"Cheap digoxin 0.25mg online, hypertension 1."By: Dawn Sowards Brezina, MD - Assistant Professor of Medicine
 https://medicine.duke.edu/faculty/dawn-sowards-brezina-md
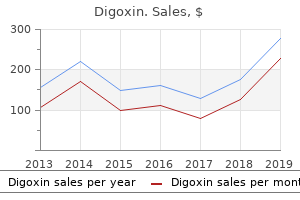
Purchase 0.25mg digoxin with mastercardThere are four "should know" questions in acute stroke triage that must be answered rapidly and accurately. Vascular Territory the vertebrobasilar system usually provides the entire posterior fossa constructions in addition to the midbrain, posterior thalami, occipital lobes, many of the inferior and posterolateral surfaces of the temporal lobe, and upper cervical spinal cord (8-27). In cerebral ischemia, the affected tissue stays viable although blood circulate is insufficient to sustain regular mobile perform. In cerebral infarction, frank cell dying occurs with lack of neurons, glia, or each. Hyperacute stroke designates events inside the first 6 hours following symptom onset. In hyperacute stroke, cell demise has not yet occurred, so the combined time period acute cerebral ischemia-infarction is usually used. Arterial Anatomy and Strokes Etiology Ischemic stroke is a heterogeneous disease with different etiologies and a number of other subtypes. Etiology varies with stroke subtype, and stroke subtypes additionally range by racial and ethnic teams. Intracranial atherosclerosis causes 30-50% of strokes in Asians but solely 8-10% in North America. Genome-wide analysis has also identified a robust overlap between large artery stroke and migraine headaches, particularly those without aura. Small artery occlusions, also known as lacunar infarcts, are outlined as lesions measuring lower than 15 mm in diameter. Most contain penetrating arteries in the basal ganglia/thalami, internal capsule, pons, and deep cerebral white matter. Common threat elements embody myocardial infarction, arrhythmia (most usually atrial fibrillation), and valvular heart illness. Other is a heterogeneous group that mixes strokes with miscellaneous however identified etiologies along with strokes of undetermined etiology ("cryptogenic stroke"). Oxygen is rapidly depleted, mobile vitality manufacturing fails, and ion homeostasis is lost. Neuronal dying with irreversible lack of operate happens in the core of an acute stroke. A relatively less ischemic penumbra surrounding the central core is present in about half of all patients. This ischemic but not-yet-doomed-to-infarct tissue represents physiologically "at risk" however doubtlessly salvageable tissue. There is a well-defined histologic "hierarchy of sensitivity" to ischemic damage among the many totally different cell varieties that represent the neuropil. They are adopted (in descending order of susceptibility) by astrocytes, oligodendroglia, microglia, and endothelial cells. There can be a geographic "hierarchy of sensitivity" to ischemic harm among the many neurons themselves. Hypertension, diabetes, smoking, metabolic syndrome, and elevated triglycerides are vital recognized predisposing elements. Acute infarcts could be solitary or a quantity of and range in size from tiny lacunar to large territorial lesions that can contain a lot of the cerebral hemisphere. An acutely thrombosed artery is crammed with delicate purplish clot that may contain the whole vessel or only a short phase (8-29A). Clot extension into secondary branches with or with out distal emboli into smaller, more peripheral vessels is frequent. Longer and bigger thrombi are additionally related to reduced likelihood of reperfusion after intravenous thrombolysis, so thrombectomy may be essential to maximize the chance and pace of recanalization. Gross parenchymal adjustments are minimal or absent within the first 6-8 hours, after which edema in the affected vascular territory causes the mind to appear pale and swollen. Frank cerebral infarction is characterised by irreversible harm to all cells within the infarcted zone. Within 12-24 hours, acutely ischemic neurons classically seem "red and dead" with hypereosinophilic cytoplasm, early karyolysis, and pyknotic nuclei. Acute infarcts are pale and sometimes vacuolized, especially close to the junction with intact mind. Stroke is the third main explanation for dying in lots of industrialized international locations and is the main worldwide reason for adult neurologic incapacity. Strokes have an result on sufferers of all ages-including newborns and neonates-although most occur in middle-aged or older adults. Children with strokes usually have an underlying disorder such as right-to-left cardiac shunt, sickle cell disease, or inherited hypercoagulable syndrome. Strokes in younger adults are sometimes attributable to dissection (spontaneous or traumatic) or drug abuse. Stroke symptoms differ widely, depending on the vascular territory affected in addition to the presence and adequacy of collateral circulate. Sudden onset of a focal neurologic deficit such as facial droop, slurred speech, paresis, or decreased consciousness is the most typical presentation. Between 20-25% of strokes are thought of "major" occlusions and cause 80% of opposed outcomes. Six months after stroke, 20-30% of all sufferers are dead, and an identical quantity are severely disabled. Nearly half of all strokes have insufficient collateral blood move and no vital penumbra. Most sufferers with main vessel occlusions-even those with a big ischemic penumbra-will do poorly until blood move can be restored and the brain reperfused. Stroke treatment choices and inclusion/exclusion standards are continually evolving. Acute ischemia is seen as delicate lack of gray-white interfaces and "blurred" basal ganglia. Endovascular thrombectomy benefits most patients with acute ischemic stroke attributable to occlusion of the proximal anterior circulation and offers an alternate, doubtlessly synergistic methodology to thrombolysis. Its advantages include delivering site-specific remedy and tailor-made thrombolytic dosage. Mechanical thrombectomy may also be appropriate in sufferers beyond the therapeutic window or in whom thrombolytic remedy is contraindicated. The main goals of emergent stroke imaging are (1) to distinguish "bland" or ischemic stroke from intracranial hemorrhage and (2) to select/triage patients for possible reperfusion therapies. Once intracranial hemorrhage is excluded, the second critical issue is determining whether or not a significant cerebral vessel is occluded. Nontraumatic Hemorrhage and Vascular Lesions 212 alternative for depicting probably treatable major vessel occlusions.
Buy 0.25mg digoxin free shippingAn appropriate pores and skin flap will end in excellent element of the sculpted cartilaginous framework. Most auricular deformities will have been present from start, however you will want to elicit any changes in growth of the ear or historical past of trauma to the auricle. Parents should be asked about how bothered the child is by the auricular deformity. The costochondral cartilage graft technique is a secure procedure as long as meticulous tissue handling is utilized and strict postoperative care is adopted. Careful dealing with of the cartilage and consciousness of the proximity of the pleura is essential. The synchondrosis between the sixth and seventh rib has been harvested along with the eighth rib cartilage. An x-ray movie template is useful each for marking the skin and for fashioning the cartilage framework. Has the kid had any previous makes an attempt at auricular surgery or has an auricular prosthetic ever been used Surgical repair is optimal in a recipient bed whose vascular supply has not been compromised by trauma, scarring, or previous surgical procedure. At the initial go to, cautious questioning concerning start historical past and neonatal exposure history might uncover potential causes of the microtia. Family historical past: Is there a family historical past of microtia, atresia, skin tags, cleft-craniofacial abnormalities, congenital cardiac abnormalities, kidney illness, or listening to loss If the time for surgical restore is close to, assess danger for bleeding or wound-healing difficulty by asking about: 1) Known bleeding disorders in the family 2) Antiplatelet medicine 3) Patient or family historical past of keloid formation 4) Herbal products 5) Smoking or smoke publicity 6) Nutritional status g. When contemplating a costochondral graft, you will need to ask about any known pulmonary illness, skeletal dysplasias, or rib anomalies. Facial symmetry � Especially in unilateral circumstances of microtia, the presence of facial asymmetry, hemipalatal paresis, or jaw discrepancy, may indicate a necessity for further assessment for hemifacial microsomia. If any vital crossbite or jaw asymmetry is famous, this will warrant orthodontic or oral surgical analysis previous to microtia restore, as the final word place of the reconstructed auricle could change with these interventions. Audiometric evaluation � Parents must be reminded that hearing is the first priority. Assessing listening to status on physical examination in an toddler or younger baby is unreliable. Anthropometric measurements-Having adequate costochondral graft materials for surgical restore of microtia relies upon the sufferers height and weight much more so than on age. An common 7-year-old may have an acceptable quantity of costochondral graft material. Assessing the place of the affected person on the expansion chart will aid in figuring out the proper timing of surgical procedure. If the patient is very excessive on the expansion curves, surgery may be thought-about at an earlier stage. An examination of the chest wall should reveal any skeletal abnormalities, including pectus excavatum, which can present a challenge for cartilage harvest.
[newline]Palpation of the decrease border of the ribs will reveal any contour irregularities which might be current. Examination of the auricle � Careful examination and documentation of the anatomy of the auricle is important. Examination of the preauricular space could reveal accessory tragi or sinus tracks that may be addressed before or throughout one of many phases of surgery. Otoscopic examination � Bilateral examination of the ear canals, if current, with an otoscope is crucial in assessing for aural atresia and external auditory canal stenosis. In unilateral instances, it is very necessary to document the examination of the tympanic membrane of the unaffected facet, as this can be the one listening to ear. Significant, uncorrected bleeding dysfunction or dietary deficiency that would increase the chance for complications with wound healing. Chest wall skeletal abnormalities, corresponding to significant scoliosis or pectus excavatum. An example of "closed framework" on the left (Bonilla); particulars of the cartilage are carved into the framework; tragus has been carved and might be connected to the primary framework prior to insertion. An instance of "open framework" on the right (Jabbour); antihelix is augmented with items of cartilage sutured to the primary framework. Typical examples of postoperative view immediately following stage I reconstruction (left) and 1-week postoperative (right). The movie then may be cut to develop a template which could be sterilized for use in the first stage of surgery. Patients should be endorsed on the importance of postoperative care and advised on practical surgical outcomes. Positioning Supine: the affected person is positioned supine so that both ears may be viewed and accessed during the process. Perioperative Antibiotic Prophylaxis First-generation cephalosporin Second-generation cephalosporin Clindamycin if allergic to penicillin. A pocket is created within the lobule to insert the inferior aspect of the cartilage framework. Excess pores and skin on the superior facet of the lobule is used to deepen the conchal bowl, and multiple smaller W-plasty incisions are carried out to irregularize the scar. Suture: 4-0 undyed nylon suture, 3-0 and 4-0 Vicryl suture, 5-0 monocryl suture, or related 4. Scarring Preoperative Preparation � Design of auricular template from flipped picture of contralateral auricle (if available). This can be carried out by printing a horizontally-flipped photo in picture modifying software program or by tracing the contralateral ear with transparency film. Rectus abdominus-inserts to cartilaginous parts of fifth, sixth, and seventh ribs and xyphoid course of. External stomach oblique muscles-origin is exterior surfaces of ribs 5 to 12; inserts to stomach aponeurosis. Internal stomach indirect muscles-has insertions into ribs eight to 12 and abdominal aponeurosis. Intercostal space-Neurovascular bundle runs within the superior aspect of each intercostal space in the order of vein, artery, nerve, from superior to inferior. Costochondral junction-The bony to cartilaginous junction of each rib can be recognized by the modifications in shade on the junction and confirmed with a 25-gage needle intraoperatively after exposing the rib, as the needle will pass extra easily into the cartilaginous portion. Surgical Technique There are two techniques: (1) three-stage Bonilla technique and (2) four-stage technique. Stage I-Creation and Insertion of Cartilage Framework and Tragus � Preoperative � Mark patient ear and rib to verify laterality in preoperative area. Have the nostril exposed, because the angle of the nasal dorsum parallels the best auricular angle. Skill and experience in carving costochondral cartilage for microtia reconstruction three.
Cheap digoxin 0.25mg onlineEtiology the main factors that decide whether a projectile will penetrate the skull are (1) its energy at influence on bone, (2) the contact area, and (3) the thickness of bone on the point of impression. Penetration by a ballistic projectile craters bone, punching it inward via the dura and into the mind. As a projectile penetrates the mind, it leaves a short lived cavity in Missile and Penetrating Injuries the extent of tissue harm from a projectile is decided by the kind of bullet, its velocity and mass, and the bodily characteristics of the affected tissues. Projectile (2-107) Autopsy specimen from a affected person with a gunshot wound from a 9-mm bullet reveals the typical findings of a relatively high-velocity projectile, specifically hemorrhage and disrupted macerated brain alongside the bullet path. It additionally causes outward radial stretching of adjacent tissue, depositing energy at very high pressure charges. This is why the entry wound is usually small and tissue injury expands because the bullet slows; the exit wound could also be very large. Projectiles with high kinetic energy could transfer enough vitality to the cranium to rework the bone fragments themselves into tiny secondary missiles. In the mixture, these fragments may be simply as deadly as through-and-through penetration by the projectile itself. Bullets passing via the firm brain tissue usually take a barely curved path between the entry point and ultimate location. The trajectory is marked by macerated tissue, torn vessels, and disrupted axons (2-107). Signs of brain swelling and herniation, together with apnea and bradycardia, are widespread. Mass of blood, imploded bone, and some bullet fragments are seen underneath the entrance wound. Enough kinetic power was current to punch the remaining fragments via the left squamous temporal bone, fracturing and exploding the skull outward. In common, a small-caliber, low-velocity projectile may have a comparatively small linear monitor through the brain (2-108). The bullet path is hyperdense and tends to curve slightly, broadening as the bullet yaws and slows. The exit wound is usually either a ledge-shaped fracture or "punched-out" bone (2-109). Injuries are most extreme with large-caliber missiles traveling at excessive velocity that fragment early on entry into the skull. Possible damage to crucial blood vessels ought to be noted together with secondary effects such as ischemia and herniation syndromes. A veritable "cascade" of antagonistic pathophysiologic occasions continues to develop after the initial injury. Some-such as progressive hemorrhagic injury-occur within the first 24 hours after trauma. These secondary results are sometimes extra devastating than the initial damage itself and may turn into life-threatening. Many doubtlessly severe secondary results are at least partially reversible if acknowledged early and handled promptly. Emergent imaging evaluation together with aggressive administration of elevated intracranial stress, perfusion alterations, and oxygenation deficits may assist mitigate each the quick and long-term results of mind trauma. In this article, we consider a broad spectrum of secondary effects that observe mind trauma, starting with herniation syndromes. They are the commonest secondary manifestation of any expanding intracranial mass, regardless of etiology. In this section, we briefly focus on the relevant anatomy and physiology that explain the pathology underlying brain herniations. We then delineate the spectrum of mind herniations and their imaging findings, beginning with the most typical types (subfalcine and descending transtentorial herniation). Posterior fossa herniations (ascending transtentorial and tonsillar herniations) are then thought of. We conclude the dialogue with a short consideration of uncommon however important kinds of herniations, corresponding to Trauma 66 (3-1) Falx cerebri divides the supratentorial compartment into 2 halves. Relevant Anatomy Bony ridges and dural folds divide the intracranial cavity into three compartments: two supratentorial hemicrania (the right and left halves) and the posterior fossa (3-1). The dura mater consists of two layers, an outer (periosteal) and an internal (meningeal) layer. The periosteal layer is tightly utilized to the inside surface of the calvaria, especially at suture strains. The meningeal layer folds inward to type two necessary fibrocollagenous sheets, the falx cerebri and tentorium cerebelli. The falx cerebri separates the proper and left hemispheres from each other, whereas the tentorium cerebelli separates the supratentorial from the infratentorial compartment. The concave inferior "free" margin of the falx incorporates the inferior sagittal sinus. As it courses posteriorly, the inferior margin of the falx forms a big open house above the corpus callosum and cingulate gyrus. This open area permits potential displacement of mind and blood vessels from one aspect towards the opposite. The opening is largest in the front and becomes progressively smaller, ending the place the falx joins the tentorium cerebelli at its apex. The tentorium cerebelli is a tent-shaped dural sheet that extends inferolaterally from its confluence with the falx, the place their two merging dural folds include the straight sinus. The tentorium is hooked up laterally to the petrous ridges, anteroinferiorly to the dorsum sellae, and posteriorly to the occipital bone. It has two concave medial edges that include a large U-shaped opening referred to as the tentorial incisura (3-2). Displacement of brain constructions and accompanying blood vessels from the supratentorial compartment or posterior fossa can occur in both direction-up or down-through the tentorial incisura. Parenchyma, cranial nerves, and/or blood vessels can become compressed towards the adjoining unyielding bone and dura. Secondary ischemic adjustments, frank brain infarcts, cranial neuropathies, and focal neurologic deficits may develop. If remedy is unavailable or unsuccessful, extreme neurologic injury and even dying is the results of what turns into, in essence, a brain "compartment syndrome. Herniation happens because the affected hemisphere pushes across the midline beneath the inferior "free" margin of the falx, extending into the contralateral hemicranium (3-3) (3-5). The ipsilateral ventricle appears compressed and displaced across the midline, while the contralateral ventricle (3-3) Autopsy exhibits subfalcine herniation. Left lateral ventricle is compressed, shifted throughout midline, as is cingulate gyrus. Right uncus and hippocampus are displaced medially and demonstrate "grooving" attributable to impaction against tentorial incisura.

Generic digoxin 0.25mg free shippingIn contrast to massive artery territorial strokes, embolic infarcts are likely to involve terminal cortical branches. Small peripheral foci of diffusion restriction in a number of totally different vascular distributions are typical of multiple embolic infarcts (8-52). The major differential diagnosis of multiple embolic infarcts is hypotensive cerebral infarction (see below). Hypotensive infarcts are usually attributable to hemodynamic compromise and tend to involve the deep internal watershed zones. Signs and symptoms vary in severity and embody petechial rash, headache, seizure, drowsiness, altered psychological status, and coma. Onset is from 2 hours as a lot as 2 days after trauma or surgery, with a mean of 29 hours. The main differential prognosis of cerebral fats embolism syndrome is a quantity of embolic infarcts. Lesions are inclined to involve the basal ganglia and corticomedullary junctions more than the white matter. Nontraumatic Hemorrhage and Vascular Lesions 226 Cerebral Gas Embolism Pathoetiology. Minor quantities of air in the intracranial venous systems is normally iatrogenic, introduced during intravenous catheter placement. Other etiologies of arterial or venous air embolism embrace lung biopsy, craniotomy in the sitting place, and angiography. Penetrating trauma, decompression illness, and hydrogen peroxide ingestion are other causes of fuel embolism. In more extreme instances, focal neurologic deficit, coma, seizures, and encephalopathy may ensue. Asymptomatic air following intravenous catheter placement is most commonly observed as an incidental finding, typically as dots of air within the cavernous sinus. If large air embolism occurs, cerebral ischemia or diffuse mind swelling typically ensues (8-56). Lacunar Infarcts Terminology the phrases "lacuna," "lacunar infarct," and "lacunar stroke" are sometimes used interchangeably. Lacunae are typically known as "silent" strokes, a misnomer as subtle neuropsychologic impairment is frequent in these patients. Lacunar stroke means a clinically evident stroke syndrome attributed to a small subcortical or brainstem lesion which will or is probably not evident on mind imaging. Lacunae are thought of macroscopic markers of cerebral small vessel ("microvascular") disease. There are two main vascular pathologies involving small penetrating arteries and arterioles: (1) thickening of the arterial media by lipohyalinosis, fibrinoid necrosis, and atherosclerosis causing luminal narrowing and (2) obstruction of penetrating arteries at their origin by giant intimal plaques within the parent arteries. Nontraumatic Hemorrhage and Vascular Lesions 228 pallidus, caudate nucleus), thalami, internal capsule, deep cerebral white matter, and pons. Grossly, lacunae appear as small, pale, irregular however relatively well-delineated cystic cavities (8-58). Microscopically, ischemic lacunar infarcts demonstrate tissue rarefaction with neuronal loss, peripheral macrophage infiltration, and gliosis. Clinical Issues Independent threat factors for lacunar infarcts embody age, hypertension, and diabetes. Between 20-30% of patients with lacunar stroke expertise neurologic deterioration hours and even days after the preliminary event. The pathophysiology of "progressive lacunar stroke" is incompletely understood, and no therapy has been proven to prevent or halt development. Cavitation and lesion shrinkage are seen in more than 95% of deep symptomatic lacunar infarcts on follow-up imaging. Embolic infarcts are typically peripheral (cortical/subcortical) quite than the standard central and deep location of typical lacunae. Watershed or "border zone" infarcts grossly resemble lacunar infarcts on imaging research. However, "border zone" infarcts happen in specific locations-along the cortical and subcortical white matter watershed zones-whereas lacunae are extra randomly scattered lesions that primarily have an result on the basal ganglia, thalami, and deep periventricular white matter. Anatomy of the Cerebral "Border Zones" Watershed zones are outlined because the "border" or junction the place two or extra main arterial territories meet. Etiology Two distinct hypotheses-hemodynamic compromise and microembolism-have been proposed because the etiology of hemispheric watershed infarcts. Terminal vascular distributions usually have decrease perfusion strain than main arterial trunks. Maximal vulnerability to hypoperfusion is biggest where two distal arterial fields meet collectively. Hypotension with or without extreme arterial stenosis or occlusion can lead to hemodynamic compromise. Anteriorly, they middle within the posterior frontal Arterial Anatomy and Strokes lobe close to the junction of the frontal sulcus with the precentral sulcus. Bilateral lesions are sometimes associated to world reduction in perfusion strain, often an acute hypotensive event. Confluent infarcts are large, cigar-shaped lesions that lie alongside or simply above the lateral ventricles. They resemble a line of beads extending from front to again within the deep white matter (8-63B). Nontraumatic Hemorrhage and Vascular Lesions 232 thalami, and pons and seem randomly scattered. Emboli are sometimes bilateral and multiterritorial however can also happen at vascular "border zones. Death or extreme lifelong neurologic deficits, including motor impairment, cognitive deficiency, and developmental delay, are widespread. This part will emphasize the position of ischemia and hypoxia in perinatal brain injury and acknowledge that inflammatory elements. Focal ischemia refers to decreased or absent perfusion in a specific vascular territory. Global ischemia happens when general cerebral perfusion drops beneath the extent required to preserve normal mind operate. From the middle of the third trimester of being pregnant via the 40th postconceptional week, the dorsal brainstem, thalami, basal ganglia, and perirolandic cortex exhibit excessive metabolic exercise. Damage is reflected in the interarterial (watershed) boundary or border zones and cerebral cortex (8-79A). In the 2nd trimester (gestational age of 14-26 weeks), ischemic injury results in liquefaction (8-80F); within the third trimester (27-40 weeks), ischemic damage leads to astrogliosis. Prolonged systemic hypoxemia leads to cardiac hypoxia, which in turn diminishes cardiac output.
Generic 0.25 mg digoxin overnight deliveryFor simple fractures, an arterial line is commonly not needed and transfusion is rare. However, for in depth facial fractures with many approaches, these monitoring strategies and blood products could additionally be helpful. Staged procedures can also enable for extra imaging and adjustments of the three-dimensional position of segments if in depth fractures are current. In the central region, the flap is superior anteriorly just superficial to the periosteum as much as the supraorbital ridge. Osteotomes can be used to mobilize the bone housing the supraorbital neurovascular bundle to acquire more flap mobility. If indifferent from their regular insertions, then a small fragment of bone can virtually at all times be recognized. Appropriate three-dimensional positioning of the zygoma, superior orbital rims, and nasal bones is important to providing the appropriate width, peak, and projection of the face. The positioning of the maxilla typically relies upon upon the place of the upper facial skeleton. Trans-nasal wiring secured to a contralateral plate is helpful in reaching correct dimensions. The arch is dissected out separately as needed, making the incision roughly 1 cm superior to the arch into the deep layer of the superficial fascia or adipose tissue pad. The skin could also be closed with staples, running 4-0 monofilament or 4-0 resorbable braided suture. Often, restricted approaches give a limited view of the adequacy of discount in three dimensions. After discount, if the defect is small and never in a important space where quantity loss can happen, then a reconstruction of the ground may not be needed. Critical areas where quantity loss may occur include the bulge within the flooring of the orbit and the medial bulge of the medial wall. D, A transcranial method was required via bicoronal incision and bifrontal craniotomy with removing of the posterior wall of the frontal sinus. E�J, Split-thickness cranial vault bone was used for reconstruction of the orbits and other areas. K, the affected person had a pre-existing malocclusion consisting of an open chew, which was recognized due to developmental mammelons on the incisors and a pre-injury plan for orthognathic surgical procedure. L�M, Despite an elevated intracranial pressure, the affected person recovered with the necessity for under minor nasal cartilage revision and rhinoplasty as a end result of lacerations associated with the nostril. A, A young male who sustained a left fist to the face leading to a fractured zygoma with medial displacement. B, the computed tomography scan reveals the standard displacement that requires three-dimensional repositioning through a number of incisions. Brow, intra-oral, and transconjunctival incisions are sometimes used to position and fixate fractures similar to these. Lower-lid approaches such as the deep fornix trans-conjunctival with or with out inferior lateral cantholysis, subcilliary, or lid crease incisions can be utilized depending upon the need for access, current lacerations, or preferences. Larger defects profit from extra assist with materials that retain a selected shape, such as porous polyethylene with imbedded mesh. These are greatest reconstructed with preformed or personalized reconstructive implants. Some surgeons place a small drain within the floor of the orbit to keep away from the formation of a hematoma. When lowering these fractures, you will want to mobilize them back to the right projection. Ifmultiple facial fractures have occurred and the maxilla is in several fragments, then the mandible is normally reconstructed to its authentic three-dimensional type. This permits for correct closure later and a great vascular pedicle to anterior maxillary segments. It is often useful to expose the anterior nasal ground and inside piriform rim to help align the segments for fixation. A, the basic clinical look of an emergent lure door fracture in a younger girl with entrapment. B, A coronal computed tomography scan shows entrapment of periorbita and inferior rectus. C, Navigation and mirroring technology can be utilized to assist place an orbital implant into a defect as quickly as the periorbita has been launched. The anterior and lateral views of the Le Fort midface fracture classification are proven highlighting the involvement of the various constructions of the midface. Custom splints could be made of acrylic using dental fashions, but they may additionally be fashioned quickly from perforated thermoplastic splint materials. As such, plating methods are sometimes used on the 4 anterior buttresses of the maxilla to provide fixation. Many surgeons use an outside-in method, by which the mandible and upper cranio-orbital skeleton are reconstructed previous to the maxilla when pan-facial fractures occur. Dissecting the coronal incision too superficial within the anterior area of the superficial temporal fascia layers might trigger frontal nerve branch weak spot. Dissecting the coronal incision too deep within the anterior area of the superficial temporal fascia layers into the muscle, inflicting muscle wasting and a lateral aesthetic defect within the temporal region. Complete reconstruction of the eyelid suspension system, leading to a rounded appearance to the eyelid 5. Incomplete repositioning of the canthi leading to traumatic telecanthus or poorly suspended eyelids 6. Failure to integrate dento-alveolar fracture treatment with the repositioning of the maxilla and/or mandible when reestablishing the occlusion 8. Failure to check with a dental specialist for dental accidents either during the preliminary reconstructive part or soon thereafter Common Errors in Technique 1. Drains are placed to bulb suction in the scalp and may be eliminated when fluid assortment has decreased markedly. In sufferers with solid fixation, gentle food could be launched within several weeks. Much of the information are self-reported and have inherent bias associated with the examine designs. That being mentioned, many surgeons quote an eyelid scarring complication rate such as ectropion, lid lag, or entropion at barely over 10%. Disruption of the orbital septum, orbicularis oculi, levators, or canthal system normally creates some lid contour irregularity. Postoperative nasal/oral bleeding may cease spontaneously if gentle or with oxymetazoline spray for nasal bleeding. Cerebrospinal fluid leak because of a persistent fistula or breach at the cranial base into the sinonasal area. Many small leaks can be repaired using an endoscopic method with or without navigation. Others could require an open strategy with pericranial flap placement or different techniques to block the leak. In some instances, a lumbar drain could be positioned to change differential strain for very small leaks.
Germanium Lactate Citrate (Germanium). Digoxin. - How does Germanium work?
- Arthritis, pain relief, osteoporosis (weak bones), low energy, AIDS, cancer, high blood pressure, high cholesterol, heart disease, glaucoma, cataracts, depression, liver problems, food allergies, yeast infections, ongoing viral infections, heavy metal poisoning, increasing circulation of blood to the brain, supporting the immune system, use as an antioxidant, or other uses.
- Dosing considerations for Germanium.
- Are there safety concerns?
- What is Germanium?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96468
Generic digoxin 0.25 mg with amexThere are few different areas of the body the place impaired nerve perform may be more devastating than within the head and neck. Peripheral cranial nerves contribute to our most personal attributes, corresponding to speech, facial expression, and the advanced neural coordination of deglutition. The technical elements of nerve restore have been refined; however, challenges persist in phrases of the practical outcomes. Any affected person undergoing head and neck surgical procedure faces dangers to multiple cranial nerves. Often in our subject, a nerve should be recognized and dissected for preservation or resected as part of an oncologic process. The lack of facial expression removes the visible thumbprint of our personalities in day-to-day interactions and could be devastating both emotionally and functionally. Patient expectations should be managed to put together for incomplete recovery, which might happen even with one of the best of reconstructive efforts. Past Medical History � H istory of diabetes mellitus and smoking could impair wound therapeutic. In this situation the affected person must be requested for consent to the use of acceptable donor websites for nerve graft harvest. As the seventh cranial nerve travels through the temporal bone, it develops more of a masking. This nerve sheath offers some safety with surgical manipulation, thus permitting the extratemporal nerve to be more resilient to extensive dissection. Surgical Technique Primary Neurorrhaphy the absolute best outcome after neural injury follows primary neurorrhaphy. Standard microsurgical techniques apply, and microscopic magnification should be used. Perioperative Antibiotic Prophylaxis Antibiotic prophylaxis must be given based on established pointers. In the case of a really clear process with no entry into the middle ear or oral cavity, weight-appropriate antistaphylococcal antibiotics ought to be given preoperatively and discontinued 24 hours postoperatively. Primary neurorrhaphy of a big buccal department of the facial nerve following trauma (left). This nerve might be positioned at the bisection of a line between the angle of the mandible and the mastoid tip. Notice its proximity to the external jugular vein (prominence seen at the inferior neck). Great auricular nerve cable interposition extending from the principle trunk of the facial nerve to the hypoglossal nerve. The nice auricular nerve seen operating anterosuperiorly on top of the sternocleidomastoid muscle (arrow). Other nerve graft choices in these areas embrace the lesser occipital and transverse cervical nerves. Consideration have to be given to using the contralateral great auricular nerve in the presence of malignancy, where perineural invasion might be present ipsilaterally. Skin incision marking for harvesting the medial antebrachial cutaneous nerve alongside the bicipital groove within the higher proper arm. Nerve hook underneath the medial antebrachial cutaneous nerve in the left higher arm. Note the distal branching and the basophilic vein and median nerve deep to the medial antebrachial cutaneous nerve. Sural Nerve Graft the sural nerve is frequently used for cranial nerve repair; its diameter is good for a wide range of repairs. Surgical Technique � The most direct method to harvesting this nerve makes use of a vertical incision operating from its location on the lateral malleolus and extending superiorly along the lateral leg for the length needed. Many strategies have been described, similar to segmental end-to-end neurorrhaphy extending from the donor nerves to the paretic nerve finish to side versus end-to-end coaptation. Positioning � A two-team strategy for sural nerve harvest and facial wound prep can be utilized. If90degreesisturned,thenthedonorleg must be away from anesthesia for ease of harvest. Technique � A facelift incision could be made using a #15 blade, and a pores and skin flap can be elevated over the parotideomasseteric fascia extending out to the anterior border of the parotid gland. Note extension into the hairline quite than utilization of the complete neck incision for this nerve transposition. Note: the babysitter nerve is defined within the part titled Cross-Facial Nerve Grafting. Right (donor) side of cross-facial nerve graft with three large buccal branches recognized at the anterior border of the parotid overlying the masseteric fascia (arrows). Infection is treated with culture-directed antibiotic remedy and incision and drainage if needed. This can be prevented through the use of good surgical method with consideration to detail and meticulous handling of the tissues and nerve endings. Becausetheinvolvedstructures are in the identical vicinity, one other nerve graft was unnecessary. If the primary reconstructive process occurred greater than 12 months earlier, a brand new muscle transfer ought to be carried out. All patients showed muscle contraction after 3 months and a smile with open mouth after 6 months. Symmetrical excursions of the oral commissure and a satisfactory social smile have been achieved; nonetheless, a spontaneous smile was not. Patients, significantly girls, must be suggested to use caution with blow dryers and curling irons. Fibrin glue versus microsurgical sutures in peripheral nerve repair: experimental and clinical study. Grafting of the Sural Nerve � I ntensification of diabetic neuropathy findings and pain might happen. Godin Prompt consideration to the ophthalmic manifestations of facial nerve paralysis is crucial to the care of affected patients. Loss of facial nerve function causes quite a few functional and beauty deficits within the periocular area. These embody poor eyelid closure with an increased palpebral fissure height, decrease eyelid ectropion inflicting restricted lacrimal pump perform, decreased meibomian gland perform and speedy evaporation of tears, decreased lacrimation from lack of parasympathetic tone, and descent of the forehead with secondary hooding of the visible axis. Greater degree and length of facial nerve dysfunction is an important danger factor for important ocular injury, however different features similar to concurrent trigeminal nerve involvement, poor Bell phenomenon, and elevated age or greater tissue laxity worsen the prognosis for the attention. The latter can be seen as a sort of tarsorrhaphy, with larger cosmesis and reversibility, with doubtlessly much less limitation of peripheral imaginative and prescient.
Generic digoxin 0.25 mg visaSignal depth decreases with time, reaching isointensity at 1-2 weeks (the T2 "fogging effect") (8-47). Nontraumatic Hemorrhage and Vascular Lesions 222 can sometimes be recognized as a well-delineated hyperintense band that extends inferiorly from the infarcted cortex along the corticospinal tract. The intravascular enhancement usually seen within the first forty eight hours following thromboembolic occlusion disappears within 3 or 4 days and is changed by leptomeningeal enhancement brought on by persisting pial collateral blood flow. Patchy or gyriform parenchymal enhancement can occur as early as 2 or 3 days after infarction (8-46) and will persist for 2-3 months, in some instances mimicking neoplasm (8-48). Arterial Anatomy and Strokes Chronic Cerebral Infarcts Terminology Chronic cerebral infarcts are the tip results of ischemic territorial strokes and are additionally called postinfarction encephalomalacia. A cavitated, encephalomalacic mind with strands of residual glial tissue and traversing blood vessels is the usual gross look of an old infarct (8-49A). The adjoining sulci and ipsilateral ventricle enlarge secondary to volume loss within the affected hemisphere (849A). Look for atrophy of the contralateral cerebellum secondary to crossed cerebellar diaschisis. Multiple Embolic Infarcts Brain emboli are less widespread however important causes of stroke. Simultaneous small acute infarcts in multiple completely different vascular distributions are the hallmark of embolic cerebral infarcts (8-51). Echocardiography could reveal valvular vegetations, intracardiac filling defect, or atrial or ventricular septal defect. Ipsilateral hemispheric emboli are mostly because of atheromatous internal carotid artery plaques. Focal hemorrhage is demonstrated on the caudothalamic groove, which represents the situation of the best aggregation of germinal matrix tissue. Linear accumulations of intraventricular hemorrhage are demonstrated throughout the frontal horns. Arterial Anatomy and Strokes 235 (8-70A) Coronal autopsy specimen reveals expansile clot throughout the left lateral ventricle. Note the bihemispheric hypointense halos, representing neurons migrating outward from the germinal matrix. During the period of early restoration (6-18 hours after insult), lactate and diffusivity abnormalities could transiently "normalize," solely to revert to abnormality after 24 hours. This just so happens to complement the present mind cooling protocols that usually conclude on day four. Normally, blood vessels of the brain constrict when blood stress will increase and dilate when blood pressure decreases. In the term newborn, hypoxia and hypercarbia lead to the loss of cerebral vascular autoregulation. Physiologic monitoring is required, and sedation is commonly wanted to control movement. Cranial sonography is nicely fitted to germinal matrix and intraventricular hemorrhage detection, and follow-up, is low value, requires no sedation, is portable to the bedside, and uses no ionizing radiation (8-67A). As an example, maternal chorioamnionitis leading to preterm delivery at 30 weeks (third trimester of pregnancy) with the next discovery of periventricular white matter harm probably represents a perinatal harm, not essentially a neonatal harm. This nuance of understanding has practical implications for our neuroimaging reviews because of attainable obstetrical and fetal maternal drugs legal consequences. The perinatal time-frame is outlined because the interval beginning at 20-28 weeks of gestation previous to birth and increasing 14 weeks after birth. Note the absence of anticipated T1 shortening (myelination) inside the posterior limbs of inside capsule. Ca++, manganese, and lipids within injured tissue could contribute to T1 shortening. The spectrum of mind harm within the preterm and time period neonate is surprisingly broad with distinctive qualities and factors of overlap. The full appraisal of injury is dependent upon the timing of imaging and the imaging modality selected. Preterm newborns are born earlier than 37 weeks of gestation and usually weigh less than 1,500 g. For those who survive prematurity, 90% will manifest neurologic deficits, including cerebral palsy and cognitive, behavioral, and a focus deficit issues. The prevalence and severity of neurologic sequelae improve with the extremes of prematurity. Lateral ventricles are compressed, outstanding regular torcula because of surrounding edema. Diffusion restriction is inside the corticospinal tracts and superior cerebellar vermis. T2 prolongation is usually seen in affected areas in the first few days after injury, and T1 shortening may be detected after 3 to four days. Given the diffuse cerebral injury (neurons and axons) beyond simply white matter, a more accurate encompassing but less generally used description is encephalopathy of prematurity. Therefore, decrease extremity axons are more incessantly injured, often leading to the clinical presentation of spastic diplegia. In affected areas, the cortex practically touches the lateral ventricles, which are enlarged and have irregular ("scalloped") margins (8-77). Reduced cerebellar volume in preterm newborns is common and may mirror transsynaptic degeneration of cerebellar tracts and neurons ensuing from supratentorial brain damage and/or disturbed signaling between the overlying leptomeninges and the underlying growing cerebellum. Imaging findings of asphyxia in term infants vary with severity of insult, timing of imaging, and chosen modality. Other at-risk regions include subthalamic nuclei, corticospinal tracts, and lateral geniculate nuclei. Sensitivity is recognizably lacking; nevertheless, if abnormalities are observed inside the first 12 hours after birth [e. T1 shortening inside the posterolateral putamina greater than T1 shortening throughout the posterior limb of inner capsule is a poor prognosticator. The pathologic T1 shortening likely represents accumulating Ca++, released myelin lipids, and manganese within infarcted tissue. T2 hyperintensity begins within 24 hours and lasts for 3-4 days and then transitions to T2 hypointensity, which is seen by day 7 and persists for up to a month(s) (8-78). Diffusion abnormalities peak close to 5 days after which "pseudonormalize" by the end of the primary postnatal week. Arterial strokes are underestimated within the pediatric inhabitants and symbolize a big explanation for neurologic morbidity and mortality. Known threat contributors embody obstetrical elements, congenital coronary heart disease, anemia, thrombotic/coagulation issues, polycythemia, metabolic derangement. Focal venous infarctions are less frequent than arterial infarctions in the neonate. Suspect venous infarctions when unexpected intracranial hemorrhage is detected.
Purchase 0.25 mg digoxin fast deliveryApproaches to brow raise that avoid subcutaneous skin dissection ought to be chosen on this population. General well being concerns which will preclude anesthesia must be considered and investigated. Multiple straight and curved periosteal elevators with various tip configurations b. Specialized insulated curved endoscopic scissors and graspers to facilitate dissection and cautery d. Typical minor plastic instruments, retractors, and periosteal elevators are necessary for many other brow carry approaches. Medication restriction listing reviewed with the affected person 2 weeks previous to the process. Facility with endoscopic approach is important to perform the endoscopic method to brow carry. Improper airplane of dissection: the surgeon needs to understand exactly which airplane of dissection is necessary to obtain the specified outcomes as each brow raise approach requires distinctive and infrequently a number of ranges of dissection. Injury to the frontal department of the facial nerve: Depending on the strategy chosen, careful anatomical dissection and conservative use of cautery or traction in the region of the nerve path is warranted to assist keep away from harm and ensuing significant disfigurement. E Surgical Technique With the patient seated in an upright place, manual elevation of the brow is helpful to decide the extent of elevation essential for best results. Plucking of lateral caudal brow hair is a typical beauty apply to create the looks of lateral forehead elevation. Proper brow elevation often requires lifting of the lateral brow region adequate to elevate thick forehead skin to or above the superior orbital rim. In these sufferers with severely thinned lateral brow hair the resultant brow might look "overly raised" when forehead hair is used as the primary determinant of proper postop brow position. Identification and preoperative counseling of these sufferers are necessary to set expectations. The affected person could also be inspired to allow resumption of hair progress in the lateral brow postoperatively. The targets of any forehead raise method are to elevate the forehead place and to abrogate the miserable effect of the glabella musculature when possible. This illustration demonstrates the incision sites used in various brow raise approaches: (A) Direct forehead carry, (B) Midforehead brow lift, (C) Hairline incision brow lift, (D) Coronal incision forehead lift, (E) Endoscopic brow raise. It is less adequate in the remedy of glabella ptosis and lateral orbital hooding than different forehead carry options as the shorter horizontal length of the incision web site may restrict medial and lateral elevation potential. It is a good alternative for use in unilateral facial paralysis instances given its capability for important change in brow place using a unilateral well-concealed incision. After marking the incision web site with the affected person in the upright place, 1% lidocaine with 1:one hundred,000 epinephrine is injected to the operative space. Half-strength betadine resolution (betadine solution combined 50:50 with balanced salt solution) is used to sterilize the brow and eyelid area. A fusiform horizontal incision is created inside the upper row of hairs in the brow hairline taking care to bevel the incision within the path of the hair shafts. Cutting throughout upper brow hair shafts may lead to lack of hair near the incision. The most superior incision must be beveled to assist create an everted skin closure. The horizontal length of the incision ought to be restricted and not extend previous the superior brow hair-bearing margin. Superior edge subcutaneous dissection could be performed to enhance forehead rhytids in this area. Detachment of the affected pores and skin from the forces exerted by deeper brow muscle exercise will allow enchancment in static rhytids. Medial sub-orbicularis muscle dissection might enable for sectioning of glabellar muscles if essential. After hemostasis is achieved with bipolar cautery, ptotic orbicularis and frontalis muscle may be sutured to the periosteum of the lower brow using multiple well-positioned 4-0 prolene easy stitches to obtain adequate correction of lateral, central, and medial forehead ptosis. Midforehead Brow Lift this strategy to forehead carry could be effective in men with unpredictable hairlines. The resulting scar is especially nicely hid when the technique is utilized in sufferers with deeper preexisting static brow rhytids. After marking the incision site with the patient within the upright position, 1% lidocaine with 1:100,000 epinephrine is injected to the incision site and supraorbital rim space. A fusiform horizontal incision is created in the midforehead taking care to bevel the incision to permit for eversion of the skin edges on closure. The contralateral brow raise incision website ought to be deliberate in an uneven trend with each incision web site centered on a horizontal rhytid of varying vertical position. The horizontal size of the incision could be prolonged to overlap at different heights medially for correction of medial forehead/ glabella ptosis and should lengthen laterally previous the lateral fringe of the frontalis muscle. Limited subcutaneous superior dissection is performed to permit some eversion of this pores and skin margin upon closure. The inferior subcutaneous undermining could also be carried inferiorly more extensively within the airplane just above the frontalis muscle to the level of the forehead if needed. Great care have to be taken in lateral dissection to keep away from injury to the frontal branch of the facial nerve and in medial dissection to avoid the supraorbital neurovascular bundle. The quantity of skin eliminated is predicated on the raise required and takes some experience to choose adequately. Fixation is achieved utilizing 4-0 prolene to secure the soft tissues of the forehead and orbicularis to superior periosteum. Sharp dissection close to the midline allows transition to a deeper subperiosteal aircraft of dissection giving access to the glabella musculature. Surgical sectioning of the corrugator and procerus muscular tissues, if deemed needed, is feasible using this method. Medial publicity and dissection from the above approaches are facilitated anteriorly and inferiorly in the subgaleal plane to a degree approximately 3 cm above the forehead. Sharp dissection to the subperiosteal aircraft is performed from this level inferiorly to the nasal bones taking care to protect the supraorbital and supratrochlear neurovascular bundles. The lateral incisions of each approach extend to the temple hair where dissection is carried all the means down to the superficial layer of the deep temporal fascia. Anterior dissection and publicity to the orbital rim is carried out within the layer between this fascia and the temporoparietal fascia that contains the frontal branch of the facial nerve. The arcus marginalis is launched on the stage of the orbital rim permitting mobilization of the lateral forehead. In either technique, an sufficient quantity of pores and skin is excised anterior to the incision and multilayer wound closure facilitates enough rigidity for brow fixation. Some surgeons suggest using tissue adhesives or bone-anchoring strategies for adjunct brow help through the therapeutic phase. For closure of the coronal incision wound, subcutaneous 4-0 vicryl deep sutures and superficial staples are used.
References - Uetani N, Bouchard M: Plumbing in the embryo: developmental defects of the urinary tracts, Clin Genet 75(4):307-317, 2009.
- Harmann P, Kron I, et al: Elevated intra-abdominal pressure and renal function, Ann Surg 196:594-597, 1982.
- Heinrich M, Oberbach A, Schlichting N, et al: Cytokine effects on gap junction communication and connexin expression in human bladder smooth muscle cells and suburothelial myofibroblasts, PLoS ONE 6(6):e20792, 2011.
|
|

