be symptomatic after resectional surgery. A giant population-based study recently has shown only a few sufferers going on to have surgical procedure after preliminary conservative treatment of diverticulitis. Attempts have been made to stratify the management of diverticular disease by pathological and radiological means. Ultimately, the extensive spectrum of illness encountered makes dogmatic statements about intervention unreliable, and sound clinical judgment is still required to determine when to intervene. Indications for operative intervention are di erent in two affected person subgroups: these younger than 50 years and the immunocompromised. Patients with polycystic kidney disease have a really excessive incidence of colonic diverticular disease. In some facilities, routine colonic screening of sufferers awaiting renal allografts is carried out. Patients should be rehydrated with an intravenous infusion; in septic sufferers a urinary catheter is invaluable for assessing an sufficient hourly urine output. Other supportive measures include oxygen remedy, enough opioid analgesia, and antimicrobial therapy. Early oral feeding could commence when tolerated, and a swap to oral antibiotics can be made with signs of decision of in ammation. In nearly all of patients, this conservative remedy will lead to the resolution of symptoms. Surgery is principally directed at controlling peritoneal sepsis and should be tailored to each situation. Even within the face of superior peritoneal signs, a selection of patients will reply to these measures and avoid the requirement for surgical procedure. Resection of the a ected colon is associated with a decrease morbidity and as much as thrice much less mortality compared with nonresection procedures. More lately with the advances in laparoscopic surgical procedure, lavage and drainage of Hinchey types 1�3 have been successfully performed. When bowel continuity is restored after a Hartmann procedure, whole sigmoid colectomy plus removing all of the diverticula- bearing colon and a rectal anastomosis has been shown to reduce the risk of recurrence by some107,a hundred and fifteen but not others. Laparoscopic surgical procedure in colon cancer is oncologically equal to the open approach with better cosmesis, much less analgesic usage, and shorter hospital stays. In over 1100 sufferers reported over the last 5 years, the postoperative complication charges vary from 7. Conversion rates vary between four and 14%, operating time from 141 to 300 minutes, and return of bowel exercise takes between 2 and a pair of. In growing nations the peak incidence is in males in the 40- to 60-year age group that account for up to 90%. Redundancy of a colon is due to both colonic dysmotility, excessive ber consumption, or a genetic predisposition. Volvulus in Western society is usually seen in institutionalized, bed-bound aged sufferers with an acquired megacolon. When an operation is required, the standard of the surgical procedure seems to be more necessary than whether or not the operation is undertaken open or laparoscopically. Further prospective trials investigating recurrence charges, and in particular risk components for recurrence, in addition to the role of prophylactic surgical procedure within the varied subgroups is required. Cecal bascule is a variant of the true cecal volvulus with the di erence being an absence of the axial twist however quite the redundant cecum folds again transversely and upward over the ascending colon. Chapter 32 Diverticular Disease and Colonic Volvulus 659 Presentation Colonic volvulus generally presents with bowel obstruction, vomiting, obstipation, belly pain, and distension. Signs of peritonitis usually point out underlying issues of perforation or gangrene. Complications Perforation of the twisted phase of bowel (closed-loop obstruction) or bowel ischemia and infarction may happen. Secondary renal failure or multiorgan failure may come up because of third-space loss or loss from vomiting. Alternatively, this might be as a end result of reperfusion injury after the volvulus is untwisted. Investigations A plain supine belly x-ray is normally su cient within the analysis of sigmoid and cecal volvulus. In sigmoid volvulus the form is that of a "bent inner tube" with its point aimed at the proper higher quadrant. Other options embrace "2 air to 1 uid level" and a "pair of scales" whereby the uid ranges are at di erent horizontal ranges. To con rm the analysis, a Gastrogra n (diatrizoate meglumine) or barium enema research is performed to look for the "bird beak" signal that signifies the site of twisting of the colon. It has the next fee of therapeutic success than an enema research specifically for the sigmoid volvulus. Of notice reperfusion syndrome is an actual phenomenon following detorsion of an ischemic or gangrenous bowel section. Potential critical bacterial/toxin translocation and multiorgan failure are penalties that the treating clinician must continually keep in check. If no immediate surgery is required, a rectal tube must be placed to stop further recurrences of the volvulus to permit the persevering with decompression of the obstructed colon. For recurrent sigmoid volvulus in a affected person who could face up to surgery, a sigmoid colectomy with or without anastomosis, once the bowel is adequately decompressed, is warranted.
Purchase generic oratane pillsWith a large breast, the default depth may actually must be elevated to include the posterior tissues. The depth may also must be elevated to demonstrate the posterior acoustic enhancement of a cyst or shadowing of a mass. Focal Zone Positioning When surveying the breast, the focal zone should embody the area of the breast tissue from slightly below the skin to the pectoral muscle. Once a lesion is recognized, improvement in image high quality could be gained by narrowing the focal zone to the world of the lesion. Adenosis, lymph nodes involved by tumor, or lymphomatous lots may appear markedly hypoechoic and may be mistaken for cysts. When questioning a cyst within the axilla, remember that cysts in this location are very uncommon, and a pathologic lymph node must be suspected. However, because of the much larger noise introduced by the movie and film processing, the signal-to-noise ratio of film-screen mammography in practice is decrease. The main enhancements gained by way of digital mammography are elimination of film granularity noise and a big enhance within the dynamic vary of x-ray intensities that can be measured. Resolution Higher frequency transducers are higher in resolution however have decrease tissue penetration. Because the breast is a superficial organ, a very high frequency transducer can be utilized. Images of the best axilla in a 71-year-old lady show three markedly hypoechoic masses (A) that could possibly be mistaken for cysts. However, color Doppler examination (B) confirms internal flow within the largest mass, indicating a strong lesion. An ultrasound beam transmitted at one center frequency creates higher harmonic frequencies as it passes by way of tissue. The discount in reverberation artifact may also be useful within the analysis of implants. It can also make delicate abnormalities of tissue echotexture, such as lesions showing mammographically as architectural distortion, much more conspicuous. With compound imaging, additional sweeps are generated at totally different angles, and the returning echoes are compounded to produce the image. A, Mammogram of a 42-year-old girl with a history of reduction mammoplasty shows an irregular mass in the right breast (arrow). B, the lesion is far more conspicuous with tissue harmonic imaging (right picture, B2), and its shadowing is accentuated. A 61-year-old girl recalled from screening because of suspected architectural distortion. B, Ultrasonography with routine processing exhibits a corresponding shadowing hypoechoic lesion. It is necessary for the sonographer and radiologist to realize that the posterior acoustic options of a lesion may be significantly reduced or eliminated by compound imaging. The shadowing of a refined lesion, which will be the only function that permits its detection, may be eliminated by this method. Compound imaging is therefore most useful for characterizing a lesion that has already been detected, somewhat than in survey scanning or screening of a big area. Cancers tend to be firmer on scientific examination, and likewise stiffer on elastography. Elastography maps the relative stiffness of the breast tissue, typically utilizing a colour map. This method makes use of both dimension and stiffness standards; cancers seem bigger on the elastogram. Vibration elastography (shear wave) makes use of a variant of Doppler imaging to generate tissue movement. For example, a small mass with low degree echoes and a benign elastogram might enhance confidence that the lesion represents a cyst. The use of compound imaging permits detailed evaluation of this axillary lymph node. The picture has high distinction, and the form, margins, and inner characteristics of the lesion are well assessed. A, this patient was recalled from screening for analysis of a subtle growing asymmetry (arrow). Images of this malignant mass obtained with conventional (B) and compound imaging (C). During survey scanning a subtle space of shadowing could also be overlooked when utilizing compound imaging. A, Diagnostic mammogram demonstrates an irregular, high-density mass with spiculated margins that corresponds to a palpable lump. B, Ultrasonography demonstrates a round hypoechoic mass with microlobulated margins and an echogenic rim. C, Shear wave elastogram demonstrates very stiff tissue at the anterior border of the mass (red). Using isotropic voxels (a cube) permits viewing of the sequence in any plane with out distortion, so the scan airplane turns into much less essential. The dynamic sequence ought to commence about 30 seconds after injection of contrast agent. Gadobenate dimeglumine (MultiHance, Braco) has a higher relaxivity resulting in improved lesion detection over gadopentetate dimeglumine (Magnevist, Bayer Healthcare). Three to five dynamic sequences are obtained; every dynamic sequence must be lower than 2 minutes. Curve-ology (Color Display) the dynamics of lesion contrast enhancement are predictive of the likelihood of most cancers. Contrast enhancement is considered in two phases: preliminary (rapid, medium, or slow) and delayed (washout, plateau, persistent). Suspicious lesions are much less likely to demonstrate rapid initial enhancement in a woman with low cardiac output. Lowering the color threshold to beneath 60% of background might assist in the analysis of those women. Despite multiple attempts to acquire good fats saturation, fat signal remains to be shiny on the T1 sequence (after contrast). There is elevated sign (arrows) where the breast is touching the coil, mimicking inhomogeneous fats saturation. This worth is usually set at 60% (yellow boxes) on the first time point after distinction (yellow circle). The lesion at the intersection of the reference lines (a small focus of ductal carcinoma in situ) enhances to 64% over background (yellow arrow). For a persistent curve (blue), there is an increase of more than 20%, and a washout curve (red) is a decrease of over 20%.
Syndromes - Ulcers in the mouth, on the tongue, or in the throat
- Tea and coffee
- Do not consume more than 1 alcoholic drink per day for women, 2 per day for men. Certain people should not drink any alcohol.
- Phenylketonuria (PKU)
- Addiction to prescription pain medications (if they are not used correctly)
- Chronic diarrhea
- Inner ear (cochlear) implants
- Medicines to treat symptoms
- If you have diabetes, heart disease, kidney problems, or certain other conditions, you may need to be watched more closely.
Purchase oratane 10mg lineAt instances, in extremely obese people, the addition of an extra port or two is required. If this proves to be the case, we simply insert a further port decrease within the midline. Once the omentum is free, is it placed above the extent of the transverse colon, and the transverse colon mesentery then grasped and elevated to help expose the ligament of Treitz. Once identied, the proximal jejunum is then divided between 30 and 50 cm distal to the ligament. Generally, dividing the bowel on the 50 cm stage supplies a proximal finish of the Roux limb that can reach the proximal stomach in even very large sufferers. However, the division of the mesentery must proceed in a path directly downward on the mesentery, equally dividing the mesentery between the two segments of divided bowel. Straying to either side will cause ischemia to one of the bowel segments, requiring further resection back to viable tissue. Care must be taken to apply gradual application of power in several adjacent points when dividing the most important crossing vessels of the jejunal mesentery. Chapter 27 Morbid Obesity and Its Surgical Treatment 559 but at first the surgeon could wish to use an instrument or some marker that helps estimate intestinal size. In this way the mesentery of the Roux limb has a steady bend in a counter-clockwise course as the limb is being measured. Once the appropriate size of Roux limb is measured, that point is sutured to the biliopancreatic limb with a single suture on the antimesenteric side of the Roux limb connecting to the antimesenteric floor of the biliopancreatic limb about 6 cm proximal to its finish. Resected items of gut are both removed directly now or placed in a specimen bag for later elimination, depending on their size. We have discovered that this double- ring technique essentially eliminates the occasional issue of stenosis of this distal anastomosis, a complication that can show deadly. Finally, the mesenteric defect of the enteroenterostomy is closed with a working permanent suture, beginning at the base of the mesenteric defect and completing the suture by sutures between the top of the biliopancreatic limb and the aspect of the Roux limb a few centimeters past the enteroenterostomy. Some surgeons choose to create the enteroenterostomy using a single-stapled approach. Some surgeons additionally favor to create this anastomosis with a handsutured technique. Proponents for an antecolic Roux limb argue that this technique is faster and has little danger of anastomotic problems due to tension. We nd that the world just to the left and above the ligament of Treitz usually serves as a protected location to create an opening within the transverse colon mesentery with the ultrasonic scalpel. A longitudinal opening a number of centimeters in length is made, and the mesentery is then fastidiously divided with the ultrasonic scalpel. Once a gap is made into the lesser sac, the abdomen is normally readily visible and can be grasped and pulled as much as the opening within the mesentery. Enlarging the mesenteric opening permits enough room to cross the Roux limb into the retrogastric space. Di culties in passing the Roux limb could be overcome with several tips that have been discovered through the years. In this case the gastrocolic ligament often needs to be opened with the ultrasonic scalpel over a 4- to 6-in area. We have discovered the next finest step for guiding the size of the pouch is to have the anesthesiologist cross an Ewald tube, which is a gastric lavage tube used to evacuate the abdomen of enormous clot or particles, measuring 32F in diameter. Some surgeons favor to use a exible endoscope, esophageal dilator, or different space-occupying tube to help as a guide to create the proximal gastric pouch. Once the gastric pouch is created, the Penrose drain is normally visible behind the lower stomach. If not, the gastrocolic ligament could have to be opened to locate it and facilitate passage of the Roux limb as much as the proximal gastric pouch. Retrogastric adhesions are a problem that should be acknowledged in the occasion that they forestall simple passage of the Roux limb. Any limitation to the simple passage of the Roux limb must be investigated by opening the gastrocolic ligament and assessing the posterior gastric floor. Once the 2 organs are thus aligned, a operating suture is used to connect the facet of the Roux limb to the staple line of the proximal gastric pouch. An adjacent enterotomy is made within the Roux limb, using the ultrasonic scalpel for both. We then check the anastomosis for leaks by forcefully injecting methylene blue into the Ewald tube while holding pressure on the Roux limb just past the anastomosis. Chapter 27 Morbid Obesity and Its Surgical Treatment 563 Many surgeons use the round stapler to create the gastrojejunostomy. Should it do so, the Roux limb will assume the form of an accordion, and multiple partial obstructions or a single dominant level of obstruction will typically then end result. We forestall this by tacking the Roux limb to the adjoining proximal portion of the biliopancreatic limb, simply distal to the ligament of Treitz, with a quantity of nonabsorbable sutures. Skin closure is with subcuticular absorbable suture, and the skin websites are dressed with Dermabond (cyanoacrylate). Usually the pores and skin incision must prolong above the xyphoid by about 1�2 cm, and the division of the fascia and muscle should proceed alongside the left aspect of the xyphoid course of. Liver retraction using the open method could also be different than the laparoscopic one. Instead, division of the triangular ligament of the left lobe of the liver and folding the liver inferiorly and medially exposes the gastroesophageal junction area rather more adequately. We now begin the open operation with this a part of the process and carry out it in an similar method as the laparoscopic approach. Palpation and upward stress of the mesentery from behind the abdomen facilitates creating the opening within the mesentery adjacent to the stomach. However, if the intraoperative methylene blue check has shown a leak that wanted repair, or if the standard of the tissue or the anastomosis is at all doubtful, or for these extremely technically difficult operations the place visualization was just barely optimal, then in those situations the patient is treated in a fashion to prophylactically anticipate a possible leak. If the gastrojejunostomy is of concern, a closed-suction drain is left adjoining to it, placed simply inferior to it and coursing behind the spleen and out by way of the left ank. A distal gastrostomy is also placed during di cult open operations or converted operations where problems may have arisen. A standard Stamm-type gastrostomy with a 28- to 32-size tube is created to entry and drain the distal abdomen. Major aspects of this protocol are as follows: Intravenous isotonic uids are given at a price of 250 mL/h for the rst 12�24 hours and adjusted as wanted based on urine output. While many authorities have written that such a postoperative study is inaccurate and cost-ine ective,forty one we nonetheless use it to detect any potential issues of obstruction distal to the anastomosis and to doc gastric pouch size. Pain control is achieved by way of a combination of intravenous medications graduated to oral medicines by the rst postoperative day. Intravenous antibiotics are stopped after a postoperative dose in addition to the preoperative dose. Wound care is simpli ed by the Dermabond, which permits wounds to be uncovered to water if wanted. Oxygen is equipped the rst 24 hours after which eliminated as appropriate based mostly on oxygen saturation levels.
Oratane 10 mg without prescriptionIf not potential, the stone can be removed by way of an enterotomy made in a nonedematous segment of bowel. If one or multiple diverticula seem in amed or scarred, segmental resection of the concerned bowel with a main anastomosis is remitted. However, many sufferers often have a number of diverticula over a protracted stretch of bowel, and thus, if no evidence of in ammation or scarring is current, no resection is indicated. Upper and lower endoscopies are sometimes negative, and the diagnosis is made with angiographic and radioactive pink blood cell studies. Although therapy with angiographic embolization has been documented, segmental bowel resection is incessantly the required therapy. It is typically 644 Part V Intestine and Colon situated on the antimesenteric border of the small bowel inside 100 cm of the ileocecal valve. A symptomatic Meckel diverticulum can present in both the pediatric and adult population; the frequency of presentation decreases with growing age. In the adult inhabitants the most common shows are bleeding (38%), obstruction (34%), and diverticulitis (28%). In the pediatric population the most common shows are obstruction (40%), bleeding (31%), and diverticulitis (29%). Bleeding in the setting of a Meckel diverticulum is believed to result from acid secretion from ectopic gastric mucosa resulting in ulceration of and subsequent bleeding from adjacent ileal mucosa. A technetium-99m pertechnetate scan is the most typical and correct noninvasive study used to consider the presence of a Meckel diverticulum. Studies have found technetium-99m pertechnetate scans to be highly sensitive and speci c in each the pediatric and grownup populations. If suspicion is high, other etiologies have been ruled out, and noninvasive diagnostic instruments exhausted, exploratory laparoscopy could additionally be required to diagnose and treat an advanced Meckel diverticulum. Options for resection embody a diverticulectomy or a segmental bowel resection with a primary anastomosis. If diverticulitis is present, the road of resection should be freed from in ammation. Amputation ought to be carried out in a transverse orientation and might make the most of a surgical stapling device. Alternatively, the diverticulum may be resected between bowel clamps and the defect sutured closed in two layers, utilizing a steady internal layer of 3-0 Vicryl or chromic suture adopted by an outer layer of 3-0 silk Lembert sutures. Such situations embrace the presence of diverticulitis or palpable ectopic tissue on the diverticular-intestinal junction. Some authors argue that certain asymptomatic patients are extra doubtless to develop signs and thus recommend resection of an by the way detected diverticulum in a patient who ful lls any of the following standards: (1) youthful than 50 years, (2) male sex, (3) diverticulum higher than 2 cm in length, and (4) ectopic or irregular features inside a diverticulum. In this research, the chance of postoperative issues, including an infection and intestinal obstruction, was signi cantly larger following resection than leaving the diverticulum in situ (5. Commentaria cum Amplissimus Additionibus Super Anatomia Mundini Una cum Texta Ejusudem in Pristinum et Verum Nitorem Redanto. Of an inguinal rupture, with a pin within the appendix caeci, incrusted with stone, and a few observations on wounds within the guts. Perforating in ammation of the vermiform appendix; with special reference to its early prognosis and remedy. Studies within the etiology of acute appendicitis: the signi cance of the construction and performance of the vermiform appendix in the genesis of appendicitis. Balancing the conventional appendectomy rate with the perforated appendicitis fee: implications for quality assurance. Role of sequential leucocyte counts and C-reactive protein measurements in acute appendicitis. Role of Alvarado rating in diagnosis and therapy of suspected acute appendicitis. A potential trial of computed tomography and ultrasonography for diagnosing appendicitis in the atypical patient [see comment]. E ect of computed tomography of the appendix on treatment of patients and use of hospital assets. Ultrasonography and limited computed tomography in the analysis and administration of appendicitis in children. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Appendicitis in being pregnant with changes in place and axis of the conventional appendix in pregnancy. Ultrasonographic ndings after conservative treatment of acute appendicitis and open appendicectomy. Randomized medical trial of antibiotic therapy versus appendectomy as major treatment of acute appendicitis in unselected sufferers. Nonoperative remedy of suspected appendicitis in distant medical care environments: 646 Part V Intestine and Colon one hundred and one. Histopathologic analysis of interval appendectomy specimens: support for the role of interval appendectomy. Can interval appendectomy be justi ed following conservative remedy of perforated acute appendicitis Nonsurgical therapy of appendiceal abscess or phlegmon: a scientific evaluate and meta-analysis. Appendiceal tumors: retrospective clinicopathologic evaluation of appendiceal tumors from 7,970 appendectomies. Primary neoplasms of the appendix: radiologic spectrum of disease with pathologic correlation [erratum appears in Radiographics 2003;23:1340]. Primary malignant neoplasms of the appendix: a population-based research from the surveillance, epidemiology and end-results program, 1973�1998. Conservative management of perforated duodenal diverticulum: a case report and review of the literature. A Danish multicenter examine: cefoxitin versus ampicillin + metronidazole in perforated appendicitis. Systematic evaluate of randomized managed trials comparing laparoscopic with open appendicectomy. Laparoscopy reduces pointless appendicectomies and improves analysis in fertile girls. Invagination of the appendiceal stump for the discount of peritoneal bacterial contamination. Appendicectomy: assessment of stump invagination versus simple ligation: a potential, randomized trial. Evidence-based value of prophylactic drainage in gastrointestinal surgical procedure: a scientific evaluate and meta-analysis. Prospective randomized trial of two wound management methods for dirty stomach wounds. An extended retroperitoneal abscess brought on by duodenal diverticulum perforation: report of a case and quick review of the literature.
Buy generic oratane on lineAlthough most anorectal abscesses originate within the anal crypts, different disease entities must be considered if the pathology appears atypical. Endorectal advancement ap restore of rectovaginal and other sophisticated anorectal stulas. Tuberculosis is now a rare explanation for anal abscesses and stulas but has just lately been noticed in immigrants to America. Close examination, nevertheless, will reveal that the illness arises from the perianal skin and never the anal crypts. Actinomycosis should be suspected if typical sulfur-like granules are seen in the abscess cavity or stula tract. Hair obtained from the abscess cavity when the pilonidal abscess is drained will point out the true nature of the disease. Genital-anal, oral-anal, and different anal-based practices amongst gay or bisexual males and amongst girls who engage in anal receptive intercourse account for the transmission of most of those diseases. A high prevalence of histologically con rmed dysplasia in these inner lesions may be detected in asymptomatic gay men. Types 16 and 18 have been found in cervical cancer and high-grade cervical dysplasia, and type sixteen has been present in high-grade anal dysplasia and invasive cancers. It is most likely going that the progression price is low, however further research is required for documentation. Wide local excision could end in morbidity including anal stenosis or incontinence. Chlamydial proctitis might coexist with other rectal infections, especially gonorrhea. Several serotypes are liable for proctitis, and serotypes L1, L2, and L3 are responsible for lymphogranuloma venereum. Infection may be asymptomatic or might encompass nonspeci c signs such as anal ache, pruritus, purulent discharge, and bleeding. Perianal stulas and rectovaginal stulas might develop, with untreated cases progressing to severe rectal stricture. Two weeks after the initial signs, inguinal lymphadenopathy turns into predominant and the inguinal nodes might fuse collectively in a large mass. A biopsy of the rectal mucosa might be probably the most generally used technique to con rm the analysis. Unfortunately, a continual relapsing course is widespread, though recurrent lesions are usually much much less painful. Primary or initial infections are treated with oral acyclovir, famciclovir, or valacyclovir for 7�10 days. Chronic suppressive remedy or selfinitiation of antiviral therapy with recurrent episodes may be useful in sufferers with more than six recurrences per 12 months. Even after the lesions have completely healed, a condom should be used throughout sexual intercourse. All patients with con rmed rectal gonorrhea should have a serologic test for syphilis three months after therapy is accomplished. Syphilis e traditional lesion of primary syphilis is a chancre on the genitalia, however in homosexual males the chancre often presents in the anal canal or at the anal verge. Classic descriptions indicate that the syphilitic chancre is a painless lesion, however anal chancres may be extremely painful. Early syphilis may be diagnosed by examining scrapings from the bottom of the chancre with dark- eld microscopy; these lesions teem with spirochetes that could be seen as corkscrew-shaped motile uorescent yellowish-green organisms. Rapid plasma reagin and darkish eld microscopy are the appropriate checks for suspected early syphilis. It could present as condyloma latum, a pale-brown or esh-colored at verrucous lesion, or as a mucocutaneous rash. Patients with syphilis must abstain from sexual contact until therapy is complete. All sexual contacts inside the previous 90 days must be prophylactically treated. Gonorrhea Anorectal infections brought on by the bacterium Neisseria gonorrhoeae are widespread within the male gay population and frequently accompany different venereal ailments. Over half of gay males seen in screening clinics have been discovered to be contaminated, with the rectum being the one site infected in about half of instances. Untreated rectal gonorrhea can lead to septic arthritis, endocarditis, perihepatitis, and meningitis, as properly as infection of sexual companions. Several drugs (penicillin, tetracycline, ampicillin, and spectinomycin) could additionally be used for treatment, although growing numbers of resistant strains are being acknowledged. Fecal Incontinence Quality of Life Scale: quality of life instrument for sufferers with fecal incontinence. Balloon expulsion test facilitates prognosis of pelvic oor outlet obstruction because of nonrelaxing puborectalis muscle. Anorectal perform in patients with defecation disorders and asymptomatic topics: evaluation with defecography. High-resolution three-dimensional endovaginal ultrasonography in the evaluation of pelvic oor anatomy: a preliminary examine. Benign Anorectal Diseases: Diagnosis With Endoanal and Endorectal Ultrasound and New Treatment Options. One hundred circumstances of anal ssure handled with botulin toxin: early and long-term results. Total anal sphincter saving method for stulain-ano; the ligation of intersphincteric stula tract. Outcomes of primary repair of anorectal and rectovaginal stulas utilizing the endorectal advancement ap. Evaluation of recent anti-infective drugs for the remedy of genital infections as a outcome of herpes simplex virus. Dynamic magnetic resonance imaging defecography: a diagnostic alternative within the evaluation of pelvic oor disorders in proctology. Randomized, managed trial of biofeedback with anal manometry, transanal ultrasound, or pelvic oor retraining with digital steerage alone in the treatment of gentle to moderate fecal incontinence. Manometric squeeze strain di erence parallels functional outcome after overlapping sphincter reconstruction. Factors associated with percutaneous nerve analysis and everlasting sacral nerve modulation outcome in patients with fecal incontinence. Sacral nerve stimulation is extra e ective than optimum medical therapy for extreme fecal incontinence: a randomized, managed examine. Factors related to failure of the arti cial bowel sphincter: a study of over 50 cases from Cleveland Clinic Florida.
Discount oratane 5mg overnight deliveryInvasive carcinoma is present in 5% of all adenomas, but the incidence correlates with the dimensions and type of the adenoma (Table 36-9). Dysplasia is a term used to describe the intervening state between regular tissue and invasive malignancy. Intuitively, polyps with a larger mass have a larger volume of neoplastic cells, and therefore a better chance of harboring cancer. Prognostic components in colorectal carcinomas arising in adenomas: Implications for lesions eliminated by endoscopic polypectomy. Pedunculated polyps: stage 0-not invasive carcinoma; degree 1-invasion to the top of the pedunculated polyp; stage 2-invasion to the neck of the pedunculated polyp; level 3-invasion to the stalk of the pedunculated polyp; level 4-invasion to the base of the pedunculated polyp. A similar, however less well-known, classi cation was developed in 1993 by Kudo and associates, who for prognostic purposes instructed to divide the submucosal invasion of sessile malignant lesions into three ranges (Sm1, Sm2, Sm3). A hamartomatous polyp is composed of a spectrum of di erent cellular elements and is considered a nonneoplastic entity with no signi cant premalignant potential. Sm1-invasion into higher third of submucosa; Sm2-invasion into middle third of submucosa; Sm3-invasion into lower third of submucosa. Surgical administration of early Chapter 36 Tumors of the Colon 743 intestinal and extraintestinal disease, and several additionally impose an elevated chance of creating intestinal cancer as a outcome of immature glandular elements in the hamartomatous polyp. Stable estimates of this danger are di cult to calculate because of the relative rarity of those illnesses. Hyperplastic polyps are small, sessile mucosal outgrowths that display an exaggerated crypt structure. Histologically, hyperplastic polyps show well-formed glands and crypts which would possibly be lined by nonneoplastic epithelial cells. Because of their small dimension, hyperplastic polyps are usually clinically silent, but large or a number of hyperplastic polyps sometimes can be liable for gastrointestinal signs. Historically, hyperplastic polyps have been thought-about is paradigm has been benign and never premalignant. In ammatory polyps are the results of reactive regenerative processes occurring in or next to a damaged epithelium. Histologically, a combination of distorted crypt structure at the side of granulation tissue and in ammatory in ltrates is attribute. In an e ort to quantify the scientific severity/importance of dysplasia, nevertheless, the diploma of dysplasia is categorized and reported in three grades. Common phrases for polyps include low-grade dysplasia, intermediate-grade dysplasia, and high-grade dysplasia (by some additionally referred to as in situ [Tis] adenocarcinoma). Once there are clear microscopic options of tumor invasion through the muscularis mucosa of the colorectum, an invasive most cancers (T1 or greater) is current. First, a polyp may not be resectable because of dimension, attachment to bowel wall, or other causes associated to the anatomy of the affected person or polyp. In these situations, a careful assessment of the risks of surgical resection versus observational management is warranted, as 12�18% of these polyps harbor an 744 Part V Intestine and Colon invasive malignancy. When invasive cancer is found in a polyp, the administration relies mainly on the level of invasion and the completeness of the polypectomy. Based on the endodermal glandular tissue origin, adenocarcinoma and its histologic variants are by far the predominant histopathology and account for 90�95% of all colorectal malignancies. Colorectal most cancers (adenocarcinoma) is essentially the most frequent malignancy of the gastrointestinal tract, the fourth most frequently diagnosed malignancy, and the fourth commonest cause of cancer-related mortality on the planet. Macroscopically, most colorectal cancers have both a polypoid or an ulcerative-in ltrating look, but combos are frequent. Very hardly ever, colorectal most cancers might have a dissolute development pattern and resemble linitis plastica of the stomach, in which case a metastatic lesion from another primary site (eg, lobular breast most cancers, abdomen cancer) or a nonepithelial neoplasia (eg, lymphoma, carcinoid) would need to be dominated out. Adenocarcinoma, the exceedingly predominant histopathology of colon cancer, has a much less frequent variant of mucinous adenocarcinoma that features signet ring cell carcinoma and accounts for roughly 10% of all colorectal cancers. Compared to nonmucinous colon cancers, mucinous carcinomas normally present at a more advanced stage and thus have an overall poorer prognosis. Tumor dissemination primarily happens through access to the lymphatic vessels into the locoregional lymph nodes or through entry to the blood stream as hematogenous metastasis to distant organs. In addition, tumor dissemination can occur by transperitoneal seeding and result in peritoneal carcinomatosis. Growth by perineural in ltration could additionally be seen on microscopic examination and has a unfavorable prognostic influence. Additional modi ers are used to re ect the method of stage determination (p for pathology, c for scientific, u for ultrasound), and y to point out a standing after neoadjuvant therapy. Historical classi cations similar to Dukes and Astler-Coller are still sporadically in use but largely have been and should be deserted. Lipomas are submucosal lesions that develop within the fth or sixth decade of life and are extra frequent within the giant than in the small intestine. Whereas solitary lipomas are most likely to occur extra regularly on the proper facet of the colon within the vicinity of the ileocecal valve or the ascending colon, lipomatous polyposis might di usely contain the whole small and huge gut. Occasionally, when lipomas become massive sufficient to protrude into the lumen, they might cause symptoms such as gastrointestinal bleeding, diarrhea, intussusception, or bowel obstruction. Surgery could additionally be required if such a complication happens; it should therefore be thought-about preemptively for very large symptomatic lipomas. Alternatively, the mucosa overlying the lipoma may be opened endoscopically to allow the lipoma to spontaneously enucleate into the lumen. Modern nomenclature classi es carcinoids as neuroendocrine tumors, based on their neuroendocrine origin. In absence of different de nite indicators for malignant conduct, carcinoids smaller than 1 cm are thought-about benign, lesions bigger than 2 cm are probably malignant, and the grey zone in between stays undetermined or doubtlessly malignant. Diagnosis of a carcinoid may be suspected clinically however may be di cult to con rm histologically short of a surgical resection because the lesions are submucosal and never generally in attain of an endoscopic biopsy. Cross-sectional imaging and somatostatin receptor scintigraphy are instruments to consider for systemic disease. Multicentricity and related high charges of synchronous gastrointestinal and genitourinary malignancies warrant each an upper and lower gastrointestinal endoscopy. Tumors of smaller than 1 cm dimension could additionally be managed regionally, whereas the management of lesions measuring 1�2 cm stays controversial. Distinction from different mesenchymal tumors (eg, leiomyosarcoma) is necessary from a prognostic perspective. Tumor dimension and lightweight microscopic determination of the mitotic fee (mitotic gures per x number of high-power elds) are the most e necessary standard prognostic indicators. Recurrent and regionally superior or metastatic tumors are handled more and more with imatinib in a palliative, adjuvant, or neoadjuvant setting. Immunocompetent sufferers normally are asymptomatic, and the nodular lymphoid hyperplasia is an incidental nding. Nodular lymphoid hyperplasia has been associated with an increased subsequent incidence of lymphoma (small bowel).
References - Carlton CE Jr, Guthrie AG, Scott R Jr: Surgical correction of ureteral injury, J Trauma 9:457, 1969.
- Welch AJ, Torres JH, Cheong WF: Laser physics and laser-tissue interaction, Tex Heart Inst J 16:141-149, 1989.
- Brenner BM, Lawler EV, Mackenzie HS: The hyperfiltration theory: a paradigm shift in nephrology, Kidney Int 49(6):1774n1777, 1996.
- Blanco Munoz J, Lacasana M, Borja Aburto VH: Maternal miscarriage history and risk of anencephaly, Paediatr Perinat Epidemiol 20(3):210n218, 2006.
- Creighton G, Oliffe JL: Theorising masculinities and menis health: a brief history with a view to practice, Health Sociol Rev 19:409n418, 2010.
|
|

