"Purchase generic naproxen from india, arthritis diet oatmeal."By: Keira A Cohen, M.D. - Co-Director, The Johns Hopkins Center for Nontuberculous Mycobacteria and Bronchiectasis
- Assistant Professor of Medicine
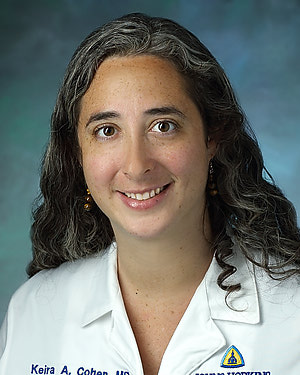 https://www.hopkinsmedicine.org/profiles/results/directory/profile/10003818/keira-cohen
Cheap 500mg naproxen visaIf cervical backbone harm is suspected, avoid any cervical maneuver that strikes the neck considerably. Flexion of the neck will transfer the tip posteriorly; extension of the neck will move the tip anteriorly; rotation of the neck to the right and left will move the tip of the tube contralateral to the direction of rotation. Based on the suspected location of the tip of the tube, the next methods will help achieve success when difficulties with tube placement are encountered. Anterior to the Epiglottis Difficulty advancing the tube past 15 cm or palpation of the tip of the tube anteriorly on the level of the hyoid bone suggests an impasse anterior to the epiglottis in the vallecula. Withdraw the tube 2 cm, decrease the degree of neck extension, and readvance the tube. No knowledge can be found on widespread obstacles encountered if the tube is placed in the left nares. Assisted ventilation will usually produce gurgling sounds when the epigastrium is auscultated. Withdraw the tube till breath sounds are clearly heard, and reattempt passage whereas applying pressure to the cricoid. If attempts proceed to end in esophageal misplacement, the next maneuver could lead to profitable tracheal intubation. This technique could additionally be particularly helpful in sufferers with cervical backbone damage as a outcome of it requires no manipulation of the top or neck. The suction catheter will usually pass easily into the trachea; the cuff can be deflated and the tube superior into the trachea. A widespread mistake is exerting an excessive quantity of drive on the ring, which can result in the tube curling up before the larynx and stopping development. There has been a case report of an Endotrol tube "kinking" at the point of sharpest curvature and causing problem with suctioning however no problems with air flow. This is incessantly profitable as a end result of the vocal cords are widely kidnapped during inhalation. Assess laryngeal anesthesia, and if topical and nebulized lidocaine has already been administered with out success, contemplate transcricothyroid anesthesia. B, Rotation of tube 90 levels counterclockwise orients the bevel of the tip posteriorly and permits passage into the larynx. The tracheal tube is then handed over the suction catheter, and the catheter is eliminated. This maneuver orients the bevel of the tube posteriorly and regularly leads to profitable passage. It will usually pass through the larynx without difficulty, and the tube can then be advanced over the catheter. Withdraw the tube 2 cm, rotate it barely away from the bulge, after which readvance it. Severe epistaxis was encountered in only 5 of 300 circumstances reported by Danzl and Thomas. B, Once breath sounds are heard, the cuff is inflated with 15 mL of air and readvanced into the laryngeal inlet. Once seated within the inlet, the cuff is deflated and the tube advanced into the trachea. Digital intubation could be notably helpful in situations with poor lighting, irregular patient positioning. Advantages embody pace and ease of placement, immunity to constraints visualizing the larynx, and little neck movement. The tip of the epiglottis should be palpated 8 to 10 cm from the corner of the mouth in average adults. Use of a stylet within the tube is elective, but the largest reported collection had good success without a stylet. If a stylet is used, place it within the tube and bend it into the type of an open J with the distal end terminating in a delicate hook. If the clinician has sufficiently long fingers, place them posterior to the arytenoids to act as a "backstop" for the tube, to both keep away from esophageal passage and assist in laryngeal placement. A variation of the strategy of digital intubation has been described for intubating a newborn. In addition, emergency physicians regularly use paralytics to facilitate orotracheal intubation. A prehospital collection of sixty six digitally intubated sufferers demonstrated an 89% success price. Introduced by Butler and Cirillo in 1960,337 the approach has undergone several current modifications that have enhanced its value as a way of creating a definitive airway when more standard methods have failed. The tracheal tube is cradled between the index and middle fingers and guided into the glottic opening. Indications embrace trismus, ankylosis of the jaw or cervical backbone, upper airway lots or swelling, unstable cervical spine injuries, and maxillofacial trauma. It can be used to convert transtracheal needle ventilation (see Chapter 6) right into a definitive airway. If fast control of the airway is needed, contemplate other alternate strategies together with a cricothyrotomy as a end result of retrograde intubation takes a quantity of minutes to arrange and carry out. The tube is guided through the use of only the index finger to palpate the epiglottis and laryngeal inlet. Bend the end of the tube and moisten each the tube and the finger with sterile water. Use the index finger of the nondominant hand to follow the tongue posteriorly and palpate the epiglottis and paired arytenoids. The tube will encounter delicate resistance as it enters the trachea, and palpation of the tube through the trachea supplies further affirmation of correct placement. A styletted tube, formed in the form of a J, is usually desired till familiarity with the process is achieved. Equipment Materials embody (1) local anesthetic and pores and skin preparation materials, (2) an 18-gauge needle, (3) a 60-cm epidural catheterneedle mixture or an 80-cm (0. Complications the chance associated with esophageal intubation is always present, and the potential for esophageal misplacement is increased in comatose or cardiac-arrest sufferers. If used in patients with a gag reflex, induction of emesis with aspiration is a risk. A high incidence of left major stem intubation was famous in a cadaveric examine,336 but scientific confirmation is lacking. Procedure and Technique Locate the three essential anatomic landmarks by palpation: hyoid bone, thyroid cartilage, and cricoid cartilage. Aspirate air to confirm position of the tip of the needle inside the lumen of the larynx. An alternative entry level is the excessive trachea, normally through the subcricoid area, with the same steps being used as described for the cricothyroid membrane. If the wire is found in the hypopharynx, grasp it with the Magill forceps and draw it out by way of the mouth.

Generic naproxen 250mg visaIf time permits, pass a nasal airway first and allow it to remain in place to physically dilate the passage. Do not direct the tube cephalad, as one might expect from the exterior nasal anatomy, but quite direct it straight backward towards the occiput and alongside the nasal ground. At 6 to 7 cm, one normally feels a "give" because the tube passes the nasal choana and negotiates the abrupt 90-degree curve required to enter the nasopharynx. This is essentially the most painful and traumatic a half of the process and have to be accomplished gently. If resistance persists despite continued gentle pressure and twisting of the tube, pass a suction catheter or endoscope down the tube and into the oropharynx to allow profitable passage of the tube over the catheter. To keep away from this problem from the outset, use a controllable-tip tracheal tube (Endotrol, Mallinckrodt Medical, Inc. The tube permits you to increase the flexion of the tube, thereby facilitating passage past this tight curve. At the purpose of maximal breath sounds, the tube is mendacity instantly in entrance of the laryngeal inlet. The tube is most easily superior into the trachea throughout inspiration, when the vocal cords are maximally open. If a cough reflex is current, the patient often coughs and becomes stridulous during this maneuver, which suggests successful tracheal intubation. The absence of such a response ought to alert the clinician to possible esophageal passage. If this occurs, direct conscious sufferers to stick out their tongue to inhibit swallowing and forestall consequent motion of the larynx. After intubation, auscultate over each lungs whereas making use of optimistic pressure ventilation. If only one lung is being ventilated, withdraw the tube till breath sounds are heard bilaterally. The optimum distance from the external nares to the tip of the tube is roughly 28 cm in males and 26 cm in females. Do not take away it from the nostril as a outcome of it will create extra trauma to the nasal delicate tissues. Remove the needle from the neck and safe the tip of the wire on the puncture web site with a hemostat. The next steps will depend upon whether a plastic sheath, additionally referred to as an obturator, is available. Threading the wire through the side port allows the tip of the tube to protrude 1 cm past the purpose at which the wire enters the larynx. Because retrograde intubation is a blind approach, it might be troublesome to determine whether the tube has entered the trachea or is impeded by extra proximal constructions. If in doubt, pull the tube again 2 cm, rotate it ninety levels counterclockwise, and then readvance the tube. If a sheath is out there, after grasping the wire from the mouth, thread the plastic sheath over the wire till it comes to relaxation towards the anterior laryngeal wall. If any resistance on the arytenoids or vocal cords is encountered, pull the tube again 1 to 2 cm and rotate it ninety levels counterclockwise. One benefit of the antegrade sheath is that it lies freely in the larynx, allowing more posterior passage by way of the widest distance between the cords. A 90� counterclockwise tube rotation and jaw traction will help the tube pass into the laryngeal inlet. The potential for hemorrhage is minimized by taking care to puncture the cricothyroid membrane in its decrease half to keep away from the cricothyroid artery. A small incidence of soft tissue infection is reported with translaryngeal needle procedures, and ensuring that the wire is withdrawn from the mouth somewhat than the neck can reduce this downside. The last complication, failure to obtain intubation, has been mitigated by addition of the antegrade sheath over the wire. A methodology of replacing the tube with out dropping control of the tracheal lumen is most popular. This could be achieved by passing a information down the defective tube, withdrawing the tube while leaving the guide in place, and introducing a new tube over the information and into the trachea. Tracheal Retrograde Intubation 1 Place a saline-filled needle through the cricothyroid membrane. B) Pass the antegrade sheath over the wire into the trachea whereas maintaining each ends of the wire taut. This is the crucial portion of the process as a end result of solely a small portion of the sheath is in the trachea. Bougies are typically simpler to find within the airway cart and intubators are extra familiar with their use. They most frequently happen when patients suddenly pull out their very own tube or during transport. Procedure and Technique Before the procedure, sedate and restrain the affected person correctly. While applying cricoid strain, withdraw the defective tube over the information, and take care to not dislodge the guide when removing the tube. At this juncture, it may be helpful to carry out a jaw-thrust or chin-lift maneuver to facilitate passage via the pharynx. If this occurs, withdraw the tube 1 to 2 cm, rotate it ninety levels counterclockwise, after which readvance it. After the tube is visualized clearly in the trachea, take away the information, inflate the cuff, and ventilate the affected person. Although the definition of a difficult airway will change as our capacity to visualize the laryngeal inlet continues to improve, the problem of emergency airways will persist. Mastery of technique, advance preparation of apparatus, and expertise in scientific decision-making are essential. Scenario visualization and superior simulation models can present a wonderful technique of working towards the difficult choice making and technical maneuvers necessary for efficient emergency airway administration. Russell T, Ng L, Nathan E, et al: Supplementation of ordinary preoxygenation with nasal prong oxygen or machine oxygen flush during a simulated leak state of affairs. Ooi R, Pattison J, Joshi P, et al: Pre-oxygenation: the Hudson masks in its place method. Hayes-Bradley C, Lewis A, Burns B, et al: Efficacy of Nasal Cannula Oxygen as a Preoxygenation Adjunct in Emergency Airway Management. Miguel-Montanes R, Hajage D, Messika J, et al: Use of high-flow nasal cannula oxygen therapy to forestall desaturation throughout tracheal intubation of intensive care sufferers with mild-to-moderate hypoxemia. Lane S, Saunders D, Schofield A, et al: A potential, randomised managed trial evaluating the efficacy of pre-oxygenation in the 20� head-up vs supine place. Wimalasena y, Burns B, Reid C, et al: Apneic oxygenation was associated with decreased desaturation rates during rapid sequence intubation by an Australian helicopter emergency drugs service. Shiga T, Wajima Z, Inoue T, et al: Predicting difficult intubation in apparently regular sufferers: a meta-analysis of bedside screening take a look at efficiency. Salimi A, Farzanegan B, Rastegarpour A, et al: Comparison of the higher lip bite check with measurement of thyromental distance for prediction of adverse intubations. Honarmand A, Safavi M, Ansari N: A comparability of between hyomental distance ratios, ratio of top to thyromental, modified Mallamapati classification test and upper lip chunk take a look at in predicting tough laryngoscopy of patients undergoing common anesthesia.
Syndromes - Fluids by IV
- Abnormal reflexes
- Delirium
- Alopecia (hair loss)
- Lung problems such as emphysema and chronic bronchitis, or asthma that is harder to control
- Birth defects that have damaged your intestines
- High blood pressure or heart disease
- Amount swallowed
Purchase generic naproxen from indiaNote the box-shaped mark to the left of the complexes (arrows); this is a graphic representation of the calibration for the tracing. The calibration on this tracing was (inexplicably and unexpectedly) modified to 20 mm/ mV by the computer, not by the operator. A was recorded minutes later with correction of calibration to the standard 10 mm/mV and was unchanged from baseline tracings. These additional, or nontraditional, leads embrace posterior leads (V7, V8, and V9), proper ventricular leads (especially V4R), and procedural leads (transvenous pacemaker wire placement and pericardiocentesis). Place leads V7, V8, and V9 on the identical horizontal aircraft as V6, with V7 at the posterior axillary line, V8 on the tip of the left scapula, and V9 near the border of the left paraspinal muscle tissue. An additional electrode, V7, may be used and is placed on the posterior axillary line equidistant from electrode V8. Place right-sided leads V1R to V6R on the chest as a mirror picture of the standard precordial leads. This alteration in lead placement is used to investigate the potential for a right-sided acute myocardial infarction that is in all probability not appreciated with regular lead placement. This patient was discovered to have a subtotal proximal occlusive lesion of his proper coronary artery at cardiac catheterization. Next, advance it till contact is made with the endocardium and the ventricle is captured. This type of monitoring will help in appropriate positioning of the catheter within the pericardial area. In such cases, it could be essential to place the pacing wire without the advantage of fluoroscopy. In such cases the recommendation is to advance the wire underneath electrocardiographic steering with the affected person connected to the limb leads of a grounded electrocardiographic machine and the pacing wire linked to the V lead (see Chapter 15). Importantly, this reduction in time to administration is seen in city, suburban, and rural settings, whatever the transport time or kind of reperfusion strategy chosen for the particular affected person. Alteration in Amplitude and Paper Speed Most 12-lead electrocardiography machines right now allow alteration of both amplitude and paper pace from the fundamental 10-mm/ mV and 25-mm/sec requirements, respectively. Increasing the amplitude to double the standard or 20 mm/mV, can improve the prominence of smaller deflections such because the P wave, and may improve recognition of the atrial rhythm. This technique is most advantageous when assessing patients with marked atrial or ventricular tachycardia. Increasing the paper speed exaggerates any current irregularity (such as in atrial fibrillation) and may enhance recognition of smaller deflections, such as P waves, within the presence of a significant tachycardia. A variety of various lead techniques requiring fewer electrodes have been described. Other different lead placements to improve detection of atrial activity have additionally been described44�46 (Table 14. Because of the speedy price, the precise P waves are difficult to discern, thus making determination of the rhythm tough. In addition, the vertical sternal leads are positioned over bone, which may scale back artifact attributable to muscle activity on recordings. Limb-Precordium Leads A sequential pattern of bipolar leads on the chest, termed limb-precordium leads, has been proposed together with the original Einthoven limb leads. Esophageal Leads the esophageal lead (E) was first described by Brown in the Nineteen Thirties. Once within the esophagus, the situation of the electrode is decided either by fluoroscopy or by making a series of low to high esophageal recordings. The place of the electrode within the esophagus is adjusted by slowly pulling the electrode wire out the nares or mouth. In normal adults, leads E15�25 (the electrode is located within the esophagus 15 to 25 cm from the nares) generally records atrial exercise; E25�35, activity of the atrioventricular groove; and E40�50, activity of the left ventricular posterior floor. Central Venous Catheter Intracardiac Leads For sufferers in whom a central venous catheter was placed for vascular entry (or for other causes such as cardiac pacing, hemodialysis, or Swan-Ganz monitoring) that catheter, when filled with saline, can be used as a modified intracardiac electrode for recording of atrial exercise. Once full of saline, a needle was then left in a aspect access port of the catheter and attached via an alligator clip to lead V1. A multitude of prospects for misconnection of the limb electrodes exists; some of the most likely are summarized here. Reversal of the leg electrodes is largely insignificant in that the potentials at the left and proper legs are basically the identical. A patient with a historical past consistent with acute coronary syndrome was delivered to the emergency department after this electrocardiogram was recorded in a clinic. Precordial Electrode Misplacement and Misconnection in distinction to the limb electrodes, the precordial electrodes are extra susceptible to misplacement, particularly when variations in physique habitus. This may cause some variability within the amplitude and morphology of the complexes within the precordial leads. Note that the usual precordial progression of R-wave development in leads V2 and V3 is disrupted within the tracing displayed in A. It has been noticed that leads V1 and V2 are usually positioned too excessive and that the lateral leads are placed too laterally and too low. McCann and colleagues56 demonstrated a excessive degree of variability between experienced clinicians in figuring out anatomic landmarks for precordial electrocardiographic electrode placement. There was regularly a big distinction within the measured distance from the precise to the "standardized" electrode position that ranged between 0 and one hundred and five mm in the vertical direction (mean, 14 mm; median, 10 mm), and between zero and 120 mm within the horizontal airplane (mean, 17 mm; median, 10 mm). An abrupt change in wave morphology evolution- adopted by a seeming return to normalcy within the next lead-is a great clue to misconnection of the precordial electrodes. It could be attributed to both physiologic (internal) or nonphysiologic (external) sources; the former consists of muscle activity, affected person movement, and poor electrode contact with the pores and skin. Tremors, hiccups, and shivering could produce frequent, slim spikes on the tracing and simulate atrial and ventricular dysrhythmias. Minimizing pores and skin impedance and artifact may be achieved by: (1) avoiding electrode placement over bony prominences, major muscular tissues, or pulsating arteries; (2) clipping somewhat than shaving thick hair at electrode sites; and (3) cleaning, and most significantly, drying the skin floor earlier than reapplying the electrode if the tracing features substantial artifact. Nonphysiologic artifact is most frequently caused by 60-Hz electrical interference, which is ascribable to various other sources of alternating present near the affected person. As a clue to the artifact, the affected person was clinically stable and asymptomatic in the course of the event, apart from his rigors. Electrocardiographic artifact should be thought of when the medical picture signifies stability, and establishment and coincident procedures are in progress. Differentiation of artifact from true electrocardiographic abnormality is intuitively important; furthermore, clinical consequences have been reported that are immediately attributable to confusion of artifact with illness. Brady W, Adams M, Perron A, et al: the influence of the 12-lead electrocardiogram in the evaluation of the emergency department patient [abstract]. Surawicz B, uhley H, Borun R, et al: Task Force I: standardization of terminology and interpretation. American Heart Association Committee Report: Recommendations for standardization of leads and of specs for devices in electrocardiography and vectorcardiography. Lapostolle F, Petrovic T, Bernot B, et al: Comparison of the utilization of conventional and prewired electrodes for electrocardiography in an emergency setting: the Spaghetti Study.

Cheap naproxen online visaThe extent of organ involvement should be ascertained, and management must be centred on symptomatic control and prevention of issues. Patients, particularly with diffuse scleroderma, could expertise severe renal disease which may precipitate scleroderma renal crises. These may present with a sudden onset of hypertension, acute kidney harm and proteinuria, and can also present with complications and fatigue. Patients usually present with symmetrical proximal muscle weak point and sparing of the distal extremities. E Both polymyositis and dermatomyositis could have systemic features, such as fever, arrhythmias and arthritis. Anti-Mi-2 antibodies are highly particular for dermatomyositis however are only seen in a few quarter of patients. P Both polymyositis and dermatomyositis may be associated with an underlying malignancy, and this must be investigated thoroughly. Treatment involves avoiding sun publicity and utilizing sunblock (in dermatomyositis) and steroids first line, and immunosuppressive therapy with azathioprine or cyclophosphamide if unresponsive. Epidemiology: � Women are 2 to four occasions more more probably to have the condition than males � Patients are usually above the age of 50 10. This disrupts the layer between the tunica intima and the media of the artery, whilst leucocyte proliferation and angiogenesis proceed to happen. These processes narrow the vessel lumen, leading to ischaemia and producing symptoms similar to headaches or blindness, relying on which arteries are affected. E It is important not to delay treatment while ready for confirmation of the temporal artery biopsy. In addition, the temporal artery biopsy may be adverse in up to half of affected people, in all probability as a end result of the sampled area has remained unaffected by disease. Patients must be supplied corticosteroids first line, with other immunosuppressive medications getting used if treatment stays ineffective. The American College of Rheumatology identifies six standards: � Asthma � Sinusitis � Peripheral blood eosinophilia >10% � Pulmonary infiltrates � Histological demonstration of vasculitis � Polyneuropathy (or mononeuritis multiplex) Any 4 of these confer a really high probability of the analysis. Descriptively, these options include the next: Condyle: a rounded articular floor covered with articular (hyaline) cartilage. Facet: a lat, smooth articular floor, usually covered with articular (hyaline) cartilage. Foramen: a round or oval "gap" within the bone for passage of one other construction (nerve or vessel). Fossa: a "cuplike" melancholy in the bone, normally for articulation with another bone. Bone Development Bones develop in one of many following two ways: Intramembranous formation: most lat bones develop on this means by direct calcium deposition right into a mesenchymal (primitive mesoderm) precursor or model of the bone. Endochondral formation: most lengthy and irregularly shaped bones develop by calcium deposition right into a cartilaginous model of the bone that provides a scafold for the long run bone. Spongy (trabecular or cancellous): is a much less dense trabeculated network of bone spicules making up the substance of most bones and surrounding an internal marrow cavity. Epiphysial plate: the site of progress in length; it incorporates cartilage in actively growing bones. Diaphysis: the shaft of an extended bone, which represents the first ossiication middle and the site the place progress in width occurs. As a residing, dynamic tissue, bone receives a wealthy blood provide from: Nutrient arteries: normally one or several larger arteries that move via the diaphysis and provide the compact and spongy bone, in addition to the bone marrow. Metaphysial and epiphysial arteries: often arise from articular branches supplying the joint. Periosteal arteries: numerous small arteries from adjacent vessels that offer the compact bone. Chapter 1 Introduction to the Human Body 9 Epiphysial capillaries 1 Perichondrium Periosteum Proliferating hyaline cartilage Canals, containing Hypertrophic capillaries, periosteal calcifying mesenchymal cells, cartilage and osteoblasts Thin collar of cancellous bone Cancellous endochondral bone laid down on spicules of calcified cartilage Primordial marrow cavities A. At 10 weeks Articular cartilage Bone of epiphysis Calcified cartilage Epiphysial (secondary) ossification middle Outer a part of periosteal bone transforming into compact bone Central marrow cavity Epiphysial ossification centers Proliferating progress cartilage Proximal epiphysial progress plate Sites of progress in size of bone Distal epiphysial development plate Hypertrophic calcifying cartilage D. At delivery Calcified cartilage Endochondral bone laid down on spicules of degenerating calcified cartilage Proliferating progress cartilage Diaphysis; progress in width happens by periosteal bone formation Metaphysis Bone of epiphysis Articular cartilage E. Cavitation of the first ossiication heart and invasion of vessels, nerves, lymphatics, purple marrow elements, and osteoblasts. Diaphysis elongation, formation of the central marrow cavity, and appearance of the secondary ossiication facilities in the epiphyses. Types of Joints Joints are the sites of union or articulation of two or extra bones or cartilages, and are classiied into one of the following three sorts. Cartilaginous (amphiarthroses): bones joined by cartilage, or by cartilage and ibrous tissue. Synovial (diarthroses): on this commonest kind of joint, the bones are joined by a joint cavity illed with a small amount of synovial luid and surrounded by a capsule; the bony articular surfaces are coated with hyaline cartilage. Fibrous joints embody sutures (lat bones of the skull), syndesmoses (two bones linked by a ibrous membrane), and gomphoses (teeth itting into ibrous tissue-lined sockets). Cartilaginous joints embrace main (synchondrosis) joints between surfaces lined by hyaline cartilage (epiphysial plate connecting the diaphysis with the epiphysis), and secondary (symphysis) joints between hyaline-lined articular surfaces and an intervening ibrocartilaginous disc. Primary joints enable for progress and some bending, whereas secondary joints enable for strength and a few lexibility. Synovial joints usually allow for appreciable movement and are classiied based on their form and the type of movement that they allow (uniaxial, biaxial, or multiaxial movement). Secondary cartilaginous Saddle: are biaxial joints for lexion, extension, abduction, adduction, and circumduction. Condyloid (ellipsoid; generally classiied separately): are biaxial joints for lexion, extension, abduction, adduction, and circumduction. Ball-and-socket (spheroid): are multiaxial joints for lexion, extension, abduction, adduction, mediolateral rotation, and circumduction. Smooth: nonstriated muscle ibers that line varied organ methods (gastrointestinal, urogenital, respiratory), attach to hair follicles, and line the walls of most blood vessels (sometimes simplistically referred to as involuntary muscle). Skeletal muscle is divided into fascicles (bundles), which are composed of muscle ibers (muscle cells). Each myoibril is composed of many myoilaments, that are composed of particular person myosin (thick ilaments) and actin (thin ilaments) that slide over one another during muscle contraction. At the gross degree, anatomists classify muscle on the premise of its form: Flat: muscle that has parallel ibers, normally in a broad lat sheet with a broad tendon of attachment referred to as an aponeurosis. Cardiac: striated muscle ibers that make up the partitions of the center and proximal parts of the great veins the place they enter the guts. Plane 12 Chapter 1 Introduction to the Human Body Clinical Focus 1-4 Fractures Fractures are categorized as either closed (the pores and skin is intact) or open (the skin is perforated; typically referred to as a compound fracture). Additionally, the fracture could also be categorised with respect to its anatomical look. Closed fracture with hematoma Open fracture with bleeding Intraarticular fracture with hemarthrosis Pathologic fracture (tumor or bone disease) Greenstick fracture Torus (buckle) fracture In youngsters Transverse fracture Oblique fracture Spiral fracture Comminuted fracture Segmental fracture Impacted fracture Avulsion (greater tuberosity of humerus avulsed by supraspinatus m.

Discount naproxen 500 mg onlineThe mucosa in segments of the pharyngeal esophagus vibrates in response to airflow, thereby creating speech. Once the tracheocutaneous fistula has epithelialized, the catheter could also be inserted. After the tract has totally matured, most sufferers can change their catheter at residence. One milliliter of sterile saline is instilled into the catheter, and a cleansing rod is inserted as far as potential. The cleansing rod is inserted and extracted 3 times to remove secretions and encrustations from the lumen of the catheter. The stoma must be cleaned twice every day and inspected thoroughly for signs of an infection. All patients ought to be given supplemental oxygen by nasal cannula during catheter upkeep procedures. Adequate humidification, cleaning, and systemic hydration will help scale back the incidence of mucous blockage. Early problems (developing inside 3 weeks after the procedure) occur in roughly 30% of sufferers and embrace bleeding, an infection, pneumothorax, costochondritis, and dislodgement (which can be attributable to coughing). Life-threatening airway obstruction ensuing from the formation of a giant mucous ball has been reported. Obstruction throughout the catheter tubing may trigger a whistling sound from the oxygen tank humidifier. Always look at the patient for signs of subcutaneous air and catheter dislodgement. If routine broad-spectrum antibiotics are used by the affected person, Candida infections can develop on the stoma. Such infections are more frequent in patients receiving systemic antibiotics or long-term corticosteroids or those with diabetes. Many patients with chondritis have a deep, indurated, nonfluctuant lump across the tract that may be tender to palpation. If important bleeding is identified or suspected, consult a specialist on an emergency foundation and handle the airway definitively as clinically indicated (see the part on Major Bleeding). Manage skin and pulmonary infections with the methods mentioned for tracheostomy care. Stents Tracheal stenosis and tracheomalacia are identified problems of synthetic airways. Management choices embrace surgery and placement of silicone stents in the trachea. Morbidly obese sufferers are particularly in danger for lifethreatening complications associated to tracheostomy. Dislodgement is particularly associated with increased rates of morbidity and mortality. In addition to standard monitoring, use continuous capnography, if obtainable, to forestall delay within the recognition of tube dislodgement. The patient should be positioned with the neck in slight extension, and the top of the mattress must be elevated to roughly 30 degrees. If the stoma tract has not healed or seems to be contaminated, change the catheter through a modified Seldinger method. Ask the patient to sit upright, maintain a pillow to the stomach, and cough forcefully after three deep inspirations. If the tube is obstructed, deflation of the tracheostomy cuff will not be sufficient to allow adequate ventilation as a end result of exterior compression attributable to abnormal neck anatomy might happen. Laryngectomy Patients It is important to distinguish the affected person with a routine tracheostomy from the patient with a laryngectomy as this might doubtlessly limit the ability to present air flow by the use of the higher airway. A affected person with a partial laryngectomy will have a contiguous upper and lower airway, and interventions by the use of the higher airway could also be limited. Partial laryngectomy sufferers also needs to be ventilated through their stoma, and their mouth and nose should be saved closed to avoid air escape. First, it is important to examine the laryngectomy stoma for any mechanical obstruction. External air flow with a pediatric face masks or laryngeal masks airway could be carried out. The approximate distance between the pores and skin of the stoma and carina is just roughly 6 cm. Pediatric tracheostomy tubes hardly ever have inflatable cuffs, except for these used for certain particular indications. Continuous capnography might detect certain tracheostomy complications and is beneficial. Age tips can be helpful, however they may not be reliable in pediatric sufferers due to complex medical issues. Premature infants may be small for their age and weight, thus making estimation of tube dimension much more troublesome. When the tracheostomy tube is seated accurately in a pediatric patient, it ought to prolong at least 2 cm past the stoma and no nearer than 1 to 2 cm above the carina. Its curvature should be such that when the tube is placed appropriately, the distal portion of the tube is concentric and collinear with the trachea. After replacing a tracheostomy tube, verify its position by auscultating breath sounds, using capnography, and confirming the placement of the distal tip with a chest radiograph. In comparison, patients with central nervous system issues, respiratory misery syndrome, and congenital coronary heart problems are less prone to expertise issues. Systemic absorption of lithium is unlikely to cause medical symptoms in adults but could additionally be a consideration in children. Use humidifiers frequently to keep secretions unfastened and help stop obstruction of the tube. Suctioning Suctioning suggestions in pediatric sufferers clearly support using a premeasured suction catheter to cut back the rate of mucosal irritation and to limit the event of granulation tissue. Depth of insertion can be estimated by measuring a similar tube earlier than inserting the suction catheter. In children with fenestrated tracheostomy tubes, suction catheters could accidentally undergo the fenestrations and cause mucosal irritation. Chronic respiratory problems embody tracheomalacia, tracheal stenosis, vocal twine paralysis, and vocal wire fusion. It typically occurs in the tracheal lumen both at the superior margin of the tracheostomy or on the degree of the tip of the tube. The development of granulation tissue is the end result of persistent mucosal irritation and irritation. Any affected person with a clinically significant granuloma must be evaluated by a pediatric specialist for definitive care. Pneumomediastinum and pneumothorax are generally thought to be early problems of tracheostomy, but they need to always be thought of in a pediatric tracheostomy patient.
Purchase 500 mg naproxen fast deliveryIn infants and small children, an adhesive sensor unit is most well-liked and regularly positioned on the fingers and toes. Probes can be secured in place over the palm, heel, or lateral aspect of the foot with a gauze or wrap. Electrocautery Electrical interference from units corresponding to electrocautery can impair the accuracy of pulse oximetry. Such interference could be reduced by increasing the space between the surgical website and the probe. Conclusions Pulse oximetry is a widely obtainable expertise that gives a simple, noninvasive, and usually reliable methodology of monitoring oxygenation. Because measurements are steady, pulse oximetry permits earlier detection of hypoxic episodes than intermittent arterial blood gas evaluation does. Frequent measurements can result in earlier corrective measures and prevention of antagonistic penalties. Future Directions New units that target regional detection of O2 saturation, specifically cerebral oximetry, are being studied for various scientific functions related to emergency medication. Oxygenation and ventilation are distinct physiologic functions that are assessed in each intubated and spontaneously respiration sufferers. Terminology the ancient Greeks believed there was a combustion engine inside the body that gave off smoke (capnos in Greek) within the form of a breath. Technology Capnography turned a routine a half of anesthesia apply in Europe within the Nineteen Seventies and within the united States in the Nineteen Eighties. A capnography waveform (arrow) is displayed, as is a capnometry numerical reading (37). Patients with obstructive lung disease could have a more rounded ascending phase and an upward slope within the alveolar plateau. Indications for Intubated Patients � � � � � � Physiology the capnogram, which corresponds to a single tidal breath, consists of 4 phases (ascending section, alveolar plateau, inspiratory limb, dead area ventilation). Experimental proof signifies that interruptions in chest compressions are adopted by sustained durations throughout which move progressively returns to pre-interruption ranges. Sustained hyperventilation is also detrimental and associated with worse neurologic end result in severely brain-injured patients. The presence of a traditional waveform denotes a patent airway and spontaneous respiratory. Capnography can be utilized to assess and triage critically sick or injured sufferers and actively seizing patients. Capnography is a reliable, accurate monitoring modality for actively seizing patients. In contrast, capnography will detect absence of air motion and subsequently exhibits a flatline waveform. Modified from Krauss B: Capnography as fast assessment and triage device for chemical terrorism, Pediatr Emerg Care 21:493, 2005. Both central and obstructive apnea can be detected nearly instantaneously by capnography (Table 2. Obstructive apnea is characterised by loss of the capnogram with continued chest wall movement and absent breath sounds. The response of the capnogram to airway alignment maneuvers can further distinguish upper airway obstruction from laryngospasm. Capnography is more delicate than medical evaluation of ventilation in detecting apnea together with other respiratory problems. This leads to extra consciousness of respiratory problems related to procedural sedation, which is adopted by acceptable and timely interventions. Acute bronchospasm ends in a capnogram with a curved ascending part and an upsloping alveolar plateau. Two types of drug-induced hypoventilation happen throughout procedural sedation and analgesia (see Table 2. Three possibilities exist: (1) ventilation may remain steady with the low�tidal volume breathing resolving over time as drug ranges in the central nervous system decrease following redistribution, (2) hypoventilation might progress to periodic respiration with intermittent apneic pauses (which may resolve spontaneously or progress to central apnea), or (3) hypoventilation may progress directly to central apnea. The low�tidal quantity respiration that characterizes hypopneic hypoventilation increases useless house ventilation on account of inhibition of the normal compensatory mechanisms by drug results. Determining the Adequacy of Ventilation in Patients With Altered Mental Status Patients with altered mental status, together with these with alcohol intoxication, intentional or unintentional drug overdose, patients requiring chemical restraint, and postictal sufferers (especially these treated with benzodiazepines), might have impaired ventilatory function. Capnography can differentiate between sufferers with effective air flow and those with ineffective ventilation, as properly as present continuous monitoring of ventilatory developments over time to identify patients at risk for worsening respiratory despair. These points have largely been resolved in the newer-generation capnography monitors. Capnography is best when assessing a pure ventilation, perfusion, or metabolism problem. Capnographic findings in sufferers with blended air flow, perfusion, or metabolism problems are tough to interpret. Absolute values and even tendencies over time could also be difficult to interpret in these situations. Limitations Significant technical issues have historically restricted the effective medical use of capnography. Kikuchi Y, Okabe S, Tamura G, et al: Chemosensitivity and perception of dyspnea in patients with a historical past of near-fatal bronchial asthma. Magadle R, Berar-Yanay N, Weiner P: the risk of hospitalization and near-fatal and fatal bronchial asthma in relation to the notion of dyspnea. British Thoracic Society Scottish Intercollegiate Guidelines Network: British guideline on the management of asthma. Pedersen T, Nicholson A, Hovhannisyan K, et al: Pulse oximetry for perioperative monitoring. Sutcu Cicek H, Gumus S, Deniz O, et al: Effect of nail polish and henna on oxygen saturation determined by pulse oximetry in healthy young grownup females. Sanfilippo F, Serena G, Corredor C, et al: Cerebral oximetry and return of spontaneous circulation after cardiac arrest: A systematic evaluate and meta-analysis. Genbrugge C, Dens J, Meex I, et al: Regional cerebral oximetry throughout cardiopulmonary resuscitation: helpful or ineffective Kane I, Abramo T, Meredith M, et al: Cerebral oxygen saturation monitoring in pediatric altered psychological status patients. Bouzat P, Oddo M: Non-invasive cerebral oximetry for the emergent resuscitation of comatose cardiac arrest patients: is there still some light at midnight Beynon C, Kiening Kl, Orakcioglu B, et al: Brain tissue oxygen monitoring and hyperoxic treatment in sufferers with traumatic mind damage. Colman Y, Krauss B: Microstream capnograpy technology: a brand new method to an old problem. Berengo A, Cutillo A: Single-breath evaluation of carbon dioxide concentration data. Grmec S: Comparison of three totally different methods to confirm tracheal tube placement in emergency intubation. PantazopoulosC,XanthosT,PantazopoulosI,etal:Areviewofcarbon dioxide monitoring during adult cardiopulmonary resuscitation. Touma O, Davies M: the prognostic worth of end tidal carbon dioxide throughout cardiac arrest: a scientific evaluation. Bou Chebl R, Madden B, Belsky J, et al: Diagnostic value of finish tidal capnography in patients with hyperglycemia in the emergency department. Soleimanpour H, Taghizadieh A, Niafar M, et al: Predictive value of capnography for suspected diabetic ketoacidosis within the emergency department.
Aframomum melegueta (Grains Of Paradise). Naproxen. - Use as a stimulant.
- Are there safety concerns?
- How does Grains Of Paradise work?
- Dosing considerations for Grains Of Paradise.
- What is Grains Of Paradise?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96660

Naproxen 250 mg on-lineIn patients with in any other case limited peripheral access, it can be cannulated as follows. Take the cannula and align it within the direction of the vein with the point aiming toward the ipsilateral shoulder. Puncture halfway between the angle of the jaw and the midclavicular line while frivolously compressing the vein with the free finger above the clavicle. A, Note that traction on the vein is utilized with the thumb of the nondominant hand whereas the index finger tamponades the vessel (arrow) (essentially serving as a tourniquet) close to the clavicle. Use a half-inchwide strip of tape, adhesive aspect up, under the hub of the catheter and fold it over in a bow-shaped manner. Saline locks may be connected to needleless hubs to prevent unintentional needle damage. Sterile gauze or transparent, semipermeable, polyurethane dressings may be left in place till removal of the catheter with out increasing infection rates, as lengthy as the site is often evaluated. Until lately, heparin solutions had been used to flush catheters and maintain patency, however heparin may cause issues such as hemorrhage. Complications embrace brachial artery puncture, hematoma, and transitory paresthesias. Prepare the positioning within the traditional manner and apply a tourniquet above the antecubital house. At some extent instantly medial or lateral to the pulse, insert an angiocatheter with an attached syringe and advance it at a 45-degree angle while maintaining suction on the syringe. Phlebitis, infiltration, an infection, nerve injury, air embolism, bruising, and thrombosis are the most common complications and infrequently trigger vital morbidity or fatality. Phlebitis necessitates removing of the catheter and substitute on one other extremity. Particulates from reconstituted drugs, degradation products, precipitates, glass from vials, and different foreign debris could all play an element in postinfusion phlebitis. B, After incising and cleansing the infected subcutaneous tract, a gauze pack was positioned for twenty-four hours and oral antibiotics got with good outcomes. It most frequently happens in sufferers with thermal injury and long-term or decrease extremity cannulation. Tissue or interstitial infiltration happens when the catheter is dislodged from the vein during infusion. Extravasation of certain infusions, corresponding to hypertonic options, vasopressors, or chemotherapeutic agents, nevertheless, poses a big risk for necrosis and pores and skin sloughing when infiltration and extravasation occur. Any peripheral nerve is doubtlessly vulnerable to a needle-induced injury, and sequelae can range from a minor motor or sensory abnormality to full paralysis. Nerve injury could also be because of direct injury by the needle, intraneural microvascular harm from hematomas, or toxic effects of the agent injected. Should a patient complain of numbness or severe pain after a needle puncture, cease the injection immediately. If the return fluid appears bloody, discard the syringe and then gently flush the saline lock and resume the infusion. Symptoms include chest pain, shortness of breath, sudden vascular collapse, cyanosis, and hypotension. Invasive maneuvers embody aspiration of air via a central venous catheter and even thoracotomy with direct aspiration from the heart (see Chapter 18). If the air is near a Y-connector, one can use a needle and syringe to instantly remove it. Record and date the time of catheter insertion in an obvious location close to the insertion website. Do not palpate the insertion website after the pores and skin has been cleansed with antiseptic. Wash arms earlier than and after palpating, inserting, changing, or dressing any intravascular access web site. Pain on the infusion website or the alarm sounding on an infusion pump device requires inspection of the infusion website for extravasation. There are few downsides to this intervention, though hypotension is a theoretical aspect effect as a outcome of phentolamine is an -adrenergic antagonist. To inject phentolamine, place 5 mg in a vial and dilute with equal components of saline (final form: 5 mg in 2 mL). For massive areas, use two vials with the contents of each vial injected 10 minutes apart through a 25- to 27-gauge needle or a tuberculin syringe. The complete space of skin blanching, or suspected space of extravasation, is injected with multiple small aliquots of the answer, roughly 0. Hyaluronidase is probably benign and has been suggested prior to now to ameliorate some results of extravasation of other solutions. Aminophylline Calcium chloride 10% Carmustine Chlordiazepoxide Colchicine Crystalline amino acids 4. Thus, any grievance of pain throughout infusion or signs of tissue swelling should prompt an investigation for extravasation. Phentolamine, injected subcutaneously to reverse vasoconstriction, is the most typical method, however its efficacy has not been nicely studied. Extravasation of hypertonic dextrose, phenytoin, and vasoconstrictors or vasopressors will cause comparable necrosis. B, Full-thickness tissue injury from doxorubicin extravasation, not obvious until 7 to 10 days after the infusion. The affected person could complain of pain and burning on the time of infusion, however skin sloughing may be delayed for many days. Injury from extravasation of phenytoin could be minimized or prevented by using dilute options, no extra than a 2-mg/ mL focus (1 g in 500 mL saline), or through the use of fosphenytoin instead of phenytoin. Multiple subcutaneous injections in and around the area of extravasation with a 25-gauge needle: 4 mL of 10% sodium thiosulfate + 6 mL water. Inject subcutaneously in and around the area of extravasation with a 25-gauge needle: one hundred fifty units (1 mL). Inject subcutaneously in and across the area of extravasation with a 25-gauge needle. Inject subcutaneously in and around the space of extravasation with a 25-gauge needle: hydrocortisone, 500 mg diluted in 500 mL saline. Vinca alkaloids (vincristine, vinblastine, and vinorelbine) Doxorubicin Doxorubicin, daunorubicin, and mitomycin Mitomycin Nonspecific Nonspecific a Hyaluronidase Granulocyte-macrophage colony-stimulating factorc Dimethyl sulfoxide (free radical scavenger) Pyridoxinec Saline Corticosteroidsd Many of those interventions are anecdotal and none are assured to reverse or ameliorate tissue injury. Controversy surrounds the actual benefit, and no randomized potential trials have been carried out for lots of the advised regimens. This may include sufferers with no palpable or visible peripheral veins, historical past of intravenous drug use or multiple previous peripheral lines causing scarring or thrombosis, obesity, or previous surgeries causing distortion of the anatomy. Use of ultrasound to obtain peripheral intravenous access has been discovered to increase the speed of success, lower both the time to placement and the number of makes an attempt, and improve general patient satisfaction.
Purchase naproxen 500mg onlineMaruyama K, yamada T, Kawakami R, et al: Randomized cross-over comparability of cervical-spine motion with the AirWay Scope or Macintosh laryngoscope with in-line stabilization: a video-fluoroscopic examine. Maruyama K, yamada T, Kawakami R, et al: Upper cervical backbone movement during intubation: fluoroscopic comparability of the AirWay Scope, McCoy laryngoscope, and Macintosh laryngoscope. Uakritdathikarn T, Asampinawat T, Wanasuwannakul T, et al: Awake intubation with Airtraq laryngoscope in a morbidly overweight patient. Combes X, Sauvat S, Leroux B, et al: Intubating laryngeal mask airway in morbidly overweight and lean patients: a comparative study. Frappier J, Guenoun T, Journois D, et al: Airway administration using the intubating laryngeal masks airway for the morbidly overweight affected person. Riley E, DeGroot K, Hannallah M: the high-pressure characteristics of the cuff of the intubating laryngeal mask endotracheal tube. Joo H, Naik V: Conventional tracheal tubes for intubation by way of the intubating laryngeal mask airway. Kundra P, Sujata N, Ravishankar M: Conventional tracheal tubes for intubation by way of the intubating laryngeal masks airway. Kundra P: Conventional endotracheal tubes for intubation through the intubating laryngeal masks airway. Zhu T: Conventional endotracheal tubes for intubation through the intubating laryngeal mask airway. Nakayama M, Kataoka N, Usui y, et al: Techniques of nasotracheal intubation with the fiberoptic bronchoscope. Shigematsu T, Miyazawa N, Kobayashi M, et al: Nasal intubation with Bullard laryngoscope: a useful method for difficult airways. Schwartz D, Singh J: Retrograde wire-guided direct laryngoscopy in a 1-month-old infant. Barriot P, Riou B: Retrograde technique for tracheal intubation in trauma sufferers. Afilalo M, Guttman A, Stern E, et al: Fiberoptic intubation in the emergency division: a case series. Chapman N: Gastric rupture and pneumoperitoneum attributable to oxygen insufflation by way of a fiberoptic bronchoscope. Ho C-M, yin I-W, Tsou K-F, et al: Gastric rupture after awake fibreoptic intubation in a patient with laryngeal carcinoma. Hata y, Sato F, Takagi K, et al: Transbronchoscopic Oxygen Insufflationinduced Barotrauma During Endobronchial Silicon Spigot Removal. Rudolph C, Schlender M: [Clinical experiences with fiber optic intubation with the Bonfils intubation fiberscope]. Agro F, Cataldo R, Carassiti M, et al: the seeing stylet: a model new gadget for tracheal intubation. Klein L, Paetow G, Kornas R, et al: Technique for Exchanging the King Laryngeal Tube for an Endotracheal Tube. A related method that has been described as delayed-sequence intubation has emerged in recent years. Both awake intubation and delayed-sequence intubation methods have their very own distinctive pharmacologic concerns. Clinicians must concentrate not solely on the manual abilities of airway management, but additionally on number of the appropriate medication to achieve particular objectives. These goals include: (1) immediate airway management, together with induction of unconsciousness and muscle paralysis; (2) analgesia and sedation in awake sufferers; (3) minimization of the opposed physiologic results of intubation, including systemic and intracranial hypertension; and (4) prevention of harm during the postintubation period, including inadequate sedation, hemodynamic instability, or oversedation. Consider awake strategies of intubation in high-risk sufferers with airways which might be anticipated to be tough. Assemble all necessary drugs and tools for oral intubation and the desired backup equipment for airway administration. The intent is to displace nitrogen from the lungs and exchange it with an oxygen reserve that may last a number of minutes. Under optimal circumstances, breathing one hundred pc oxygen for 3 minutes has been demonstrated to keep acceptable oxygen saturation for as a lot as 8 minutes in previously wholesome apneic individuals. After induction agents are given, this may be safely elevated to 15 L/min of oxygen. Pretreatment consists of the administration of medicines to mitigate the potential untoward responses to intubation. Oxygen will displace nitrogen from the lungs and supply an oxygen reserve that may last a number of minutes. After induction, administer a paralytic agent to achieve muscle rest, which tremendously facilitates intubation. Assess for enough tissue oxygenation and response to beforehand administered medicine. Prudent clinicians are conscious of the potential adverse results of intubation and are cognizant of potential methods to minimize them. Careful monitoring of the postintubation condition will guide specific interventions. Overzealous attempts to suppress the physiologic responses that normally accompany airway manipulation may be counterproductive. It could be fascinating to present airway management underneath the best of circumstances and with the least amount of damage to the affected person, however the best method to the physiologic responses to intubation is just unknown. It is crucial to forestall hypotension and hypoxia throughout intubation, significantly in those with neurologic injury. The following dialogue serves as a general medical guide to alterations within the physiologic response to intubation. Apply nasal cannula at excessive circulate presently if using nasal cannula for apneic oxygenation. Premedicate as acceptable: � Fentanyl:2to3�g/kg given at a rate of 1 to 2 �g/kg per min intravenously. Induce anesthesia with one of the following brokers administered intravenously: ketamine, etomidate, fentanyl, midazolam, or propofol. If unable to intubate in the course of the first 20-second try, stop and ventilate the patient with the bag-mask gadget for 30 to 60 seconds. The Pressor Response In addition to the ubiquitous sinus tachycardia, a variety of dysrhythmias have been reported after intubation. They are primarily ventricular in origin and embrace ectopic beats, bigeminy, and quick runs of ventricular tachycardia. No research have established a direct relationship between the response and subsequent clinical deterioration in a large patient population. It is also unclear whether or not attenuation of the pressor response prevents dysrhythmias or electrocardiographic proof of ischemia. Ideally, it might be desirable to avoid sudden increases in blood strain in unstable sufferers with acute cardiac or vascular disease. Lidocaine has been probably the most extensively evaluated, but it has not been proven to improve outcomes.
Discount 500 mg naproxen free shippingPathophysiology � Exact mechanism not understood, appears to be multifactorial with likely genetic element. Typically identified between age 2 and 4, when kids start to fall behind their friends in social and language growth. Meanwhile, on the severe finish of the spectrum, children may by no means develop speech and will display very ritualistic behaviour. Investigation and prognosis Hx � Parents, carers or lecturers could elevate concern about social behaviour. Typically development is grossly normal for the primary 12 months of life, after which there may be delay. Remember social and language expertise are on a spectrum Management Management is symptomatic and holistic. From twin research genetic element that seems to be associated to dopaminergic and noradrenergic neural pathways. Clinical options Symptoms � Inattention � Hyperactivity � Impulsiveness Signs � Concerns raised by faculty staff or dad and mom � Difficulty with education or faculty refusal Investigation and diagnosis Hx � Ask about delivery, prenatal historical past and household historical past. There is a big association with substance abuse, risk-taking behaviour and criminality in later life. Some are because of translocations and an even smaller number of cases are due to genetic mosaicism (some cells have two and a few three copies of the 21st chromosome). Epidemiology and danger components � 1:650 live births (all maternal ages) � Prevalence increases with maternal age 1:37 if mother >44 years old. Chorionic villus sampling (offered to all women at excessive danger of carrying a baby with Down syndrome). If both mother and father are carriers, the kid has a (i) 25% chance of getting the situation; (ii) 50% likelihood of being a carrier themselves; (iii) 25% likelihood of being an unaffected non-carrier. There could additionally be an abnormal variety of chromosomes (aneuploidy) or deletion of part of a chromosome. Condition Edwards syndrome Patau syndrome Turner syndrome Genetics/ incidence Trisomy 18. Microcephaly, small eyes, scalp defects, cleft lip/palate, cardiac defects, renal abnormalities, polydactyly, extreme developmental delay. Infertility, brief stature, main amenorrhoea, pubertal delay, webbed neck, low-set ears, normal intelligence, wide-spaced nipples, horseshoe kidney (50%), cardiac defects (especially coarctation of the aorta). Many of those children may have brief life expectancy and never have the flexibility to be impartial as they develop up; will want long-term support. Due to the subtleties of medication, these lists are crude, inexact and abbreviated. Prehospital very important signs should all the time be interpreted with the whole clinical state of affairs in perspective. Blood stress and pulse are incessantly evaluated collectively as a measure of blood volume. Capillary refill is discussed as an assessment of overall perfusion, circulatory volume, and blood stress. Although physique temperature is usually the last vital signal measured throughout resuscitation, it has special importance for patients suffering from thermal regulatory failure. With these concerns in thoughts, the present chapter is organized according to the priorities of affected person resuscitation and analysis. Assessment of pain as a vital signal is gaining acceptance and is mentioned briefly at the end of this chapter. Vital indicators may point out the severity of sickness and likewise dictate the urgency of intervention. Although a single set of abnormal values suggests pathology, findings on triage or the initial important signs could additionally be spurious and simply related to stress, nervousness, pain, or worry. The best utility of important signs is in their continued remark and trends over time. Deteriorating very important signs are an necessary indicator of a compromised physiologic condition, and improving values present reassurance that the affected person may be responding to therapy. The regular ranges for important signs are additionally influenced by gender, race, being pregnant, and residence in an industrialized nation. Values for pulse and respiration in youngsters older than 3 years mirror a mean of female and male values for 0- to 1-, 3-, 9-, and 16-year-old populations. The values for blood pressure mirror a median of female and male values for the 1- to 6-month-old and the 3-, 9-, and 16-year-old populations. The study of pulses was tremendously influenced by galen, who expanded the subject into a quite complicated and obscure artwork type and wrote 18 books on the topic. Although their routine use was supported by Boerhaave, thermometry was not established as routine clinical apply until the 1870s. Although systolic blood pressure increases with age, normotensive or normal systolic blood pressure is outlined as ninety to a hundred and forty mm hg, and normotensive or regular diastolic blood stress is defined as 60 to 90 mm hg. The current literature suggests defining an "optimum" blood pressure as 115/75 mm hg because values at or under this stage have been associated with minimal vascular mortality. The recent literature suggests redefining values representative of hypotension in the aged, particularly in the setting of trauma. Systolic blood stress readings starting from roughly 90 to a hundred and twenty mm hg have been associated with occult hypoperfusion and elevated mortality in geriatric trauma patients. More recent information point out that forty five beats/min and ninety five beats/min could higher define the center price limits of regular sinus rhythm in adults of all ages. Spodick and colleagues recommended that the operational definition for the bounds of the resting coronary heart fee in adults must be 50 beats/min and 90 beats/min. Pregnancy is characterised by important increases in minute air flow, and is believed to be as a end result of the mixed facilitatory effects of progesterone and estrogen on central and peripheral chemoreflex drives to breathe. The norms for systolic and diastolic blood strain are depending on patient positioning. When a pregnant affected person is sitting or standing, systolic pressure is essentially unchanged. When a pregnant affected person is within the lateral decubitus place, both systolic and diastolic strain decline until the twenty eighth week and then start to rise to nonpregnant ranges. The pattern, effort, and quantity of respiration could also be more indicative of altered respiratory physiology. Rates obtained by nurses versus medical college students diversified significantly, as did these obtained by medical college students versus residents and attending clinicians. Smoothed percentile curves demonstrated a bigger dispersion at delivery (5th percentile, 34 breaths/min; 95th percentile, 68 breaths/min), whereas dispersion was less at 36 months of age (5th percentile, 18 breaths/min; 95th percentile, 30 breaths/min). It is often tough to decide whether tachypnea is a primary discovering or is simply associated with hyperpyrexia. A research of youngsters younger than 2 years in whom pneumonia was subsequently diagnosed discovered that age-appropriate limits for resting tachypnea in the presence of fever might be defined. Respiratory Pattern and Amplitude hyperventilation and hypoventilation may result from an extensive number of issues and may be related to pulmonary a main complaint or a manifestation of other systemic ailments. The respiratory status of both adults and youngsters plays a vital position in figuring out the general evaluation of sickness. Abnormal respiratory patterns could be attribute of metabolic or central nervous system pathologic situations.
Naproxen 250 mg mastercardIf no fluid is aspirated, withdraw the needle completely and redirect it in a deeper posterior trajectory. Recommendations regarding needle trajectory vary extensively, together with toward the right shoulder, sternal notch, and left shoulder. Be aware that repositioning the patient alters the place of the center and pericardial sac inside the chest, so reassessment might be necessary. Prepare the skin antiseptically and place a sterile cowl over the ultrasound probe. If time permits, anesthetize the selected area with 1% lidocaine, with the superior border of the adjacent rib being used as a landmark. Ideally, the needle should have a sheath that allows it to be withdrawn after the pericardial house is entered. Attach a saline-filled syringe to the needle, and gently aspirate whereas slowly advancing the needle. Keep the ultrasound probe on the chest wall, instantly adjacent to the aspiration website. If the contrast materials clears instantly after administration (as occurs with agitated saline) or persists quickly inside the cardiac chambers, an intracardiac location is suggested. Fluid Aspiration and Evaluation A Removal of even a small amount of pericardial fluid. After any approach used for pericardiocentesis, place a quick lived drain not only to ensure rapid entry into the pericardial sac but also to permit extra fluid to be eliminated shortly if hemodynamic collapse recurs. After needle placement is confirmed, a brief drain can be placed by the Seldinger technique, described in Chapter 22. Remove the syringe from the needle, advance a guidewire through the needle, and then take away the needle. Remove the dilator and slide an introducer sheath dilator (6 to 8 Fr Cordis) over the wire. Insert the pigtail angiocatheter via the introducer sheath, and aspirate fluid to verify placement. Attach the catheter to a three-way stopcock and connect it to a water seal to drain by gravity. The pigtail catheter allows extended drainage and safe access into the pericardial sac with out requiring the introduction of another needle. Blood retrieved from the ventricle often clots faster than bloody fluid aspirated from the pericardium. In basic, hemorrhagic pericardial effusions have local fibrinolytic activity, which prevents clot formation. The hematocrit of pericardial fluid ought to all the time be decrease than that of a pattern from the systemic vascular system, except in patients with aortic dissection or acute myocardial rupture. These circumstances aside, a hematocrit worth similar to that for systemic blood ought to elevate concern for an intracardiac needle location. Several other easy laboratory exams can differentiate regular from abnormal pericardial fluid, however they require the availability of a centrifuge system and time. Immediately following the procedure, obtain a chest movie to ensure the absence of pneumothorax and free air underneath the diaphragm. C, the shaft of the pigtail catheter (arrowhead, two discrete parallel echogenic lines mirror the catheter partitions; the echo-free area represents the catheter lumen) lying in the pericardial area after nearly all of fluid has been drained. Prepare a saline echocardiographic contrast medium through the use of two 5-mL syringes, one with saline and the opposite with air. Monitor the entrance of the agitated saline into the pericardial area sonographically- it appears as a brightly echogenic stream. Suture the pigtail catheter to the pores and skin, however be careful not to occlude the catheter by tying it too tightly. It is critical for the emergency doctor to concentrate on each the traditional and modern strategies of performing the procedure and the complications that can be related to these strategies (see Review Box sixteen. Complication rates as little as 4% have been reported in giant observational research. Earlier studies of blind pericardiocentesis documented morbidity rates of 20% to 40% and mortality rates as excessive as 6%. Cardiac arrest and demise are hardly ever related to echocardiographically guided pericardiocentesis. When blind or electrocardiographically guided pericardiocentesis is carried out, the patient is normally already in full arrest and attributing the cause for death to the process is sort of unimaginable. In a sequence of 52 sufferers the only death occurred in a patient in cardiogenic shock in whom pericardiocentesis was nonproductive and who was found to have extreme arteriosclerotic heart disease, not tamponade, on postmortem examination. The two deaths occurred during or after the process, but whether they might be attributed to the procedure is unclear. One affected person with aortic rupture that penetrated into the pericardial space died of cardiac arrest instantly after the puncture. One of the most frequent problems is a dry tap, particularly when a blind method is used. A dry tap is often brought on by blockage of the needle with clotted blood or a pores and skin plug. With the parasternal strategy, the needle can turn out to be blocked by vigorous probing of the anterior costal cartilage. Preventricular contractions are incessantly noted after the needle enters the pericardial sac; nevertheless, no severe dysrhythmias leading to hemodynamic compromise have been talked about within the literature. A minor pneumopericardium is inconsequential; a larger assortment might cause tamponade. Maggiolini and colleagues reported transient third-degree coronary heart block in a single patient. Fortunately, inadvertent needle passage into the liver has not been reported to cause vital hemorrhage or death. There have additionally been infrequent stories of pneumopericardium after removing of a pericardiocentesis catheter. The explanation for the pneumopericardium is assumed to be the formation of a bronchopericardial fistula, however the precise mechanism is unclear. The mortality fee associated with tension pneumopericardium is roughly 50%, so think about pneumopericardium when sufferers complain of dyspnea and hypotension after removal of their catheter. These problems occur extra frequently during blind or electrocardiographically guided procedures. In patients taking anticoagulants, you will need to examine coagulation elements and monitor them closely after a seemingly insignificant pericardiocentesis as a result of hemopericardium might develop simply from the procedure itself. In the series compiled by Krikorian and Hancock,126 hemopericardium developed in 13 of 123 sufferers as a result of pericardiocentesis, one on account of a lacerated coronary artery. In their series of 352 procedures, duvernoy and associates168 reported 23 penetrations. Researchers differ in their opinions concerning the adverse results of ventricular puncture.
References - Skolarikos A, Griffiths TRL, Powell PH, et al: Cytologic analysis of ureteral washings is informative in patients with grade 2 upper tract TCC considering endoscopic treatment, Urology 61(6):1146n1150, 2003.
- Jensen MS, Toft G, Thulstrup AM, et al: Cryptorchidism concordance in monozygotic and dizygotic twin brothers, full brothers, and half-brothers, Fertil Steril 93:124n129, 2010.
- Cavallin M, Kamath PS, Merli M, et al: Terlipressin plus albumin versus midodrine and octreotide plus albumin in the treatment of hepatorenal syndrome: a randomized trial, Hepatology 62(2):567n574, 2015.
- Harold KL, Pollinger H, Matthews BD, et al: Comparison of ultrasonic energy, bipolar thermal energy, and vascular clips for the hemostasis of small-, medium-, and large-sized arteries, Surg Endosc 17:1228-1230, 2003.
- Hsieh TF, Yang YW, Lee SS, et al: Use of 5-alpha-reductase inhibitors did not increase the risk of cardiovascular diseases in patients with benign prostate hyperplasia: a five-year follow-up study, PLoS ONE 10(3):e0119694, 2015.
|
|