"Cheap clomid 50 mg otc, menstruation 1 month."By: Keira A Cohen, M.D. - Co-Director, The Johns Hopkins Center for Nontuberculous Mycobacteria and Bronchiectasis
- Assistant Professor of Medicine
 https://www.hopkinsmedicine.org/profiles/results/directory/profile/10003818/keira-cohen
Buy clomid 100 mgHistologic research of the esophagus in beforehand irradiated patients have demonstrated epithelial thickening, persistent irritation, and fibrosis of the submucosa and muscularis propria, however rarely chronic ulceration. Barium swallow examination could show strictures and disruption of peristalsis on the degree of the irradiated esophagus, with repetitive and nonperistaltic waves above and under the irradiated area. Abnormal peristalsis has been reported at 1 to 3 months following treatment completion, whereas most strictures happen four to 8 months following therapy completion. Cumulatively, it is suggested that the imply esophageal dose be saved beneath 34 Gy, while limiting portions of the esophagus handled to more than 60 Gy. The 1-year actuarial fistula formation fee was 18%, and the authors really helpful caution in using this strategy, significantly along side concurrent chemotherapy. Hyperfractionation (multiple daily radiation treatments) was additionally related to elevated acute toxicity. Twenty-six % of sufferers receiving concurrent chemoradiotherapy developed grade three or greater esophageal toxicity, whereas only one. Severe acute toxicity was predicted by means of twice-daily radiation, older age, rising nodal stage, and a variety of dosimetric parameters. The overall incidence of late toxicity was 7%, with a median and maximal time to onset of 5 and 40 months, respectively. Radioprotective chemical brokers have been investigated as a means of mitigating radiation-induced normal tissue toxicity. This agent is a scavenger of free radicals and serves as an alternative goal to nucleic acids for alkylating or platinum brokers. Patients receiving amifostine, however, skilled considerably greater rates of nausea, vomiting, an infection, febrile neutropenia, and cardiac events. A retrospective study in forty one sufferers with lung carcinoma demonstrated that glutamine was nicely tolerated, with supplemented patients experiencing a lower incidence of grade 2 to 3 esophagitis, usually resulting in weight achieve throughout therapy. Glutamine was associated with less grade three esophagitis, treatment breaks, and weight loss, and administration was not associated with variations in time to occasion finish factors. The management of late esophageal radiation stricture consists of serial endoscopic dilatation for symptomatic improvement. Dilations in superior stricture may end up in esophageal rupture and therefore must be approached cautiously. Long-term use of gastric antisecretory drugs, as nicely as prokinetic brokers corresponding to metoclopramide, have been really helpful to decrease gastroesophageal reflux effects. Surgical intervention could also be required for sufferers who develop perforation or fistula. Finally, it is very important notice that the medical symptoms related to late radiation harm are sometimes difficult to distinguish from these brought on by recurrent or new main malignancies. Patients with strictures or ulcerations also needs to be evaluated to differentiate persistent radiation modifications from most cancers recurrence. Treatment interruptions may ease the symptoms of acute esophagitis, however may compromise remedy efficacy and is generally reserved for severe circumstances. Dietary modification, including bland meals, pureed or delicate meals, and soups, can help sufferers preserve oral consumption. Other modifications embrace avoidance of smoking, alcohol, espresso, spicy or acidic foods, chips, crackers, and fatty meals. A research of dietary modifications and pharmacologic prophylaxis for radiation-induced esophagitis reported decreased toxicity and fewer treatment interruptions. It was recommended to drink between meals and to eat 6 smaller meals per day, consisting of semisolid meals, soup, high-calorie dietary supplements, purees, puddings, milk, and gentle breads. Radiation to the abdomen in animals using a very excessive single dose leads to erosive and ulcerative gastritis. A barely lower single dose (23 Gy) leads to gastric dilatation and gastroparesis, with substitute of the normal gastric mucosa by hyperkeratinized squamous epithelium. With even decrease doses, gastric Chapter forty RadiationInjury 667 obstruction occurring months after irradiation was observed, with an atrophic gastric mucosa and intestinal metaplasia seen in surviving animals. Even with a relatively low dose of 18 Gy delivered in 10 fractions, roughly 40% of ulcer sufferers had a 50% discount in gastric acid secretion that lasted for a yr or extra. Histologic changes could embrace disappearance of cytoplasmic details and granules in parietal and chief cells as early as 1 week into remedy. Cell damage and subsequent cell death are often seen first in the depths of glands, followed by thinning of the gastric mucosa. Loss of glandular architecture and thickening of the mucosa can be seen by the third week of radiotherapy. Approximately 3 weeks after completing radiotherapy, histologic recovery may be seen. Signs of recovery of early radiation damage to the stomach embrace re-epithelialization and fibrosis. Symptoms of acute radiation damage of the stomach consist primarily of nausea and vomiting, dyspepsia, anorexia, belly ache, and malaise. Radiationinduced nausea and vomiting might happen inside the first 24 hours following therapy. It is estimated that roughly half of patients receiving higher stomach radiation will experience emesis within 2 to 3 weeks following radiation initiation. Perforation charges had been 2% and 14% after doses of under 50 Gy and 50 Gy or above, respectively. Symptomatic gastritis occurred roughly 2 months following radiation completion, with ulcer formation occurring at a median of 5 months. Six of 233 sufferers (3%) required surgery for ulcer hemorrhage or ache associated to ulcer disease, almost all of whom had received doses of greater than 50 Gy. Patients who acquired doses greater than 50 Gy experienced gastric ulceration and gastric ulcer�associated perforation at rates of 15% and 10%, respectively. Of the 7 sufferers enrolled, three experienced gastric or duodenal ulcers with extreme bleeding, requiring transfusion. Patients receiving dexamethasone showed a pattern toward improved full control of nausea (50% vs. The authors concluded that the addition of dexamethasone resulted in modest improvement in protection in opposition to radiation-induced emesis. Careful nutritional help together with antiemetic therapy is important for patients present process radiotherapy to the abdomen. With extra extreme complications of bleeding, ulceration, gastric outlet obstruction, fistula formation, or perforation, sufferers may require endoscopic therapeutic approaches or rarely surgical intervention with partial gastrectomy. The small bowel could be damaged during radiation treatment of malignances of the stomach, pancreas, rectum, anus, and through treatment of gynecologic cancers. Submucosal reaction shows massive, bizarre radiation fibroblasts that have both cytomegaly and nucleomegaly. Radiation-induced adjustments include thickening of the blood vessel partitions, subintimal hydropic change and fibrosis, which ends up in luminal narrowing and occlusion and subsequent tissue ischemia. Irradiation of intestinal mucosa primarily affects the clonogenic intestinal stem cells throughout the crypts of Lieberk�hn (cells that present, via self-replication and eventual maturation, alternative cells in the intestinal villi). Stem cell damage, because of direct radiation injury or radiation-induced microvascular damage, leads to a lower in mobile reserves for the intestinal villi. This results in mucosal denudement, shortened villi, decreased absorptive space, and associated intestinal inflammation and edema.
Cheap generic clomid canadaUnlike full agenesis of the pancreas, patients may be asymptomatic or might present with bile duct obstruction or pancreatitis. The earliest and most characteristic manifestation of this disease appears to be the passage of stool with an uncommon quantity of readily separable oil, which is commonly answerable for soiling. Failure to thrive is only often famous, and systemic manifestations are absent. Trypsin and amylase activity are considerably diminished in some sufferers, however different parameters of exocrine perform (including colipase and phospholipase A actions, bicarbonate and quantity secretion) are usually regular. Any residual lipase exercise has been presumed to be a result of lingual or gastric lipase activity. In addition to its practical absence, no immunologically reactive lipase may be detected,392 suggesting either the entire absence of pancreatic lipase or the incidence of a serious structural change affecting each immunogenicity and performance. The response to exogenous pancreatic enzyme remedy is suboptimal, and limitation of dietary fat is usually essential to keep away from oily stools and incontinence. Congenital enterokinase deficiency is recognized in 1% to 2% of infants undergoing analysis of suspected pancreatic insufficiency. However, even in untreated celiac disease, normal mucosal and regular intraluminal enterokinase activities have been reported. Colipase exercise is markedly lowered, with otherwise regular pancreatic enzyme secretion. Fat absorption improves dramatically with the intraduodenal instillation of purified colipase. Hypertriglyceridemia can be seen in inherited familial mixed hyperlipidemia, familial hypertriglyceridemia, remnant elimination illness (type 3 dyslipidemia), and apolipoprotein A5 deficiency. Both kindreds had autosomal dominant diabetes mellitus, sometimes identified earlier than the age of forty years. All mutation carriers had low fecal elastase ranges, and all 10 topics tested had a low coefficient of fat absorption and decreased fat-soluble vitamin ranges. Evaluation included regular amylase and lipase activities but very low trypsin exercise in the duodenum, with regular concentrations of Chronic Pancreatitis the relationship between familial hyperlipidemias and chronic pancreatitis is advanced. Chronic pancreatitis was seen in an prolonged Dutch kindred of sufferers with genetically deficient lipoprotein lipase catalytic exercise. Detection, evaluation and therapy of diabetes mellitus in chronic pancreatitis: Recommendations from PancreasFest 2012. Whole exome sequencing identifies a quantity of, advanced etiologies in an idiopathic hereditary pancreatitis kindred. A methods biology method to genetic research of pancreatitis and different complex ailments. Mutations in the cationic trypsinogen gene are associated with recurrent acute and chronic pancreatitis. Chronic alcohol consumption accelerates fibrosis in response to ceruleininduced pancreatitis in rats. Chronic alcohol consumption accelerates fibrosis in response to ceruleininduced pancreatitis in the rat. Progressive disruption of acinar cell calcium signaling is an early feature of cerulein-induced pancreatitis in mice. The role of intracellular calcium signaling in untimely protease activation and the onset of pancreatitis. Bile acids induce calcium signals in mouse pancreatic acinar cells: Implications for bile-induced pancreatic pathology. Ethanol food plan increases the sensitivity of rats to pancreatitis induced by cholecystokinin octapeptide. Trypsinogen copy number mutations in sufferers with idiopathic chronic pancreatitis. An elevated ratio of serum anionic to cationic trypsinogen might signal pancreatic illness. Cloning and characterization of an extracellular Ca(2+)-sensing receptor from bovine parathyroid. Molecular and useful identification of a Ca2+ (polyvalent cation)sensing receptor in rat pancreas. Novel mutations within the calcium sensing receptor gene in tropical persistent pancreatitis in India. Immunohistochemical research of secretory proteins within the creating human exocrine pancreas. Pancreatic aspects of cystic fibrosis and other inherited causes of pancreatic dysfunction. Identification of widespread cystic fibrosis mutations in African-Americans with cystic fibrosis will increase the detection price to 75%. Pancreatitis in Hispanic patients with cystic fibrosis carrying the R334W mutation. Genotype and phenotype correlations in patients with cystic fibrosis and pancreatitis. Mutations within the cystic fibrosis transmembrane regulator gene and in vivo transepithelial potentials. Analysis of risk components for the event of liver illness related to cystic fibrosis. Relation between mutations of the cystic fibrosis gene and idiopathic pancreatitis. Re: Ockenga et al-Mutations of cystic fibrosis gene in sufferers with pancreatitis. The Shwachman-Bodian-Diamond syndrome protein mediates translational activation of ribosomes in yeast. Shwachman-Bodian Diamond syndrome is a multi-functional protein implicated in cellular stress responses. Pluripotent stem cell models of Shwachman-Diamond syndrome reveal a common mechanism for pancreatic and hematopoietic dysfunction. Mutations in the gene encoding the serine protease inhibitor, Kazal sort 1 are related to continual pancreatitis. Elevated pancreatic secretory trypsin inhibitor levels throughout extreme inflammatory illness, renal insufficiency, and after various surgical procedures. Mechanisms of disease: Advances in understanding the mechanisms leading to chronic pancreatitis. Lipopolysaccharide-activated macrophages stimulate the synthesis of collagen kind I and C-fibronectin in cultured pancreatic stellate cells. Lowe, Increasing incidence of acute pancreatitis at an American pediatric tertiary care heart: Is larger awareness among physicians accountable A comparability of presentation and management developments in acute pancreatitis between infants/toddlers and older youngsters.
Diseases - Oculodentodigital dysplasia dominant
- Median nodule of the upper lip
- Hyperimmunoglobulinemia D with periodic fever
- Homologous wasting disease
- M?nchausen syndrome
- Char syndrome
- Microcephaly with normal intelligence, immunodeficiency
- Orstavik Lindemann Solberg syndrome
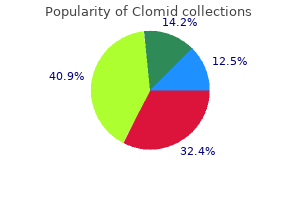
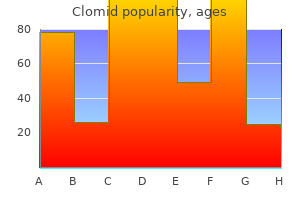
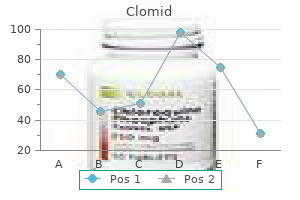
Cheap clomid 50 mg otcMost research recommend a sensitivity of 50% to 80% with a specificity of 80% to 90%. Some analyses suggest that simply assessing fluid quantity after secretin stimulation, instead of bicarbonate focus, is simply too inaccurate to be clinically helpful. These had been developed at an international consensus conference held greater than 20 years ago. The pancreatic duct abnormalities characteristic of chronic pancreatitis may be seen in different situations as nicely. Although pancreatic operate is well preserved in aging, impressive abnormalities could develop in the pancreatic duct. They embrace focal or diffuse dilatation of the main pancreatic duct and its facet branches, the development of cystic cavities, and even ductal calculi. In 1 examine, seventy four postmortem pancreatograms had been submitted to 6 skilled endoscopists. In the remaining 69 topics, there was no histologic evidence of continual pancreatitis. Depending on the observer, between 42% and 98% of those pancreatograms have been read as demonstrating continual pancreatitis, largely primarily based on gentle abnormalities within the primary duct and facet branches. The mistaken interpretations had been felt to be because of age-related modifications inside the pancreas. Another research tried to estimate intraobserver variability by submitting 51 pancreatograms to four skilled endoscopists on 3 separate events. The standard diagnostic system is predicated on the presence of abnormalities within the pancreatic duct and the parenchyma (Table 59-5). These features may be individually categorised as none, minimal, moderate, or extensive but in follow are generally only graded as current or absent, and the entire variety of features is used because the score (maximum score, 9). The sensitivity and specificity of the check is set by the edge whole rating used to define persistent pancreatitis. This was developed via skilled consensus and includes main and minor standards, with an try to provide semiquantification of severity. These subtle findings are generally not enough for a definitive prognosis of continual pancreatitis. The settlement between these exams varies widely in these research, ranging from 10-90%. The edema associated with a recent episode of acute pancreatitis could make duct margins and intralobular septa more apparent, which can reduce specificity. The markers on the dilated pancreatic duct (lower left) reveal hyperechoic margins, a diagnostic feature of continual pancreatitis. The parenchyma surrounding these markers demonstrates hyperechoic strands and foci, that are additional options of persistent pancreatitis. Resolution of this issue would require very long follow-up of patients, given the dearth of a helpful gold standard. Diagnostic Strategy the diagnosis of chronic pancreatitis is most often suspected due to the presence of an stomach pain syndrome, and less commonly because of a suspicion of exocrine (diarrhea, steatorrhea, weight loss) or endocrine insufficiency (diabetes mellitus). If the diagnosis stays doubtful, follow-up over time with periodic reassessment may be the solely diagnostic method. Although this strategy may be useful in managing pancreatic carcinoma pain, it sometimes leads only to greater dependence in patients with persistent pancreatitis. Pain administration clinics that focus on non-narcotic approaches are most useful in patients with continual pancreatitis. Tramadol is a dual-action analgesic, with mu-opioid agonistic and monoaminergic properties. High dosages of tramadol are equal to oral morphine in treating painful continual pancreatitis, with fewer effects on gut motility. Adjunctive agents may additionally be considered in patients who need stronger narcotics. Many of those sufferers are depressed, and coexistent despair lowers pain threshold. Chronic pancreatic ache can result in abnormal spinal twine gating in nociceptive neurons, a centrally sensitized ache state, with hyperalgesia and allodynia. Finally, the gabapentoids (a2d subunit voltage-gated N-type calcium channel inhibitors) gabapentin and pregabalin are used in quite lots of persistent ache states as an adjunct to narcotics. In 1 randomized trial in sufferers with continual pancreatitis requiring narcotics for pain management, pregabalin reduced pain at a dosage of as much as 300 mg twice every day. Given the increasing recognition of neuropathic mechanisms of ache in continual pancreatitis, using most of these agents appears reasonable. The preliminary analysis of pain should concentrate on figuring out associated situations for which particular remedy exists. These conditions can embrace pancreatic pseudocyst, duodenal (and presumably bile duct) compression, superimposed pancreatic carcinoma, and gastroparesis. Cross-sectional imaging can be useful in identifying a few of these issues in addition to assessing for different diagnoses that might mimic continual pancreatitis. Identifying sufferers with big-duct continual pancreatitis and differentiating them from sufferers who lack these findings may be very useful in choosing therapy for pain. Most studies, but not all, have documented an obvious lower in pain or painful relapses in sufferers who stop consuming alcohol. In a summary of those studies, ache continued in 26% of abstinent patients, compared with 53% of those that continued to drink. Cessation of smoking appears to have even more advantages in each stopping tobacco-induced illness and in decreasing the risk of secondary pancreatic carcinoma. It is value stating that the placebo response in these patients is at least 20%. Strategies to decrease the risk of overuse of narcotics and of habit embrace having a single physician take responsibility for prescriptions, ongoing counseling, and common clinic visits. Some pain administration clinics treat all sufferers in the identical method, Chapter fifty nine ChronicPancreatitis 1015 Antioxidants Damage by free radicals has been proposed as 1 mechanism for pancreatic injury in alcoholic and different forms of chronic pancreatitis. Patients with persistent pancreatitis (particularly alcoholic) have evidence of oxidant stress and reduced antioxidant capability. This trial, which recruited subjects who have been relatively younger, underweight, and suffered from primarily idiopathic or tropical pancreatitis, used a combination of selenium, beta-carotene, vitamin C, vitamin E, and methionine. A second trial from the United Kingdom282 used higher dosages of the identical antioxidants however recruited a population that was older, not malnourished, and suffered from persistent pancreatitis mainly because of alcohol and smoking. This trial demonstrated no profit from antioxidant therapy, regardless of documentation of increased serum levels of these antioxidants. The use of pancreatic enzymes to scale back pain relies on the power of those brokers to activate this feedback management system in a approach to reduce pancreatic secretion. Delivering proteases to the duodenum or very proximal jejunum can suppress pancreatic secretion.
Purchase clomid 100mg on-lineAfter the tracings are accomplished, glucagon may be administered intravenously to decrease duodenal motility, and additional meperidine or fentanyl may be given for sedation to facilitate subsequent endoscopic therapy (see later). If a cholangiogram is desired, the aspirating port can be used for contrast injection. Station pull-through tracing obtained via a triplelumen catheter during sphincter of Oddi (biliary) manometry. This tracing is irregular and shows an elevated imply basal pressure of roughly 70 mm Hg as well as normal phasic contractions of the sphincter of Oddi. The phasic wave frequency, propagation course of waves, and amplitude of the waves can additionally be determined, though their scientific use has been deserted. Some uncontrolled research have suggested that more easily measurable criteria, corresponding to elevated liver enzyme levels and biliary dilatation, are superior for predicting a response to sphincter ablation. Some providers recommend a low-fat food plan for lowering pancreaticobiliary stimulation, though no data can be found to substantiate this approach. A trial of antispasmodics or a low-dose tricyclic antidepressant (to reduce visceral hypersensitivity) is often tried in these patients. Although this response rate is just like that in sham-treated controls, a true medical response probably happens in a couple of patients. Others, however, have offered this intervention to patients with a compelling scientific history, severe symptoms, and lack of response to medical therapy, provided the risks of the process are well understood by the affected person. Observational research have instructed that recurrent assaults of pancreatitis seem to be prevented by pancreatic sphincterotomy in 60% to 80% of patients with manometrically proved pancreatic sphincter hypertension. For the affected person with an intact gallbladder and unexplained pancreatitis, some authorities advocate either biliary sphincterotomy, remedy with ursodeoxycholic acid, or empirical cholecystectomy, with the implication that microlithiasis is the doubtless trigger (see Chapters fifty eight and 65). Perhaps the most probably clarification is that the pain was not of pancreaticobiliary origin but was caused instead by altered intestinal motility or visceral hypersensitivity. The role of residual pancreatic sphincter hypertension as a supply of continuous ache in the absence of pancreatic abnormalities is unclear. Some experts advocate initial twin sphincterotomies to forestall this downside, though the reintervention rate for persistent or recurrent pain has not been totally different from that for historic controls in whom a single sphincterotomy (of 1 duct) was carried out. Frequency of abnormal sphincter of Oddi manometry in contrast with the clinical suspicion of sphincter of Oddi dysfunction. The efficacy of endoscopic sphincterotomy after cholecystectomy in patients with sphincter of Oddi dysfunction. Manometry primarily based randomized trial of endoscopic sphincterotomy for sphincter of Oddi dysfunction. Evaluation of surgical outcomes and gallbladder traits in patients with biliary dyskinesia. Cholecystokinin cholescintigraphy: Detection of abnormal gallbladder motor perform in sufferers with persistent acalculous gallbladder illness. Role of quantitative cholescintigraphy for planning laparoscopic cholecystectomy in sufferers with gallbladder dyskinesia and continual belly pain. Systematic review and meta-analysis: Does gall-bladder ejection fraction on cholecystokinin cholescintigraphy predict outcome after cholecystectomy in suspected practical biliary ache Does gallbladder ejection fraction predict end result after cholecystectomy for suspected persistent acalculous gallbladder dysfunction Does gallbladder ejection fraction predict pathology after elective cholecystectomy for symptomatic cholelithiasis Surgical therapy for biliary dyskinesia: A meta-analysis and evaluation of the literature. Meta-analysis of cholecystectomy in symptomatic sufferers with constructive hepatobiliary iminodiacetic acid scan outcomes with out gallstones. The treatment of gallbladder dyskinesia primarily based upon signs: Results of a 2-year, prospective, nonrandomized, concurrent cohort examine. Increased sphincter of Oddi basal strain in sufferers affected by gall stone disease: A position for biliary stasis and colicky pain Gallbladder ejection fraction and its relationship to sphincter of Oddi dysfunction. Incidence of persistent signs after laparoscopic cholecystectomy: A prospective study. Biliary tract complications after orthotopic liver transplantation with choledochocholedochostomy anastomosis: Endoscopic findings and results of remedy. Long-term follow-up of endoscopic retrograde cholangiopancreatography sphincterotomy for sufferers with acquired immune deficiency syndrome papillary stenosis. Sphincter of Oddi dysfunction in sufferers hooked on opium: An unrecognized entity. Beneficial effect of lovastatin on sphincter of Oddi dyskinesia in hypercholesterolemia and hypertriglyceridemia. The utility of liver perform test abnormalities concomitant with biliary symptoms in predicting a good response to endoscopic sphincterotomy in sufferers with presumed sphincter of Oddi dysfunction. Hybrid classification of sphincter of Oddi dysfunction based on simplified Milwaukee standards: Effect of marginal serum liver and pancreas check elevations. Delayed biliary drainage is widespread in asymptomatic post-cholecystectomy volunteers. A noninvasive test of sphincter of Oddi dysfunction in postcholecystectomy patients: the scintigraphic score. Scintigraphy versus manometry in patients with suspected biliary sphincter of Oddi dysfunction. Comparison of sphincter of Oddi manometry, fatty meal sonography, and hepatobiliary scintigraphy within the prognosis of sphincter of Oddi dysfunction. Comparison of ultrasound-secretin check and sphincter of Oddi manometry in sufferers with recurrent acute pancreatitis. Comparison of secretin-stimulated magnetic resonance pancreatography and manometry leads to sufferers with suspected sphincter of Oddi dysfunction. Dynamic imaging of the pancreas utilizing real-time endoscopic ultrasonography with secretin stimulation. Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in sufferers with sphincter of Oddi dysfunction. Biopsies of the ampullary region in patients suspected to have sphincter of Oddi dysfunction. A controlled examine of the effect of midazolam on abnormal sphincter of Oddi motility. Sphincter of Oddi manometry: Decreased danger of scientific pancreatitis with use of a modified aspirating catheter. Reduced danger for pancreatitis after endoscopic microtransducer manometry of the sphincter of Oddi: A randomized comparison with the perfusion manometry method. Discordance of strain recordings from biliary and pancreatic duct segments in sufferers with suspected sphincter of Oddi dysfunction. Pressure measurements from biliary and pancreatic segments of sphincter of Oddi: Comparison between patients with useful belly ache, biliary, or pancreatic disease. Clinical options, manometric findings and endoscopic therapy leads to group I patients with sphincter of Oddi dysfunction.
Generic clomid 50 mg with amexCourse and end result of chronic pancreatitis: Longitudinal research of a combined medical-surgical collection of 245 patients. The completely different programs of early- and late-onset idiopathic and alcoholic continual pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the illness. A multidimensional case-control research of dietary, alcohol, and tobacco habits in alcoholic males with persistent pancreatitis. Is it long-term steady ingesting or the post-drinking withdrawal interval that triggers the first attack of acute alcoholic pancreatitis Associations of alcohol ingesting and nutrient intake with continual pancreatitis: Findings from a case-control research in Japan. Alcohol consumption, cigarette smoking, and body mass index in sufferers with alcohol-associated pancreatitis. Effect of alcohol and smoking on pancreatic lithogenesis in the course of chronic pancreatitis. Cigarette smoking will increase the danger of pancreatic calcification in late-onset however not earlyonset idiopathic continual pancreatitis. Epidemiology of alcohol-related liver and pancreatic disease within the United States. Alcoholic nonprogressive chronic pancreatitis: Prospective long-term research of a large cohort with alcoholic acute pancreatitis (1976-1992). Long-term follow-up after the first episode of acute alcoholic pancreatitis: Time course and risk factors for recurrence. Risk elements for recurrent acute alcohol-associated pancreatitis: A prospective analysis. Effect of cessation of alcohol use on the course of pancreatic dysfunction in alcoholic pancreatitis. Smoking cessation at the medical onset of continual pancreatitis and threat of pancreatic calcifications. Autoimmune pancreatitis: An replace on classification, analysis, pure history, and management. Prevalence of autoimmune pancreatitis and different benign disorders in pancreatoduodenectomy for presumed malignancy of the pancreatic head. Endoscopic retrograde cholangiopancreatography standards to diagnose autoimmune pancreatitis: An international multicenter examine. Clinical variations between mass-forming autoimmune pancreatitis and pancreatic cancer. Distinguishing autoimmune pancreatitis from pancreaticobiliary cancers: Current technique. Treatment of relapsing autoimmune pancreatitis with immunomodulators: the Mayo Clinic experience. Endoscopic measurement of papillary sphincter zone and pancreatic major ductal strain in sufferers with chronic pancreatitis. Endoscopic retrograde cholangiopancreatography and manometry findings in 1,241 idiopathic pancreatitis sufferers. Pancreatic operate after severe acute biliary pancreatitis: the position of necrosectomy. A prospective analysis of pancreatic exocrine operate in patients with acute pancreatitis: Correlation with extent of necrosis and pancreatic endocrine insufficiency. Comparative radiological and morphological research of human pancreas: Pancreatitis-like adjustments in postmortem ductograms and their morphological pattern. A multicenter research screening fecal elastase 1 concentrations in 1,021 diabetic patients. Alcohol consumption, cigarette smoking, and the risk of recurrent acute and persistent pancreatitis. Differences within the pure historical past of idiopathic (nonalcoholic) and alcoholic continual pancreatitis: A comparative long-term research of 287 patients. Use and perceived effectiveness of non-analgesic medical therapies for continual pancreatitis in the United States. Pattern of pain, duct morphology, and pancreatic perform in continual pancreatitis: A comparative study. The course of ache is similar in alcohol- and nonalcoholinduced persistent pancreatitis. Chronic pancreatitis: Long-term pain aid with or without surgical procedure, most cancers threat, and mortality. Pancreatic tissue fluid stress during drainage operations for chronic pancreatitis. Endoscopic manometry of the pancreatic duct and sphincter zone in sufferers with continual pancreatitis. Endoscopic remedy of the principle pancreatic duct: Correlation among morphology, manometry, and scientific follow-up. Endoscopic stent therapy in superior chronic pancreatitis: Relationships between ductal changes, medical response, and stent patency. Endoscopic measurement of pancreatic tissue perfusion in sufferers with chronic pancreatitis and control patients. Neural alterations in surgical stage continual pancreatitis are unbiased of the underlying etiology. Chronic pancreatitis: the angle of pain generation by neuro-immune interplay. Molecular and behavioral changes in nociception in a novel rat mannequin of chronic pancreatitis for the examine of pain. Pain in persistent pancreatitis: the role of reorganization of the central nervous system. Is altered central pain processing associated to disease stage in continual pancreatitis sufferers with ache Fat-soluble vitamins in sufferers with continual pancreatitis (pancreatic insufficiency). Fat-soluble vitamin focus in persistent alcohol-induced pancreatitis: Relationship with steatorrhea. The prevalence of fat-soluble vitamin deficiencies and decreased bone mass in sufferers with continual pancreatitis. Serum dietary markers for prediction of pancreatic exocrine insufficiency in continual pancreatitis. Bone mineral metabolism, bone mineral density, and body composition in sufferers with persistent pancreatitis and pancreatic exocrine insufficiency. Alterations of bone mineral density and bone metabolism in sufferers with varied grades of continual pancreatitis. Vitamin D3 in sufferers with numerous grades of persistent pancreatitis, in accordance with morphological and functional standards of the pancreas. Apoptosis and proliferation of acinar and islet cells in chronic pancreatitis: Evidence for differential cell loss mediating preservation of islet operate. Mechanisms and emerging therapy of the metabolic issues of persistent pancreatitis.
Syndromes - Lower risk of heart disease and obesity
- Nausea
- Household contacts and caregivers of children under the age of 6 months, including breastfeeding women
- Have you been sick or injured recently?
- Right-sided heart failure
- Delirium
Order clomid australiaIn patients with identified pseudocysts, new signs similar to abdominal pain, chills, or fever ought to alert the clinician to the emergence of an contaminated pseudocyst or abscess. Surgical drainage of a pseudocyst is feasible with a cystgastrostomy or cyst-duodenostomy if the pseudocyst wall is broadly adherent to the abdomen or duodenum, respectively. Other procedures embody a Roux-en-Y cyst-jejunostomy or pancreatic resection if the pseudocyst is within the tail. Percutaneous catheter drainage is effective treatment to drain and close sterile as well as infected pseudocysts. As mentioned in Chapter 61, there are 2 endoscopic strategies to decompress a pancreatic pseudocyst: (1) insertion of a stent via the ampulla directly into the pancreatic duct after which into the pseudocyst itself,311,312 or (2) an endoscopic cystgastrostomy or cyst-duodenostomy. Failure of percutaneous or endoscopic drainage of a pancreatic pseudocyst increases morbidity and prolongs hospitalization. However, most collection present longterm decision with successful endoscopic drainage of pseudocysts. An endoscopically positioned stent within the pancreatic duct might induce ductal adjustments equivalent to these of chronic pancreatitis. The determination that a affected person has pancreatic necrosis has scientific implications as a end result of the morbidity and mortality of necrotizing pancreatitis are higher than that of interstitial pancreatitis. Furthermore, treatment of sufferers with necrotizing pancreatitis differs from patients with interstitial pancreatitis. Patients with necrotizing pancreatitis may seem unwell with organ failure or might seem properly with no evidence of organ failure. For the primary week, pancreatic necrosis is often considered sterile and managed conservatively. At this time, the use of antibiotics to prevent an infection is questionable and not recommended (see earlier). Surgical d�bridement of sterile pancreatic necrosis has additionally been proven not to be useful in the overwhelming majority of patients. Infection of the pancreatic necrosis is believed to occur from translocation of bacteria from the colon. This discovering could help explain why enteral feeding, decreasing the pathogenic intestinal flora, prevents infection of necrosis. Infection of the pancreatic necrosis should be suspected when symptoms recur, especially indicators of sepsis, with fever, pain, and leukocytosis. The procedure is also secure, hardly ever introducing an infection into a sterile area in the abdomen. If negative, an aspiration could be repeated every four to 7 days if infection continues to be suspected. In the past, the prognosis of infected necrosis implied the pressing want for surgical d�bridement. In a persistently ill patient with sepsis or organ failure discovered to have contaminated necrosis, surgical d�bridement ought to be considered. However, in a stable patient with contaminated necrosis, maximal supportive care and the utilization of pancreatic-penetrating antibiotics must be supplied. It is in these patients that antibiotics similar to fluoroquinolones, metronidazole, and imipenem or meropenem ought to be administered. Alternatively, bleeding may be because of the inflammatory features of the pancreatitis (see Box 58-7). The latter is believed to occur from the irritative effects of liberated activated enzymes on vascular buildings or pressure necrosis of inflammatory debris or fluid collections on surrounding constructions. Temporizing remedies with interventional radiologic strategies are used, adopted by extra definitive surgical ligation and resection. Acute and chronic inflammatory processes of the pancreas can result in thrombosis of the adjoining splenic vein, which may lead to gastric varices, with or with out esophageal varices. Treatment of variceal rupture can be endoscopic, with banding of varices or splenectomy, which is healing. Rarely, bleeding into the pancreatic duct happens (hemosuccus pancreaticus), however this usually happens in persistent pancreatitis. Postnecrosectomy bleeding is widespread and can be brought on by overly aggressive d�bridement or the position or using noncompliant drainage tubes subsequent to vascular structures. Splenic Complications Splenic issues of pancreatitis embrace splenic pseudocysts, splenic vein thrombosis, infarction and necrosis of the spleen, splenic rupture, and hematoma. Bowel Compression or Fistulization Pressure necrosis from inflammatory particles from the tail of the pancreas can obstruct or fistulize into the small or large bowel. Respiratory insufficiency is the most common systemic complication related to pancreatitis. Oxygen supplementation, antibiotics, thoracentesis, and assisted ventilation could additionally be necessary. Renal failure is because of hypovolemia causing prerenal azotemia or to hypotension, typically Chapter 58 AcutePancreatitis 993 resulting in acute tubular necrosis. Shock is normally caused by hypovolemia secondary to third-space losses, vomiting, and interstitial pancreatic edema. Other unusual causes of hypotension include myocardial infarction and pericardial effusions. Fluid replacement in severe acute pancreatitis is best completed utilizing central venous� or Swan-Ganz catheter�assisted monitoring. As talked about, mortality is substantially increased with growing organ dysfunction, particularly if shock is concerned. Metabolic Disturbances Hyperglycemia and hypocalcemia are frequent in extreme disease. Hyperglycemia is usually transient and is because of insulin deficiency from presumed islet cell necrosis or hyperglucagonemia. Controversies in medical pancreatology: Management of acute idiopathic recurrent pancreatitis. Initial management of acute pancreatitis: Critical points in the course of the first 72 hours. Comparison of problems attributable to enteral and parenteral diet in predicted severe acute pancreatitis: A systematic evaluate and metaanalysis. Primary conservative treatment ends in mortality corresponding to surgical procedure in patients with contaminated pancreatic necrosis. Coagulation Disorders Mild coagulation defects, as measured by elevated d-dimer ranges in the blood, are common in acute pancreatitis. Fat Necrosis Fat necrosis happens in subcutaneous tissue, bone, retroperitoneal tissue, peritoneum, mediastinum, pleura, and pericardium. The incidence and case-fatality charges of acute biliary, alcoholic, and idiopathic pancreatitis in California, 1994-2001.
Discount clomid 50mg without a prescriptionDiagnosis is usually recommended by an abdominal radiograph exhibiting displacement and extrinsic compression of gastric lumen. Gastric duplication in a 12-year-old boy with a 1-year history of vomiting and intermittent belly pain. D, An intraoperative picture of the gastric duplication after dissection of the stomach and earlier than resection. Additionally, mucosectomy or mucosal floor ablation should be thought of as a end result of the development of malignancy in enteric duplications has been documented in adults. These tumors might have their origins in pluripotential cells and comprise all 3 embryonic germ cell layers. Most are located alongside the larger curvature of the abdomen and are extragastric, although intramural extension has been reported. The new child infant with a teratoma could additionally be delivered prematurely or have respiratory distress on the basis of increased belly stress. Delivery could additionally be tough, placing the toddler in danger for accidents such as shoulder dystocia. Gastric teratoma associated with gastric perforation, mimicking meconium peritonitis, has been described. Premalignant adjustments and frank malignant transformation to adenocarcinoma have been reported,28,29 and peritoneal gliomatosis has been noticed. Fortunately, even those cases with malignant histologic features or extension into adjoining tissues have an excellent prognosis. A localized lack of nitric oxide synthase, an enzyme related to clean muscle leisure, or irregular neuronal innervation associated with decreased muscle neurofilaments, nerve terminals, synaptic vesicle protein, and neural cell adhesion molecule32 has been implicated. Incidence is highest amongst whites (especially northern Europeans), whereas incidence is decrease amongst African Americans and Africans and lowest among Asians. Others at elevated threat are first-born male infants, especially these with high birth weights or born to professional dad and mom. Initially infants present with gentle spitting, which progresses to projectile vomiting following feedings. Vomiting could also be so forceful as to exit by way of the nostrils, in addition to the mouth. Early in the course the toddler stays hungry following vomiting episodes however, with time, loses interest in feeding and will present wasted and severely quantity depleted. Decreased urinary and stool output accompanies Gastric Volvulus See Table 48-1 and Chapter 26. The classic physical signs are a palpable pyloric mass and visual peristaltic waves. The palpable "olive" is most simply felt in a wasted affected person, immediately following emesis or aspiration of the stomach. The location of the olive varies from the level of the umbilicus to close to the epigastrium. The pyloric mass is palpable in 70% to 90% of affected infants, depending on the expertise and persistence of the examiner. Emptying the abdomen by nasogastric tube placement and palpation of the abdomen with the infant within the susceptible position could improve detection. Many infants seem jaundiced because of an indirect hyperbilirubinemia related to volume depletion and perhaps malnutrition. When the presentation is typical and the olive palpated, no studies are needed. However, in the minority of infants with projectile vomiting, definitive prognosis requires radiologic studies. Non-contrast radiography demonstrates a distended stomach with paucity of fuel beyond the abdomen. The numeric value for the lower limit of pyloric muscle thickness has diversified in stories within the literature, ranging between three and four. Many contemplate the numeric worth less necessary than the general morphology of the canal and real-time observations. Contrast radiography have to be carried out fastidiously, and gastric contents should first be aspirated. Characteristic findings include an elongated slender pylorus with the appearance of a "double channel. Depending on severity, fluid and electrolyte repletion can usually be completed within 24 hours. Definitive remedy is the Ramstedt pyloromyotomy, which entails a longitudinal incision by way of the hypertrophied pyloric muscle all the method down to the submucosa on the anterior surface of the pylorus. After spreading the muscle, the intact mucosa bulges via the incision to the extent of the incised muscle. With this procedure the pylorus is grasped with a Babcock clamp that disrupts the hypertrophied circular muscular tissues in 2 places. Nonoperative remedy consists of using anticholinergic medications55 and paste-consistency feedings until such time that the muscle hypertrophy resolves. All of these lesions happen with biggest frequency close to the ampulla of Vater, with most lesions (80%) occurring distal to this landmark. The general incidence of the 3 anomalies mixed is about 1 per 200,000 stay births, with a slight predilection for girls. This is distinct from atresia or stenosis of the jejunum and ileum, that are attributable to vascular accidents in utero. Trisomy 21 is strongly related to duodenal atresia/stenosis/web in that wherever from 25% to more than 50% of cases happen in infants and kids with this chromosomal anomaly. Familial affiliation is rare, although isolated case reports recommend a possible genetic affiliation. The resected pylorus demonstrates regular mucosa and marked circumferential thickening of the muscularis propria. In contrast with the infantile type, the bodily examination will not be useful because the pyloric mass is difficult to palpate in adults. On distinction radiography, the elongated slender pylorus is again apparent; gastric emptying is delayed, and the stomach may be dilated. Emesis is often bilious as a outcome of most lesions happen distal to the entry of the bile duct into the duodenum. Nonbilious emesis is seen in 15% to 20% of cases secondary to extra proximal obstruction. Any youngster with trisomy 21 and vomiting (especially bile-stained) requires additional analysis for duodenal stenosis. Duodenal stenosis or a partial membrane could present at any age, relying on the diploma of obstruction.
Purchase 25 mg clomid mastercardEndoscopic look of gastric lymphoma with multiple umbilicated lesions adjoining to the gastroesophageal junction. Patients with Hp an infection should be treated with antibiotics to clear the an infection, regardless of stage (see Chapter 51). Patients with a high proportion of huge cells and disease limited to the mucosa might reply to antibiotics alone, though further study of this concern is necessary. Patients with a excessive proportion of large cells and more advanced-stage illness ought to be handled as in Table 31-3 for diffuse massive B cell lymphoma. Additional features related to a worse prognosis are deep infiltration of the abdomen wall, which is associated with a higher likelihood of regional lymph node involvement,forty six and excessive percentages of large cells on histologic analysis. Table 31-2 summarizes remedy based on stage, based on the Paris staging system. Follow-up endoscopy with multiple biopsies must be carried out 3 to 6 months after completion of therapy to document clearance of an infection and assess disease regression. Patients are then followed with endoscopy roughly every 6 months for two years after which yearly. Overall, some 75% of sufferers with stage I disease confined to the mucosa and submucosa will achieve complete remission. Approximately 90% of sufferers who had a whole medical remission to Hp eradication stay in remission,25 however late relapses can happen. Relapse may occur in association with Hp reinfection and could be cured by eradicating the organism again. However, it is necessary to recognize that the current literature in this subject is less than optimal in several respects: older studies are restricted by inadequate staging procedures and outdated classification techniques, none of the stories in the literature is a managed or randomized trial, and longer follow-up is critical. Management of patients with localized illness however a major share of large cells is also uncertain. More current research have documented remission to Hp eradication, in distinction to earlier studies. For instance, in 1 examine of 34 patients with with high-grade histology, 18 of the sufferers had illness regression with Hp eradication and were freed from lymphoma after a median follow-up of 7. As can be anticipated, these patients are much less more doubtless to reply to antibiotic therapy, however anti-Hp remedy should still be attempted because of the potential for falsenegative outcomes for Hp or in the occasion that H. There is currently no consensus relating to the optimal management of this group of patients. Thus, radiotherapy has turn into the preferred therapy for sufferers with advanced-stage local disease, in addition to those who are adverse for Hp or have persistent lymphoma regardless of Hp remedy. Singleagent oral chemotherapy utilizing cyclophosphamide sixty five or chlorambucil has activity, as does remedy with purine analogs corresponding to fludarabine or cladribine, which may be simpler in patients with the t(11;18) translocation. One examine has suggested that Hp infection is more widespread in sufferers whose large cell lesions had a low-grade component. Finally, statement of a response of early-stage large cell lymphomas to Hp eradication has suggested a job for the organism, no less than in some instances. Tumors with a low-grade component usually have a tendency to be multifocal than tumors with no low-grade element. Microscopic examination reveals compact clusters, confluent aggregates, or sheets of enormous cells that resemble immunoblasts or centroblasts, most often with a combination of the two. However, the growing consensus appears to favor combined chemotherapy and radiation and avoidance of surgery (see text). The suggestion for the addition of rituximab on this setting involves extrapolation of randomized knowledge from nodal diffuse massive B cell lymphoma. Clinical Features Patients present with epigastric pain or dyspepsia, symptoms much like these sufferers with gastric adenocarcinoma. This strategy had the advantage of providing diagnostic and staging data and prevented the chance of perforation or bleeding that was believed to result from remedy with chemotherapy or radiation. Approximately 70% of patients with stage I disease are disease-free 5 years after surgical procedure. In addition, the chance of bleeding or perforation during chemotherapy is lower than 5%, and only a few of those that bleed require urgent gastrectomy. Surgery carries a 5% to 10% threat of mortality and is related to important morbidity. Retrospective research have proven related outcomes in patients treated with surgical procedure alone versus chemotherapy alone. Whether the patient underwent surgery or not was left to the discretion of every participating heart. There was no difference in survival fee between those that obtained surgical procedure followed by chemoradiotherapy and these who acquired chemoradiotherapy alone. Patients could current with abdominal ache, weight loss, obstruction, belly mass, bleeding, and/or perforation. Approximately half of sufferers have localized disease, and half have disease unfold to regional or distant nodes. Surgery may be required because of obstruction or perforation,one hundred fifteen and extra therapy contains anthracycline-containing chemotherapy with rituximab. Thus, marginal zone and follicular lymphomas are considered indolent processes, incurable however controllable by chemotherapy, and sometimes associated with a comparatively lengthy survival. Microscopically, mantle cell lymphoma includes the mucosa and submucosa, and the malignant cells have the looks of small atypical lymphocytes, which can encompass benign-appearing germinal facilities or could efface the lymphoid tissue. The disease is characterized by t(11;14), a translocation that leads to rearrangement and overexpression of the gene encoding cyclin D1. Although mantle cell lymphoma is initially aware of chemotherapy,122 it eventually turns into refractory; median survival is 3 to 5 years. The illness usually presents as a single annular or exophytic tumor,114 which can be current anyplace in the small gut; disease is often confined to the gut or to local nodes. Some sufferers have obtained chemotherapy, but few information are available concerning regimens and end result. It should be noted that in nodal marginal zone lymphoma, chemotherapy is often reserved for sufferers with signs, because the disease is known to be slow-growing and sensitive to chemotherapy, however not curable by it. As in gastric marginal zone B cell lymphoma, the small intestinal selection could have varying components of huge cell transformation. As noted, sufferers with this prognosis may current with the gross look of multiple lymphomatous polyposis. Endoscopic look of mantle cell lymphoma presenting as lymphomatous polyps in the stomach (A) and in the colon (B). Additional synchronous and metachronous lesions have been present or later developed in the ileum and duodenum, in addition to the rectum and sigmoid colon. B, Low-power photomicrograph of the ileum exhibiting a number of discrete websites of mucosal and submucosal involvement by lymphomatous polyposis. The concerned lymphoid tissue microscopically has a starry-sky look brought on by quite a few benign macrophages which have ingested apoptotic tumor cells. Most circumstances have a translocation of c-myc on chromosome eight, either to the immunoglobulin heavy-chain region on chromosome 14 or to 1 of the immunoglobulin lightchain regions on chromosomes 2 or 22, leading to a t(8;14), t(2;8), or t(8;22) translocation. A diagnosis in North America or Europe ought to be questioned except the affected person has previously lived in an endemic space.
Cheap 25 mg clomid amexOnly dilators particularly designed to treat achalasia achieve enough diameter for lasting effectiveness. There is basic settlement that pneumatic dilation could be accomplished on an outpatient basis with the affected person under aware sedation. The strategy of pneumatic dilation is variable among practitioners when it comes to affected person preparation, parameters of balloon inflation, and postdilation monitoring. The main complication of pneumatic dilation is esophageal perforation, though perforation-related mortality may be very rare. Alternatively, some practitioners routinely acquire a fluoroscopic examination of the esophagus following pneumatic dilation to make certain that perforation has not occurred. Amyl nitrite,328 sublingual nitroglycerin,329 theophylline,329 and 2-adrenergic agonists329 have additionally been tried. The largest reported expertise has been with isosorbide dinitrate (Isordil) and nifedipine. Sublingual nifedipine administered earlier than meals (30 to 40 mg/day) was studied in 29 patients with early achalasia (prior to esophageal dilatation). Nifedipine was considerably better than placebo (which had no benefit), with good leads to 70% of achalasics followed for six to 18 months. Although conceptually interesting, the practicality of using sildenafil clinically is limited by its cost and potential unwanted side effects. Side effects are rare however can include chest discomfort for a number of days and occasional rash. Heller Myotomy Current surgical procedures for treating achalasia are variations on the esophagomyotomy described by Heller in 1913, consisting of an anterior and posterior myotomy carried out through either a laparotomy or a thoracotomy. However, adoption of the laparoscopic approach for achalasia surgical procedure has led many practitioners to rethink this. Published series of the efficacy of Heller myotomy in treating achalasia report good to glorious ends in 62% to 100% of sufferers, with persistent dysphagia troubling fewer than 10% of sufferers. In the previous, post-myotomy gastroesophageal reflux in achalasics could be particularly extreme, making this a hotly disputed element of the surgical technique. Thus, laparoscopic Heller myotomy mixed with a partial fundoplication (Toupet or Dor) has turn into the popular surgical procedure for achalasia. An unsatisfactory outcome following Heller myotomy can result from incomplete myotomy, scarring of the myotomy, useful esophageal obstruction from the antireflux component of the operation, paraesophageal hernia, or severe esophageal dilatation. Only 1 multicenter potential randomized controlled trial exists comparing pneumatic dilation to laparoscopic Heller myotomy. There was no distinction in success rates after 2 years of follow-up: 92% for pneumatic dilation versus 87% for laparoscopic myotomy. Hence, one should assess the available native resources, as nicely as patient preference, in selecting the initial remedy. Treatment Failures Persistent dysphagia after achalasia therapy suggests remedy failure and must be evaluated with some combination of endoscopy, esophageal manometry, and fluoroscopic imaging. Endoscopy might detect esophagitis, stricture, paraesophageal hernia, or anatomic deformity. Fluoroscopy is useful each to identify anatomic problems and to consider esophageal emptying using a timed barium swallow, a standardized technique of measuring the height of the esophageal barium column 1 and 5 minutes after ingestion. In the case of a patient not previously operated on, this might doubtlessly be either repeat dilation or Heller myotomy. Reoperation, generally, is much less effective than an initial operation for any indication in achalasia. In extremely advanced or refractory cases of achalasia, esophageal resection with gastric pull-up or interposition of a phase of transverse colon or small bowel could be the solely surgical choice. Although wonderful long-term practical results could be achieved, the reported mortality of this surgery is about 4%, in preserving with the mortality rate of esophagectomy accomplished for different indications. Risk of Squamous Cell Cancer Squamous cell carcinoma might develop in the achalasic esophagus. The tumors develop a few years after the prognosis of achalasia and usually come up in a greatly dilated esophagus. Symptoms attributable to the most cancers could be delayed, and the neoplasms are often large and advanced at the time of detection. However, a chic analysis of a database encompassing the whole Swedish inhabitants of 1062 achalasics means that after discounting incident carcinomas, the general squamous cell most cancers danger for achalasics compared to age-matched controls was 17-fold, leading to a 0. However, even that calculation is optimistic, provided that detection of a small cancer in a massively dilated esophagus with retained food and stasis esophagitis is much from assured. However, additionally they state that if surveillance was thought-about, it would be cheap to start 15 years after the onset of achalasia signs. Consequently, therapy focuses on minimizing potential complications using lifestyle modifications. Additionally, these sufferers are weak to pill esophagitis, and care ought to be taken to keep away from caustic pills and to convert medicines to liquid formulation, sublingual, or smaller variations to reduce tablet esophagitis. The only controlled trial exhibiting efficacy was with the anxiolytic trazodone, suggesting that reassurance and control of anxiety are important therapeutic targets. However, in the one controlled trial of this remedy, dilation with an 8-mm "placebo" dilator was as effective as an 18-mm "therapeutic" dilator in producing transient symptom relief. Esophageal Hypersensitivity Therapies for esophageal motor problems have traditionally centered on bettering esophageal contractility and emptying. However, the efficacy of those therapies may be very restricted besides within the occasion of achalasia. More recently, there was a paradigm shift with the conclusion that minor manometric findings formerly interpreted as indicative of symptomatic hypercontractile conditions have been usually epiphenomena indicative of hypersensitivity syndromes. Pharmacologic Treatments Antidepressants are the most typical medications prescribed for visceral ache modulation or chest ache of esophageal origin. In a randomized placebo-controlled research, imipramine at a dose of fifty mg at nighttime was proven to be efficient in lowering chest pain in sufferers with normal coronary angiograms. Smooth muscle relaxants corresponding to calcium channel blockers and nitrates have been used for these disorders. Although they scale back peristaltic amplitude, neither has been proven to relieve chest pain or dysphagia in scientific trials. Sildenafil is an appealing various owing to its profound 732 Section V Esophagus are 10 to 25 mg at bedtime, with escalations of 10- to 25-mg increments to a goal of 50 to seventy five mg. Unfortunately, several of those drugs have proved to have unacceptable risks related to cardiac arrhythmias or intestine ischemia that led to their withdrawal. Theophylline has also proven promising effects within the remedy of noncardiac chest pain, presumably by adenosine receptor blockade. In a latest placebo-controlled double-blind examine, sensory and biomechanical properties of the esophagus were assessed using impedance planimetry in 16 sufferers with esophageal hypersensitivity. In a parallel research using oral theophylline (or placebo) in 24 chest ache sufferers, there was a big reduction in chest pain episodes, chest ache period, and chest pain severity in the theophylline group. American Gastroenterological Association technical review on the clinical use of esophageal manometry. Distal esophageal spasm in high-resolution esophageal stress topography: Defining clinical phenotypes.
Buy clomid 25 mgThe measurement is typical for primary small intestinal carcinoids, and the tumor is subepithelial in location. B, Histopathology of a small intestinal carcinoid with its attribute insular growth sample. The well-differentiated endocrine tumors (functional or nonfunctional) are further divided into those with benign habits (confined to pancreas, nonaggressive, <2 cm) and those with uncertain habits (confined to pancreas, >2 cm or with vascular invasion). The well-differentiated endocrine carcinomas (functional and nonfunctional) are low-grade malignancies with potential for local invasion and/or metastases. Pathophysiology and Pathology Insulinomas are virtually at all times positioned in (or are attached to) the pancreas. Insulin is synthesized as preproinsulin by beta cells of the pancreatic islets within the rough endoplasmic reticulum. Proinsulin is liberated from preproinsulin and transferred to the Golgi equipment. Within these granules, a protease excises the C-peptide, and the C-peptide and the doublestranded insulin molecule are secreted in equimolar quantities. Proinsulin accommodates the alpha and beta chains of insulin and, as a end result of most insulin antibodies used in radioimmunoassays (discussed later) recognize moieties on these chains, additionally they acknowledge proinsulin. Proinsulin represents less than 25% of whole immunoreactive plasma insulin in normal topics, whereas almost all (>90%) patients with insulinomas have an elevated proportion of proinsulin relative to complete insulin. They often occur in patients between 20 and 75 years of age; 60% of them are girls. Patients regularly learn to avoid signs by consuming frequently, and obesity may end result. However, if a fasting blood glucose willpower is combined with a concomitant fasting plasma insulin level, this insulin level shall be inappropriately elevated in 65% of patients with insulinoma. Hypoglycemia with fasting or train differs temporally from hypoglycemia that occurs after meals (postprandial hypoglycemia), which can be caused by many unrelated circumstances (Table 33-6). Other much less frequent causes of fasting hypoglycemia with hyperinsulinism from islet cell illness, besides insulinoma, embrace insulinomatosis, islet hyperplasia122 and nesidioblastosis. Most symptoms of insulinomas14,21,31,40,112 are caused by neuroglycopenia, as a outcome of glucose is the principle source of energy for the mind. C-peptide, launched from beta cells in equimolar quantities to insulin, can be expected to be proportionately elevated with insulin in insulinomas. Measurement of C-peptide has proved helpful in differentiating pathologic hypersecretion of insulin, similar to in sufferers with insulinoma or insulinomatosis, from patients surreptitiously utilizing insulin, because commercial insulin preparations contain no C-peptide. Thus, in insulinoma, the characteristic findings are elevated or normal insulin and plasma C-peptide ranges, whereas in patients utilizing insulin surreptitiously the plasma insulin degree shall be excessive and the C-peptide stage low. Medical Therapy Hypoglycemia is controlled in most insulinoma patients by a mix of dietary and pharmacologic therapy. More slowly absorbed types of carbohydrates (starches, bread, potatoes, rice) are preferable. During a hypoglycemic episode, however, rapidly absorbable carbohydrates such as fruit juices with glucose or sucrose are preferable. Diazoxide should be initiated at a dose of 3 to eight mg/kg/day, divided into 2 or 3 doses per day; if not efficient, diazoxide may be increased to a maximum every day dose of 15 mg/kg. Adverse effects are dose related and will limit the power to reach maximal doses. Addition of a thiazide diuretic can right the edema as nicely as increase the hyperglycemic effect of diazoxide. Approximately 60% of insulinoma patients reply to diazoxide; some patients have been handled with it for over 20 years. The long-acting somatostatin analog octreotide has controlled hypoglycemia in numerous instances of insulinoma. However, in some wholesome, overweight fasted individuals, the insulin-to-glucose ratio could exceed 0. However, the fasting glucose remains regular (>55 mg/dL) in these obese people. Until lately, most serum insulin ranges radioimmunoassays had some cross-reactivity with proinsulin, but current insulin-specific radioimmunoassays with no cross-reactivity with proinsulin are increasingly used. A variety of conditions in addition to insulinoma may cause fasting hypoglycemia (see Box 33-1). Octreotide controls symptoms and hypoglycemia in 40% to 60% of sufferers with insulinoma. Somatostatin analogs are thought to act primarily by interacting with high-affinity somatostatin receptors on the tumor, especially subtypes 2 and 5. Though generally well tolerated, opposed effects of octreotide occur, including bloating and stomach cramping. Long-term unwanted effects (discussed later under Carcinoid Syndrome) embody malabsorption and cholelithiasis. In addition to enhancing symptoms, octreotide decreases plasma insulin ranges in 65% of sufferers. Furthermore, the low pH inactivates pancreatic lipase and might precipitate bile acids. Presently, 60% to 90% of gastrinomas are found within the "gastrinoma triangle," an area formed by the junction of the cystic and bile ducts posteriorly, the junction of the second and third parts of the duodenum inferiorly, and the junction of the pancreatic neck and body medially. The 10-year survival price in sufferers with aggressive progress was solely 30%, whereas it was 96% in those with tumors without aggressive growth. Predictors of hepatic metastases had been a pancreatic as opposed to a non-pancreatic gastrinoma and a main tumor size bigger than three cm. Because insulinomas are equally distributed within the pancreas, distal pancreatectomy has only a 50% likelihood of success. Because insulinomas are nearly invariably intrapancreatic and usually benign, insulinomas detected on imaging preoperatively are more and more being resected efficiently using a laparoscopic strategy. Signs similar to outstanding gastric folds on endoscopy (see left higher panel) or an imaging examine. Very few patients had normal values; 60% had less than 10-fold serum gastrin increases. Effects of gastrinoma extent on survival and of primary gastrinoma location and measurement on the event of lymph node or liver metastases (mets). Right, Upper half shows the proportion of eighty three patients with primary pancreatic or duodenal gastrinomas who developed lymph node or liver metastases. Lower part reveals proportion of 118 sufferers with major gastrinoma of varying diameter who developed lymph node or liver metastases. Sufficient antisecretory drug needs to be given to reduce acid hypersecretion, measured during the hour previous to the following dose of drug, to less than 10 mEq/hr in sufferers without prior gastric acidreducing surgery or to less than 5 mEq/hr in sufferers with prior gastric acid�reducing surgical procedure.
References - Martinell J, Lidin-Janson G, Jagenburg R, et al: Girls prone to urinary infections followed into adulthood: indices of renal disease, Pediatr Nephrol 10:139-142, 1996.
- DeLancey J, Gosling J, Creed K, et al: Gross anatomy and cell biology of the lower urinary tract. In Abrams P, Cardozo L, Khoury S, et al, editors: Incontinence, Plymouth (UK), 2002, Health Publication, Ltd., pp 17n82. DeLancey J: Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis, Am J Obstet Gynecol 170:1713n1717, 1994.
- Norlen L, Trasti H: Functional behavior of the continent ileum reservoir for urinary diversion: an experimental and clinical study, Scand J Urol Nephrol 49(Suppl):33n35, 1978.
|
|