"Purchase aziphar 250 mg on-line, good antibiotics for sinus infection."By: J. Matthew Brennan, MD - Associate Professor of Medicine
- Member in the Duke Clinical Research Institute
 https://medicine.duke.edu/faculty/j-matthew-brennan-md
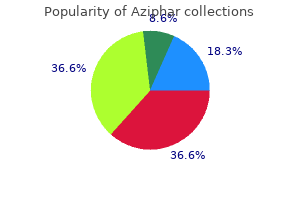
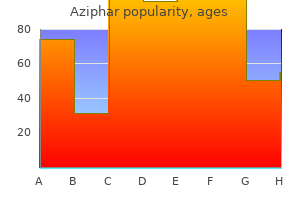
Order aziphar 500 mg with amexSome human studies have discovered an association between exposure to anesthesia and surgery in early childhood and subsequent neurodevelopmental issues. Pediatric anesthesia requires acceptable pediatric gear in a range of sizes. Distraction techniques, premedication with midazolam or 2 agonists, and parental presence at induction have all been shown to scale back anxiety. The most substantial modifications occur at delivery and in early infancy; however, many methods proceed to develop all through childhood. This prenatal interval is characterized by increased vulnerability to a big number of genetic and exterior components that can induce permanent organ dysfunction of variable severity (Table 77. Prenatal development is normally divided into three levels: (1) the germinal, (2) the embryonic, and (3) the fetal stage. The germinal stage starts with conception and ends roughly 2 weeks later with the implantation of the embryo into the uterine wall. Factors, both genetic or environmental, that intervene with the implantation process lead to the termination of being pregnant. The embryonic stage comprises the period between the third and eighth weeks of pregnancy and is characterised by intense cell proliferation, migration, and differentiation leading to the establishment of all major organs. Increased vulnerability to a wide variety of substrates, generally known as teratogens, throughout this period can induce main developmental defects, many of them incompatible with life. The fetal stage lasts from the ninth week of pregnancy to birth and is characterized by the expansion and useful differentiation of organs shaped through the embryonic period. Numerous exogenous components, similar to environmental toxins, ionizing radiation, and maternal infections in addition to a massive number of medication can intrude with the physiological patterns of organ improvement all through the fetal interval which, in flip, will lead to organ dysfunction of variable severity. Careful evaluation of prenatal history is therefore an important a part of preoperative evaluation and may guide further investigations prior to perioperative administration. While being pregnant is taken into account to attain full time period between the completion of the 37th and the forty second weeks of gestation, fetuses attain an age of viability that could be thought of, underneath tight medical support, as suitable with extrauterine life between the twenty second and twenty sixth weeks after conception. Infants weighing less than these norms could be categorised as low birth weight (<2500 g), very low start weight (<1500 g), and extremely low birth weight (<1000 g). The transition from intra- to extrauterine life is rapid and entails a posh and wellorchestrated collection of occasions aimed to guarantee neonatal viability. Apgar scores between 7 and 10 are thought of reassuring, a rating of four to 6 as reasonably irregular, while scores 3 and under are often indicative of poor consequence. In utero, many of the cardiac output is directed from the placenta throughout the foramen ovale into the ascending aorta (oxygenated blood), whereas superior vena cava blood (deoxygenated) is directed to both the pulmonary artery and the ductus arteriosus (see also Chapter 78). At delivery, a quantity of events change hemodynamic interactions such that the fetal circulation adapts to the postuterine environment. Specifically, the placenta is faraway from the circulation; portal blood stress falls, which causes the ductus venosus to shut; and blood turns into oxygenated via the lungs. As a result of the combined results of lung growth, exposure of blood to oxygen, and lack of low resistance via placental blood circulate, pulmonary vascular resistance decreases while peripheral vascular resistance rapidly rises. The decrease in pulmonary vascular resistance occurs on the primary day of life and continues to decrease progressively through the subsequent a quantity of years because the structure of the pulmonary vessels changes. An improve in stress on the left aspect of the guts (caused by the rise in peripheral vascular resistance) induces mechanical closure of the foramen ovale. As a result, all three connections between the best and left sides of the circulation close. During this crucial interval, the toddler can readily revert from the adult sort of circulation to a fetal kind of circulation; this state known as transitional circulation. When such a flip-flop occurs, pulmonary artery strain increases to systemic levels, blood is shunted past the lungs via the patent foramen ovale, and the ductus arteriosus might reopen and allow blood to shunt at the ductal degree. In this situation, the hypoxemia may be extended, despite adequate pulmonary air flow with one hundred pc oxygen. Risk components growing the probability of extended transitional circulation embody prematurity, infection, acidosis, pulmonary disease leading to hypercapnia or hypoxemia (aspiration of meconium), hypothermia, and congenital coronary heart illness. Care have to be directed to preserving the toddler heat, maintaining normal arterial oxygen and carbon dioxide tensions, and minimizing the results of anestheticinduced myocardial depression for these newborns requiring anesthesia. The myocardial construction of the heart, notably the volume of mobile mass devoted to contractility, is significantly less developed in neonates than in adults. This difference, as properly as developmental changes in contractile proteins, produce a leftward displacement of the cardiac function curve and fewer compliant ventricles. The most regularly encountered arrhythmia in pediatric populations is hypoxia-induced bradycardia that may lead to asystole, if not appropriately dealt with. Generally, myocardial perform is often adequate in most infants and kids including these with congenital heart illness. Rare exceptions from this rule are individuals with congenital neuromuscular and metabolic illnesses where the myocardium could be seriously compromised. The lung bud septates from the foregut in the course of the first trimester and the fuel exchanging parts of the airway are formed through the second trimester. Alveolar ductal growth starts at gestation week 24 while the septation of the air sacs begins around gestational week 36. At term, full growth of surface-active proteins helps maintain patency of the airways. If a toddler is prematurely born and these proteins are insufficient, then respiratory failure. The airway of infants is extremely compliant and poorly supported by the encompassing buildings. Dead house air flow is proportionally much like that in adults; nonetheless, oxygen consumption is 2 to three times greater. In preterm infants, the work of breathing is approximately 3 times that of adults. Another essential factor is the composition of the diaphragmatic and intercostal muscle tissue. Differences in airway anatomy clarify the more probably potential for technical airway difficulties in infants than in teenagers or adults. The larynx is situated higher (more cephalic) within the neck, thus making straight blades extra helpful than curved blades. For grownup sufferers, the airway size is much bigger, so the commonly used tracheal tubes are normally simple to advance past the glottic opening. As a result of the delayed improvement, newborns have decreased ability to excrete free water and solute loads; the half-life of medicines excreted via glomerular filtration will be prolonged. The number of sort I muscle fibers is inversely associated to age and will account, in part, for the ease of inducing respiratory fatigue because the work of breathing will increase. This anatomic difference is considered one of the causes uncuffed tracheal tubes have been traditionally most popular for youngsters youthful than 6 years of age. The cytochrome P450 system is responsible for part I drug metabolism of lipophilic compounds. The capability of neonates to metabolize some medicine relies on particular particular person drug cytochromes. These reactions are sometimes impaired in neonates and end in jaundice (decreased bilirubin breakdown) and long drug (and their energetic metabolites) half-lives. In addition, the binding of some medicine to albumin may be altered within the presence of hyperbilirubinemia in the neonatal period; this impact is extra necessary for medication with high protein binding as a result of a greater fraction of unbound drug will happen.
Purchase aziphar american expressThe Cataract National Dataset digital multicentre audit of fifty five, 567 operations: antiplatelet and anticoagulant medicines. Hemorrhagic complications from glaucoma surgical procedure in patients on anticoagulation remedy or antiplatelet remedy. Risk of intraocular bleeding with novel oral anticoagulants compared with warfarin a systematic evaluation and meta-analysis. Risk of considerable intraocular bleeding with novel oral anticoagulants systematic evaluation and meta-analysis. Ophthalmic regional blockade complication fee: a single heart audit of 33,363 ophthalmic operations. Impact of anesthesia on hospital mortality and morbidities in geriatric patients following emergency hip fracture surgery. Comparison of general anesthesia and monitored anesthesia care in patients undergoing breast most cancers surgery utilizing a mixture of ultrasound-guided thoracic paravertebral block and local infiltration anesthesia: a retrospective research. Comparison of clinical outcomes, affected person, and surgeon satisfaction following topical versus peribulbar anesthesia for phacoemulsification and intraocular lens implantation: a randomized, managed trial. Monitored anesthesia care with dexmedetomidine: a potential, randomized, double-blind, multicenter trial. Sole use of dexmedetomidine has limited utility for aware sedation throughout outpatient colonoscopy. Propofol versus propofol-ketamine sedation for retrobulbar nerve block: comparison of sedation high quality, intraocular strain modifications, and restoration profiles. Remifentanil versus remifentanil/midazolam for ambulatory surgery during monitored anesthesia care. The comparative amnestic results of midazolam, propofol, thiopental, and fentanyl at equisedative concentrations. Concurrent ketamine and alfentanil administration: pharmacokinetic concerns. Comparative analgesic and mental results of increasing plasma concentrations of dexmedetomidine and alfentanil in people. A novel mixture of propofol, alfentanil, and lidocaine for regional block with monitored anesthesia care in ophthalmic surgery. Population pharmacokinetics of dexmedetomidine throughout long-term sedation in intensive care patients. Obesity as a risk issue sedation-related problems throughout propofol-mediated sedation for superior endoscopic procedures. Evolution of modifications in upper airway collapsibility throughout gradual induction of anesthesia with propofol. The laryngeal mask airway for intraocular surgical procedure: effects on intraocular pressure and stress responses. Effects of propofol, etomidate, and thiopental on intraocular strain and hemodynamic responses in phacoemulsification by insertion of laryngeal mask airway. Prospective comparison of use of the laryngeal masks and endotracheal tube for ambulatory surgical procedure. Thresholds and acute kidney and myocardial injury after noncardiac surgical procedure a retrospective cohort analysis. Perioperative stroke and related mortality after noncardiac, nonneurologic surgery. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Tracheal extubation of deeply anesthetized pediatric patients: a comparability of isoflurane and sevoflurane. Tracheal extubation of deeply anesthetized pediatric patients: a comparability of desflurane and sevoflurane. Effect of propofol and sevoflurane on coughing in smokers and non-smokers awakening from general anaesthesia at the end of a cervical spine surgery. Prevention of endotracheal tube-induced coughing during emergence from common anesthesia. The effects of lidocaine spray and intracuff alkalinized lidocaine on the occurrence of cough at extubation: a double-blind randomized controlled trial. The development and validation of a threat score to predict the likelihood of postoperative vomiting in pediatric sufferers. Subhypnotic propofol infusion plus dexamethasone is simpler than dexamethasone alone for the prevention of vomiting in youngsters after tonsillectomy. Preterm infants are more susceptible to complications following minor surgical procedure than are term infants. Ophthalmic pain following cataract surgical procedure: a comparison between local and common anaesthesia. Factors independently related to increased risk of ache improvement after ophthalmic surgery. Factors associated with postoperative pain and analgesic consumption in ophthalmic surgery: a systematic evaluate. Chronic opioid use after surgical procedure: implications for perioperative administration within the face of the opioid epidemic. Deaths from unintentional harm amongst adults aged 65 and over: United States, 2000�2013. Local anesthesia with intravenous sedation for surgical restore of selected open globe injuries. The results of steep Trendelenburg positioning on intraocular strain throughout robotic radical prostatectomy. The impact of steep Trendelenburg positioning on intraocular stress and visible function throughout robotic-assisted radical prostatectomy. Effect of dexmedetomidine premedication on the intraocular pressure changes after succinylcholine and intubation. Effects of systemic administration of dexmedetomidine on intraocular stress and ocular perfusion strain throughout laparoscopic surgery in a steep Trendelenburg place: potential, randomized, double-blinded study. Endotracheal intubation in an awake affected person with a versatile bronchoscope is usually used when intubation following the induction of basic anesthesia would be imprudent. When the airway dysfunction is so in depth that awake endotracheal intubation is impractical, tracheostomy carried out using native anesthesia (with or with out even handed intravenous sedation) is often the most fitted choice. In extreme loss-of-airway emergencies, a cricothyrotomy may be preferable to a tracheostomy as a outcome of cricothyrotomy takes much less time to complete. In some head and neck instances, corresponding to in sufferers undergoing parotid surgery, the necessity for electrical testing of the facial nerve precludes the extended use of neuromuscular blocking medicine. In many patients with head and neck problems, mild emergence from anesthesia, free of coughing and straining, is vitally essential to stop emergence rebleeding because of venous engorgement. Bleeding following tonsillectomy usually occurs within the first 6 postoperative hours, but it could additionally occur several days later. Facial trauma can produce unremitting bleeding and the aspiration of enamel, blood, bone, and tissue fragments, in addition to cervical backbone injury.
Purchase aziphar 250 mg on-lineSingle-dose epidural administration of lipophilic and hydrophilic opioids is used to provide postoperative analgesia, with considerations typically similar to these mentioned for single-dose intrathecal administration of opioids. A single bolus of epidural fentanyl could also be administered to present rapid postoperative analgesia; however, diluting the epidural dose of fentanyl (typically 50-100 g) in no less than 10 mL of preservative-free normal saline will lower the onset and prolong the length of analgesia, presumably on account of an increase in initial spread and diffusion of the lipophilic opioid. Smaller doses of epidural morphine could additionally be required for elderly sufferers and thoracic catheter sites. Commonly used dosages for intrathecal and epidural administration of neuraxial opioids are supplied in Table 81. Lower doses may be effective when administered to the elderly or when injected in the cervical or thoracic area. Each of those options could affect the quality of postoperative analgesia, patient-reported outcomes, and even charges of morbidity and mortality. Use of a continuous infusion rather than intermittent boluses of epidural morphine may end in superior analgesia with fewer side effects. Use of a local anesthetic and an opioid in an epidural infusion could have benefits over infusions consisting of an area anesthetic or opioid alone. When compared with an area anesthetic or opioid alone, a local anesthetic-opioid mixture offers superior postoperative analgesia (including improved dynamic pain relief), limits regression of sensory blockade, and possibly decreases the dose of local anesthetic administered, though the effect on the incidence is unsure. In basic, bupivacaine or ropivacaine is chosen due to the differential and preferential scientific sensory blockade with minimal impairment of motor perform. Concentrations used for postoperative epidural analgesia are decrease than these used for intraoperative anesthesia. The selection of opioid also varies, although many clinicians favor a lipophilic opioid. A number of adjuvants may be added to epidural infusions to enhance analgesia whereas minimizing unwanted side effects, but none has gained widespread acceptance. Clonidine mediates its analgesic results primarily through the spinal dorsal horn 2-receptors on main afferents and interneurons, in addition to the descending noradrenergic pathway, and the epidural dose usually used ranges from 5 to 20 g/h. Clinical software of clonidine is proscribed by its unwanted effects: hypotension, bradycardia, and sedation. Location of Catheter Insertion Insertion of the epidural catheter congruent to the incisional dermatome. There is a more frequent incidence of lower extremity motor block with the usage of lumbar epidural catheters, and an earlier-than-anticipated termination of epidural analgesia may end result. Furthermore, the advantages of epidural analgesia in lowering morbidity in sufferers present process belly and thoracic surgical procedure are seen solely with thoracic (congruent), not lumbar (incongruent) epidural catheter placement. Nausea and vomiting associated with neuraxial administration of single-dose opioid occurs in up to 50% of sufferers, and the cumulative incidence in those receiving continuous infusions of opioid could also be as excessive as 80%. The general knowledge (neuraxial opioids and/or local anesthetic combined) recommend that the incidence of postoperative vomiting is similar between epidural analgesia and systemic opioids, though female sufferers will exhibit a extra frequent incidence no matter analgesic modality. Use of fentanyl alone or in combination with a neighborhood anesthetic in an epidural infusion is associated with a less frequent incidence of nausea and vomiting than infusions of morphine are. A number of medication have been used efficiently to deal with neuraxial opioid-induced nausea and vomiting, together with naloxone, droperidol, metoclopramide, dexamethasone, ondansetron, and transdermal scopolamine. Pruritus is among the most common side effects of epidural or intrathecal administration of opioids, with an incidence of approximately 60% versus about 15% to 18% for epidural local anesthetic administration or systemic opioids. It is unclear whether the incidence of neuraxial opioid-related pruritus is dose dependent. Many medication have been evaluated for the prevention and remedy of opioidinduced pruritus, which can be tough to manage and fairly bothersome for some sufferers. Serotonin receptor antagonists can also be an efficient modality within the prevention of neuraxial opioid-induced pruritus. The use of epidural morphine is related to postpartum reactivation of herpes simplex labialis. The incidence of respiratory melancholy with neuraxial administration of opioids is dose dependent and usually ranges from zero. The incidence of respiratory melancholy, as outlined by a gradual Side Effects of Neuraxial Analgesic Drugs Many medication-related (opioid and local anesthetic) unwanted effects can occur with using postoperative epidural analgesia, but earlier than routinely ascribing the trigger to the epidural analgesic routine, other causes must be thought of, corresponding to small intravascular quantity, bleeding, and low cardiac output resulting in hypotension and cerebrovascular accident, pulmonary edema, and evolving sepsis resulting in respiratory melancholy. Standing orders and nursing protocols for analgesic regimens, neurologic monitoring, treatment of unwanted side effects, and physician notification about important variables should be standard for all sufferers receiving neuraxial and other kinds of postoperative analgesia (see Box eighty one. The native anesthetics utilized in an epidural analgesic regimen could block sympathetic fibers and contribute to postoperative hypotension. Use of local anesthetics for postoperative epidural analgesia may also contribute to decrease extremity motor block in roughly 2% to 3% of sufferers, and this will lead to the development of strain sores in the heels. Patient-controlled epidural analgesic regimens generally used on the Johns Hopkins Hospital. Delayed respiratory depression is primarily associated with the cephalad unfold of hydrophilic opioids, which generally happens inside 12 hours after injection of morphine. Risk components for respiratory despair with neuraxial opioids embody increasing dose, increasing age, concomitant use of systemic opioids or sedatives, chance of prolonged or in depth surgery, and the presence of comorbid situations. The incidence of urinary retention is extra frequent with neuraxially administered opioids than when given systemically. The finding that solely thoracic epidural analgesia decreases the incidence of postoperative myocardial infarction corroborates experimental information on the physiologic advantages of thoracic epidural analgesia, similar to a reduction within the severity of myocardial ischemia or dimension of infarction, attenuation of sympathetically mediated coronary vasoconstriction, and enchancment of coronary move to areas in danger for ischemia. The use of thoracic epidural analgesia in patients present process cardiac surgical procedure decreased the danger of postoperative supraventricular arrhythmias and respiratory complications. While using intraoperative regional anesthesia decreases the incidence of hypercoagulable-related occasions. The benefits of postoperative epidural analgesia are optimized when the epidural catheter is inserted in a location comparable to the dermatomes covered by the surgical incision. Maximal attenuation of perioperative pathophysiology occurs with the use of an area anesthetic-based epidural analgesic answer. It is unclear whether or not perioperative epidural analgesia might enhance patient-reported outcomes. A regional anesthetic-induced sympathectomy should increase blood move to the extremities with subsequent improvement in tissue oxygenation and a possible favorable native anesthetic 81 � Acute Postoperative Pain 2629 effect on tumor-cell killing. However, there are a quantity of elements that will potentially have an result on cancer recurrence and the impact of perioperative regional analgesic techniques on a long-term consequence such as cancer recurrence is unsure presently. Use of neuraxial anesthesia/analgesia for complete hip or knee alternative might lower the risk of surgical website infections compared with general anesthesia. Some issues are associated with placement of an epidural catheter, and a quantity of other risks related to the utilization of indwelling epidural catheters. A evaluate of neurologic issues after regional anesthesia revealed that the rate of neurologic problems after central neuraxial blockade is less than 4 in 10,000 (0. The concurrent use of anticoagulants and neuraxial anesthesia and analgesia has at all times been a relatively controversial concern however has been highlighted over the previous decade by the increased incidence of spinal hematoma after the introduction of low-molecular-weight heparin in North America in 1993. Different types and classes of anticoagulants have different pharmacokinetic properties that have an effect on the timing of neuraxial catheter or needle insertion and catheter removing. Despite many observational and retrospective studies investigating the incidence of spinal hematoma within the setting of various anticoagulants and neuraxial techniques, no definitive conclusion relating to absolutely the safety of neuraxial anesthesia and anticoagulation has been reached. Concurrent use of a quantity of anticoagulants may enhance the risk of bleeding, and the analgesic routine must be tailored to facilitate neurologic monitoring, which can be continued in some instances for 24 hours after elimination of the epidural catheter.
250 mg aziphar otcLess devastating nerve 2 head accidents caused by cervical traction are phrenic nerve paralysis and Erb or Klumpke palsy, which are caused by brachial plexus stretching or tearing (or both). Shoulder dystocia is commonly related to clavicular and humoral fractures; femoral shaft fractures happen with breech deliveries. Injuries to the liver, spleen, adrenal glands, and kidneys could cause life-threatening hemorrhage or thrombosis. Vasoocclusion causes tissue loss within the cerebral, coronary, or renal vascular beds. Emergency instrumentation of the airway within the supply room on uncommon event leads to tracheal and esophageal perforation, significantly in a untimely toddler. Trauma in Children Accidents and trauma are the leading causes of demise in youngsters 1 to 14 years of age. Blunt trauma to the stomach may cause stable organ harm (liver and spleen), quite than a perforated viscus. Management of trauma patients of all ages requires an organized strategy that allows rapid prognosis and therapy. Most preventable deaths in pediatric trauma sufferers are caused by airway obstruction, pneumothorax, and shock; shock is usually the result of inadequate remedy of bleeding or secondary brain injury from an increasing intracranial hematoma. A disproportionately giant tongue, in relation to a slim oropharynx, simply obstructs the airway in an unconscious child. Proper jaw positioning allows bag-and-mask air flow till the trachea is intubated. Ventilation by way of an insufficient airway might result in gaseous distention of the abdomen, vomiting, and aspiration of gastric contents. After establishing an airway, adequacy of respiration ought to be verified by observation of symmetric chest motion, auscultation of normal and equal breath sounds, and an early chest radiograph. Tension hemopneumothorax can be diagnosed clinically and treated by needle aspiration. Circulation could be shortly assessed by looking for tachycardia, poor peripheral perfusion, weak peripheral pulses, and hypotension (which may not happen until blood loss exceeds 25% of the circulating blood volume). During the secondary survey, a thorough head-to-toe examination is performed, and a plan of definitive therapy is developed. Diagnostic measures in a pediatric trauma patient are similar to these in grownup patients, but there must be consideration of particular issues that happen in youngsters. Most intraabdominal accidents requiring laparotomy are recognized clinically as a result of they produce peritonitis or trigger rising abdominal girth. Indications for surgical intervention for abdominal trauma embody free peritoneal air, evidence of a ruptured viscus, and acute uncontrolled bleeding. The most important indicator of intracranial trauma is a decrease within the level of consciousness. Child Abuse the diagnosis of child abuse is made by finding an acute damage that will have a believable explanation and signs of past trauma, together with healing bruises, contusions, and fractures. Multiple hospital admissions, emergency division visits, physician or hospital "buying," and a historical past of previous trauma should be of concern. Most abused youngsters are older than three years and may have poor hygiene and delayed somatic or psychological improvement. The injuries mostly include bruises, welts, lacerations, scalds, and burns from cigarettes, stoves, heating grates, or irons. Long-bone fractures, usually of various age, belly accidents, indicators of smothering, and multiple gentle tissue or genital bruises are additionally common. Shaking an infant may cause neck injuries, intracranial hemorrhage, and contra-coup accidents, with out essentially producing external manifestations of trauma. The strategy to a suspected sufferer of child abuse features a meticulous and nonjudgmental history, written intimately within the chart. The physical examination includes progress parameters, descriptions of soppy tissue bruising or burns, and diagrams or ideally photographs of all accidents. The color, shape, placement, and estimated age of all accidents must be catalogued. Ingestion Injury Despite the success of assorted preventive public health packages, poisoning continues to occur commonly in pediatric sufferers. Fortunately, the vast majority of presumed poisonings in younger children could be managed by phone session with a regional poison control heart. Although many alternative poisonous substances are ingested by youngsters and adolescents, administration of poisoning has three major objectives: (1) identifying, decontaminating, and eliminating the toxic agents654; (2) minimizing the poisonous results on the child; and (3) offering close statement and organ system help till cleansing is complete. Procedures for drug elimination embody emesis, gastric lavage, activated charcoal, and magnesium citrate. Examples of particular antidotes are deferoxamine for iron ingestion, ethanol infusion for methanol ingestion, naloxone for narcotic overdose, and N-acetylcysteine for acetaminophen ingestion. Because many ingestions, notably those for tried suicide, embody a number of medicine, particular antidote remedy is only occasionally successful. Consultation with medical pharmacologists or with the regional poison management heart and contacting a social employee or psychiatrist are important aspects of the care of an acutely toxic baby. Common complications of ingestions and their remedy embrace aspiration pneumonia with hydrocarbon ingestion or lack of glottic perform, sepsis, respiratory depression, myocardial melancholy, arrhythmias, seizures, and coma. The psychosocial setting that allowed or precipitated the ingestion should even be thought-about. Families ought to be endorsed about correct supervision and "childproofing" their residence. Psychiatric intervention should be introduced early; unsuccessful suicide attempts are sometimes repeated. Transport of the Critically Ill Child Transport for critically ill children consists of intrahospital and interhospital transport. However, this additionally contains transport for radiologic procedures and studies all through the hospital. In this circumstance, the clinician who ordered the take a look at should understand the stability of danger and profit. There are important variations in the ability to monitor and provide care to these patients. Any affected person requiring inotropic assist is in danger for those drugs being interrupted. Depending on the hospital, the group transporting the patient may embrace a respiratory therapist, bedside nurse, and transport nurse. In the smallest patients, the upkeep of physique temperature could be tough during transport. Details to perceive include availability of helicopter and stuck wing flight, kinds of practitioners on the transport team, coverage in the circumstance where the primary staff is out on a transport, and the flexibility to provide interventions when the transport group arrives at the outdoors facility. Many transport care physicians will be succesful of intubate, place arterial and venous strains, and place chest tubes at an out of doors facility. In that regard, the person receiving the transport request could have to make some assessments of whether the affected person is secure to transfer by a team that only supplies primary life help resuscitation. For hospitals unfamiliar with caring for critically ill kids, it might be foremost in their mind to get the child to the next level of care and out of their hospital.
Buy 100 mg aziphar amexTwo approaches can be used to carry out this block: the intraoral and extraoral approaches. Intraoral strategy: For the intraoral strategy, the external landmarks embrace the foramen localized by palpation, the incisor, and the primary premolar. After adverse aspiration, 1 to three mL of local anesthetic is injected for these different approaches. Complications are hematoma, persistent paresthesia of the innervated territory, extended numbness, and intravascular injection. Ultrasound steerage can be used to find the foramina for superficial trigeminal nerve blocks. A finger is positioned over the infraorbital foramen to assess the proper location of the needle tip and keep away from damage to the attention. The main surgical indication in youngsters is cleft lip repair with good perioperative pain management and a decrease in opioid use. The mental foramen is positioned consistent with the pupil on the mental means of the mandible, in regard to the inferior premolar tooth. The 25- or Suprazygomatic Approach to Maxillary Nerve the maxillary nerve exits the cranium through the foramen rotundum and offers its terminal branches. Except for the middle meningeal nerve, innervating the dura mater, all branches (zygomatic branches, superior alveolar nerve, pterygopalatine and parasympathetic branches, palatine and pharyngeal branches) arise in the pterygopalatine fossa to the face. At the upper a part of the pterygopalatine fossa, the maxillary nerve is accessible for a whole maxillary block. The block covers the decrease eyelid, ala of the nose, cheek, higher lip, cutaneous zygomatic and temporal zone on the face and superior teeth, palatine zone, and maxillary bone. The suprazygomatic strategy to the maxillary nerve in pterygopalatine fossa seems to be the most secure and is easily reproducible in children. The needle (22-25 gauge) is inserted perpendicular to the pores and skin and advanced to reach the higher wing of the sphenoid at a depth of approximately 10 to 15 mm. The anterior trunk is formed with branches serving primarily motor innervation to temporalis, masseter, pterygoids, mylohyoid, tensor tympani and palati muscular tissues, and the buccal nerve. Auriculotemporal, lingual, and inferior alveolar nerves comprise the posterior trunk. The needle entry point is situated within the sigmoid fossa between the coronoid and condylar process of the ramus of the mandible. The needle was inserted perpendicular to the skin (A) and advanced to reach the greater wing of the sphenoid at roughly 10 to 15 mm depth (B). Reorientation of needle in a caudal and posterior course (C) and development of 35 to forty five mm deep to the pterygopalatine fossa (D and E). After perpendicular pores and skin penetration, towards the lateral pterygoid plate (to a distance of 2-4 cm of depth), the needle (22-25 gauge) is advanced posteriorly and inferiorly maintaining the same depth, guided by mandible ascension twitch. This transcutaneous procedure with nerve stimulation appears simpler and has a high success fee. Block of the Nose: Nasociliary Nerve Block and External Nasal Nerve Block the innervation of the nose and nasal cavity is kind of complex, implicating each the ophthalmic (V1) and maxillary (V2) branches of the trigeminal nerve. The nasociliary nerve is blocked before its division into nasal branches of the anterior ethmoidal nerve and the infratrochlear nerve, and close to the ethmoidal foramen. The great auricular nerve arises from the second and third cervical nerve roots, emerges from the posterior border of sternocleidomastoid muscle, and ascends (dividing into anterior and posterior branches) to the mandibular, parotid gland, and pinna. It provides the lower again of the auricle, the lobule, and the pores and skin of the angle of the mandible (in complement to the mandibular nerve). The lesser occipital nerve arises from the ventral main rami of the second and third cervical roots and provides the innervation of the higher a part of the ear lobe and lateral occipital zone. The auricular department of the vagus nerve (nerve of Arnold) innervates the concha, many of the posterior wall of the external auditory meatus (zona of Ramsay Hunt), and inferior portion of the tympanic membrane. The auriculotemporal nerve could be blocked by injecting local anesthetic solution above the posterior portion of the zygoma, anterior to the ear and behind the superficial temporal artery. The great auricular nerve and the lesser occipital nerves can be blocked distally over the mastoid course of posterior to the ear. The needle is inserted behind the lower lobe of the ear and advanced following the curve of the posterior sulcus. The superficial cervical plexus block is a extensively described proximal strategy that anesthetizes two of its terminal branches, the lesser occipital nerve and the great auricular nerve. Several painful procedures of the ear can benefit from this analgesic block, corresponding to incision and drainage of an abscess or hematoma,298 suture of a giant laceration of the ear or the pores and skin surrounding the ear,299 postauricular incision as in tympanomastoid surgery and cochlear implants,300 otoplasty,301 and surgical correction of "bat" ears. It is then directed medially and backward involved with the bony roof of the orbit. The exterior nasal department of the anterior ethmoidal nerve may be blocked by infiltration at the junction of nasal bone with cartilage. Combined with infraorbital nerve block, the external nasal nerve block is very efficient for perioperative ache control in cleft lip restore. The auriculotemporal department of the mandibular division of the trigeminal nerve supplies the superior two thirds of the anterior floor. The auriculotemporal nerve passes by way of the parotid gland to ascend anterior to the auditory canal with the superficial temporal artery and passing superiorly superficial to the zygomatic arch. The posterior surface of the ear and the decrease third of its anterior surface depend upon the nice auricular nerve Nerve Block of the Head Greater Occipital Nerve Block. The greater occipital nerve arises from the second cervical nerve root that emerges between the atlas and the axis. It ascends between the obliquus capitis inferior and semispinalis capitis before piercing the latter muscle. At this point, the larger occipital nerve is most frequently located instantly medial to the occipital artery. The higher occipital nerve supplies cutaneous innervation to a major portion of the posterior scalp from the extent of the external occipital protuberance to the vertex. The landmarks to carry out the larger occipital nerve block are positioned at roughly two thirds of the gap on a line drawn from the center of the mastoid to the exterior occipital protuberance alongside the superior nuchal line, where it lies medial to the occipital artery. Palpation in this area might elicit a paresthesia or uncomfortable feeling within the distribution of the nerve. Usually a 25- or 27-gauge needle can be utilized depending on the size of the affected person. The needle is directed at a 90-degree angle towards the occiput and, after aspiration, 1 to three mL of native anesthetic is injected. When the needle is withdrawn, stress must be maintained over the location of injection to promote the nerve impregnation and to obtain hemostasis. Numbness over the top of the pinnacle, after the injection, is a sign of a successful greater occipital nerve block. An ultrasound-guided strategy of larger occipital nerve block has been described lately with good visualization of the nerve. The nerve could be simply visualized between the obliquus capitis inferior and the semispinalis capitis muscle; the pulsation of the occipital artery can be seen near the nerve on this position. The scalp block is classically described with potential blockade of seven nerves, together with branches from cervical spinal rami and from trigeminal division. The higher occipital, lesser occipital, and great auricular nerves originate from ventral and dorsal rami of C2 and C3 spinal nerves.
Buy aziphar from indiaRed blood cell transfusion threshold in postsurgical pediatric intensive care patients: a randomized scientific trial. Disseminated intravascular coagulation rating is associated with mortality for youngsters with shock. Towards definition, medical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Current controversies within the management of idiopathic thrombocytopenic purpura throughout childhood. Continuous renal alternative therapy in children post-hematopoietic stem cell transplantation: the current and the future. Impact of continuous renal alternative remedy on oxygenation in youngsters with acute lung damage after allogeneic hematopoietic stem cell transplantation. Outcomes of hematopoietic stem cell transplant sufferers who acquired continuous renal alternative therapy in a pediatric oncology intensive care unit. The morbidity and mortality of pediatric oncology sufferers presenting to the intensive care unit with septic shock. Improved outcomes of children with malignancy admitted to a pediatric intensive care unit. Intensive care unit mortality trends in youngsters after hematopoietic stem cell transplantation: a meta-regression analysis. Changes in outcomes (1996-2004) for pediatric oncology and hematopoietic stem cell transplant sufferers requiring invasive mechanical ventilation. Evaluation of six danger factors for the development of bacteremia in kids with cancer and febrile neutropenia. The diagnostic value of C-reactive protein, interleukin-8, and monocyte chemotactic protein in threat stratification of febrile neutropenic kids with hematologic malignancies. Frequency of early dying in kids with acute leukemia presenting with hyperleukocytosis. Ventilator-associated pneumonia in pediatric intensive care unit patients: danger factors and outcomes. Tailoring the Institute for Health Care Improvement a hundred,000 Lives Campaign to pediatric settings: the instance of ventilator-associated pneumonia. Ventilator-associated pneumonia within the pediatric intensive care unit: characterizing the problem and implementing a sustainable answer. Effectiveness of a multidimensional method to reduce ventilator-associated pneumonia in pediatric intensive care items of 5 growing international locations: international Nosocomial Infection Control Consortium findings. Impact of bloodstream an infection on the end result of youngsters undergoing cardiac surgery. Pediatric trauma: differences in pathophysiology, harm patterns and remedy compared with adult trauma. Selection and nonoperative administration of pediatric blunt trauma sufferers: the role of quantitative crystalloid resuscitation and stomach ultrasonography. The most frequent explanation for airway obstruction within the quick postoperative period is the lack of pharyngeal muscle tone in a sedated or obtunded patient. The capability to strongly oppose the incisor teeth against a tongue depressor is a reliable indicator of pharyngeal muscle tone. Respiratory failure within the quick postoperative interval is commonly because of transient and rapidly reversible conditions such as splinting from ache, diaphragmatic dysfunction, muscular weak point, and pharmacologically depressed respiratory drive. Aggressive hydration with a balanced crystalloid solution offers the one most effective protection in opposition to contrast nephropathy. The incidence of postoperative shivering may be as high as 66% after general anesthesia. Identified danger elements embrace young age, endoprosthetic surgical procedure, and core hypothermia. Multiple research across different surgical specialties in elective and emergency cases have shown that postoperative delirium is associated with worse surgical outcomes, increased hospital size of stay, practical decline, higher charges of institutionalization, larger mortality, and better cost and resource utilization. Its location in shut proximity to the operating rooms facilitates rapid entry to anesthesiologists for consultation and assistance. Vital signs are recorded as often as necessary however no much less than every 15 minutes while the patient is in the unit. Specific requirements and suggestions for patient monitoring and therapeutic intervention could be found within the Practice Standards and Guidelines drafted by the American Society of Anesthesiologists. They are suggestions designed to assist the healthcare provider in medical choice making. The tips are based upon literature evaluation, skilled opinion, open discussion board commentary, and medical feasibility. They advocate the suitable assessment, monitoring, and therapy of the major organ system functions throughout recovery from anesthesia and surgical procedure (Box eighty. Nausea and Vomiting Periodic evaluation of postoperative nausea and vomiting ought to be routinely performed. Certain procedures might involve important blood loss and require further intravenous fluids management. Urine Assessment of urine output and of urinary voiding ought to be performed on a case-by-case basis for selected sufferers or selected procedures. Drainage and Bleeding Assessment of drainage and bleeding should be performed periodically as needed. Practice tips for postanesthetic care: an updated report by the American Society of Anesthesiologists Task Force on Postanesthetic Care. The Standards for Postanesthesia Care Practice Standards delineate the required obligation of minimal care within the clinical setting. As such, they function a threshold that can be exceeded when indicated by the clinical judgment of the practitioner. The Standards for Postanesthesia Care are up to date frequently to keep up with altering practice parameters and technologic advances. Particular attention should be given to monitoring oxygenation, ventilation, circulation, degree of consciousness, and temperature. During restoration from all anesthetics, a quantitative technique of assessing oxygenation corresponding to pulse oximetry shall be employed in the initial section of recovery. Nausea and vomiting, the necessity for upper airway assist, and hypotension had been the most frequent particular person problems. In 2002, airway/respiratory issues (183, 43%) and cardiovascular events (99, 24%) accounted for the majority of 419 recovery room incidents reported to the Australian Incident Monitoring Study database (Table eighty. In an awake affected person, opening of the higher airway is facilitated by the contraction of the pharyngeal muscular tissues on the similar time that negative inspiratory pressure is generated by the diaphragm. As a result, the tongue and soft palate are pulled forward, tenting the airway open throughout inspiration.
Cheap aziphar amexEven temporary disconnection of the airway circuit or mechanical ventilator can lead to important alveolar collapse and may thus be avoided if possible. It can additionally be increasingly acknowledged that intubated neonates must be transferred to and from the operating room with appropriate neonatal transport ventilator equipment rather than merely a bag and t-piece. Recent studies have advised that the neonatal brain may be notably vulnerable to hypotension. The differentiation between acutely aware and unconscious may also be problematic in neonates. However, what exactly constitutes a state of enough anesthesia within the neonate is unclear. Propofol and inhaled anesthetics can lead to profound cardiovascular depression in the neonate. Anesthesiologists must be notably cautious about opioid-induced bradycardia and its consequences on cardiac output. Low concentrations of potent inhaled anesthetics can be utilized with opioids to present a method of controlling hemodynamic responses with out considerably miserable the myocardium. Caudal and spinal anesthesia are relatively simple; however the safe placement of a lumbar or thoracic epidural block requires considerable talent. Epidural local anesthetic infusions can result in systemic toxicity as a outcome of immature metabolism. The following must be thought of in addition to the identical old concerns for the administration of neonates: (1) particular positioning for tracheal intubation. The anesthesiologist should establish enough intravenous entry to substitute all fluid deficits, together with loss from the defect (usually with regular saline), and ensure that cross-matched blood is out there (especially if rotational skin flaps are planned). Latex allergy precautions must be used with these kids for his or her first and all subsequent anesthetics. The major anesthesia-related issues with these defects embrace the following: (1) extreme dehydration and potential huge fluid loss from the uncovered visceral surfaces and due to partial bowel obstruction; (2) warmth loss; 77 � Pediatric Anesthesia 2451 (3) raised abdominal pressure with closure; and (4) high association of those circumstances with prematurity and other congenital defects, together with cardiac abnormalities (with omphalocele, 20%). These kids must have an adequate preoperative work-up that includes an echocardiogram to assess both anatomy and myocardial perform. Postoperative air flow is often required for these A patients as a result of a decent stomach wall closure. Infants with omphalocele or gastroschisis require careful management preoperatively to minimize the likelihood of an infection or compromise of bowel perform. For all children, enough fluid resuscitation must be provided and electrolyte imbalances corrected previous to surgery. Invasive monitoring is often essential, notably if the child has an related cardiac defect. The liberal use of muscle relaxants provides optimal surgical situations for closure of the defect. Hypotension throughout closure may happen because of pressure on the liver or caval compression. Similarly raised belly pressure during closure might impede sufficient air flow. Postoperative ventilation could additionally be needed until the stomach wall has had time to stretch to accommodate the viscera. It must be noted that increased belly stress after a tight closure (abdominal compartment syndrome) may compromise hepatic and renal perform and considerably alter drug metabolism. Staged closure with a premade spring-loaded silastic silo is getting used with rising frequency, thus minimizing repeat trips to the operating room. A small percentage of youngsters with omphalocele will also have Beckwith-Wiedemann syndrome, a condition characterized by profound hypoglycemia, hyperviscosity syndrome, congenital coronary heart disease, and related visceromegaly. Tracheoesophageal Fistula A tracheoesophageal fistula can have five or extra configurations, most of that are diagnosed after an inability to swallow because of an associated esophageal atresia (the esophagus ends in a blind pouch). In these cases the attribute diagnostic check is an incapability to move a suction catheter into the stomach. Neonates might have aspiration pneumonitis from a distal fistula connecting the stomach to the trachea by way of the esophagus or from a proximal connection of the esophagus with the trachea. Neonates with the rarer H-type fistulae have a fistula between esophagus and trachea; nonetheless the esophagus is patent with no atresia. These youngsters current later, typically with respiratory misery and chest infections. Any baby with a tracheoesophageal fistula or esophageal atresia should be suspected of getting the other anomalies. An echocardiogram to examine for a right-sided aortic arch and the presence of congenital coronary heart illness ought to be performed earlier than anesthesia. A major purpose of anesthesia is to ensure adequate air flow regardless of the presence of the fistula. Since optimistic stress air flow might inflate the abdomen by way of the fistula and trigger distension of the abdomen, it should be prevented until an endotracheal tube is placed distal to the fistula and/or the fistula is occluded or ligated. The danger of stomach distension and hypoventilation is greatest when the fistula is giant or the lung compliance is poor. The distended abdomen will further compromise air flow of the lungs, exacerbating the situation. Coordination with the surgeon is important to defining the optimal way to ensure sufficient ventilation till the fistula is occluded. Bronchoscopy is usually performed after induction to assess the size and placement of the fistula. At bronchoscopy a Fogarty catheter or comparable device may be positioned instantly within the fistula to occlude it. The endotracheal tube is ideally placed within the trachea distal to the origin of the fistula. This may be done blindly by advancing the tube right into a primary bronchus and then carefully pulling it again until equal air entry is heard. The endotracheal tube could additionally be inadvertently placed into the fistula leading to rapid gastric distension and arterial oxygen desaturation. Urgent transcutaneous gastric decompression could also be needed or intraabdominal clamping of the distal esophagus through an belly incision. Invasive blood pressure monitoring is beneficial since intraoperative arterial desaturation or hypotension might occur with manipulation of mediastinal buildings. A preductal and postductal pulse oximeter may be helpful in diagnosing an intracardiac shunting. Some surgeons prefer that the infant stay intubated postoperatively, whereas others prefer an try at extubation of the trachea. Postoperative pain could additionally be managed with a local anesthetic infusion, or intermittent bolus, through a caudal catheter threaded up to the thoracic stage, or with a paravertebral catheter positioned by the surgeon.

Buy generic aziphar lineHemodynamic resuscitation in shock is discussed in further element within the following part. Hemodynamic Resuscitation in Shock Circulatory shock is a typical situation in intensive care. It is outlined by insufficient end-organ perfusion and, if left untreated, leads to end-organ dysfunction and failure. In the landmark 2001 paper, Rivers and associates demonstrated a significant mortality decrease, 30. This concerned aggressive fluid resuscitation, allogenic pink blood cell transfusion, and inotropic assist per algorithm. Subsequent studies called numerous elements of this aggressive protocol into query. There are many surrogates used as indicators for end-organ perfusions, however all of them have their limitations and confounders. The most commonly used markers in shock are urine output, lactate, and base deficit. Urine Output Urine output is almost universally measured in critically ill patients. Despite these many limitations, the ubiquity of this measurement has made it a 83 � Critical Care Anesthesiology 2663 core component of evaluating a affected person in shock. Lactate is a product of glycolysis and even underneath regular physiologic situations is produced at a excessive rate. Further, lactate clearance can be lowered by hepatic or mitochondrial dysfunction. Thus, though elevated lactate levels are related to poor outcomes in shock states, it may not be a selected marker for organ malperfusion or ischemia. Like lactate, elevated base deficit has been related to mortality and poor clinical outcomes in shock states, especially in trauma. It can be confounded by nonperfusion-related circumstances including sodium and chloride concentrations, hypoalbuminemia, respiration, exogenous sodium bicarbonate, or sodium chloride administration. Newer strategies, corresponding to near-infrared spectroscopy, transcutaneous oximetry, and gastric pH/tonometry, might provide a extra specific and delicate endpoint target in shock. This method entails injecting a recognized quantity of chilly resolution into the best atrium and measuring the temperature change over time in the pulmonary artery. Transpulmonary Thermal Dilution or Lithium Dye Dilution Transpulmonary thermal or different dye dilution methods use the same rules of the Steward-Hamilton equation; however, the indicator answer is injected into the superior vena cava and the change is measured close to the aorta, usually on a femoral or axillary arterial line. These gadgets have been investigated in perioperative hemodynamic optimization with mixed leads to bettering clinical outcomes. Each has its personal strengths and weaknesses, however no single technology has been confirmed clinically superior. The absolute measurement accuracy of many of those gadgets is highly variable, particularly beneath rapidly altering hemodynamic conditions. Although the different strategies have been validated individually, precise interdevice settlement is probably going poor. The accuracy of these gadgets may be variable depending on the clinical scenario, and measurements could correlate poorly with different strategies. This is typically carried out from the transthoracic apical window or the deep transgastric esophageal window. As a end result, some have proposed central venous saturation from the vena cava as a surrogate. Unfortunately, the connection between central venous saturation and combined venous saturation has been found to be variable. These measurements also have their ultrasound corollaries: inferior vena cava diameter, end diastolic, and end-systolic ventricular diameter. Unfortunately, despite their widespread use, these static indicators of preload, and even their trend, have been discovered to be poor predictors of quantity responsiveness. Typically, a small bolus of roughly 100 to 250 mL of intravenous fluid is used. Similarly, a passive leg increase test resulting in transient autotransfusions from the decrease extremities has additionally been shown to be an effective predictor of fluid responsiveness. As optimistic pressure breath is delivered, proper ventricular preload is decreased and afterload increased. Meanwhile, the left ventricle preload experiences a transient increase after which a decrease as left ventricular afterload will increase. These methods may not be accurate in arrhythmias, right or left heart failure, or low-tidal volume air flow. There is increasing evidence that excess intravenous fluid administration is dangerous in critically unwell sufferers. The outcomes of those therapies are at present studied in a number of lots of of medical trials. Traditional static indicators for fluid administration have been measurements of filling pressures to the left or right eighty three � Critical Care Anesthesiology 2665 achieved in certain types of cancer (melanoma, leukemias, lymphomas) for which immunotherapy is now being used as a regular of care. Besides the desired antitumor effects, immunotherapy can also trigger distinctive toxicities ensuing from extreme immune system activation. Intensivists thus increasingly discover themselves main and coordinating multidisciplinary care for advanced oncologic patients. These agents can produce a unique set of side effects termed immune-related opposed occasions, which can be dermatologic, gastrointestinal, hepatic, endocrine, pulmonary, cardiac, or neurologic inflammatory complications. These side effects usually manifest weeks to months after initiation of the therapy. The mainstay of the management in circumstances of moderate- and high-grade toxicity is the interruption of the checkpoint inhibitor and administration of corticosteroids. Tumor necrosis factor- antagonists have been used in circumstances refractory to steroids. Echocardiography should be performed in patients with new onset dyspnea, pulmonary edema, or hypotension. Patients receiving extended immunosuppression for the therapy of checkpoint inhibitor toxicity are at an especially high risk of infectious issues (opportunistic infections, sepsis). It is essential that different precipitating components of neurologic, hemodynamic, or respiratory decline which are frequent in patients with advanced cancer are always actively excluded. The uses of ultrasound within the critically ill are manifold, from vascular entry to cardiopulmonary analysis. Because methods and technologies proceed to evolve, there are a large number of printed protocols. Ultrasound guidance can be utilized before the procedure to verify anatomy and vessel patency or, preferentially, it might be utilized in real time during the procedure. There are completely different methods, the 2 commonest being out-of-plane needle insertion with quick axis view of the vessel, or in-plane needle insertion with an extended axis view of the vessel. Ultrasound can be utilized for cannulating central venous structures, arteries, and even peripheral veins. In one study, a sensitivity and specificity of 86% and 96%, respectively, was achieved even with inexperienced practitioners.
References - Brydoy M, Oldenburg J, Klepp O, et al: Observational study of prevalence of long-term Raynaud-like phenomena and neurological side effects in testicular cancer survivors, J Natl Cancer Inst 101:1682n1695, 2009.
- Finney RP: Experience with new double J ureteral catheter stent, J Urol 120:678-681, 1978.
- Scully C, Beyli M, Ferreiro MC, et al: Update on oral lichen planus: etiopathogenesis and management, Crit Rev Oral Biol Med 9:86n122, 1998.
|
|