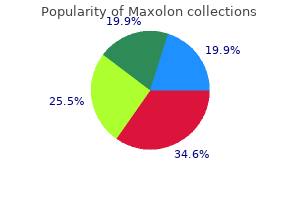
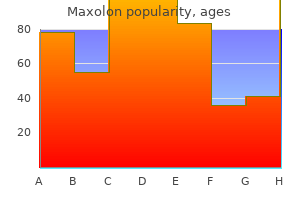
"Discount maxolon line, gastritis diet 13."By: Keira A Cohen, M.D. - Co-Director, The Johns Hopkins Center for Nontuberculous Mycobacteria and Bronchiectasis
- Assistant Professor of Medicine
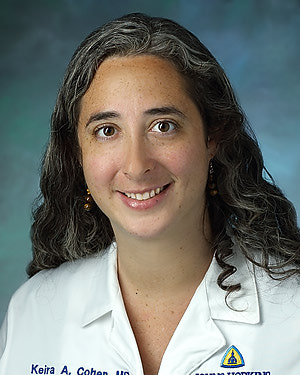 https://www.hopkinsmedicine.org/profiles/results/directory/profile/10003818/keira-cohen
Cheap 10mg maxolon amexThe proximal portion of the transverse mesocolon is termed the duodenocolic ligament. The left lateral continuation of the transverse mesocolon that fuses to the lateral parietal peritoneum is termed the phrenicocolic ligament. The identification of a mesentery or ligament may be made by the identification of its contained vessels or its location. The disease course of usually makes use of the vascular system as a scaffold as it spreads throughout the mesenteric planes. The lymphatic system, as nicely, resides throughout the subperitoneal area and is in continuity all through the stomach and pelvis. Lymphatic drainage from particular websites is exactly determined, and this is fundamental to the imaging of extension from quite lots of major origins, as will be discussed in later chapters. While the move inside the lymphatics occurs in a particular path, it may be altered by illness states. Hematogenous spread is by the arteries or veins, which course throughout the subperitoneal area as nicely as inside these vessels, as in extension of renal cell cancer within the renal veins and in malignant tumor emboli. This could occur with any illness course of and is between immediately adjoining organs. The mesentery is shaped by two visceral peritoneal layers linked to the parietal layer that forms the parietal peritoneum. Three of the 4 rows of diverticula face extraperitoneal tissues, whereas the antimesocolic row faces the peritoneal cavity. Direct or contiguous unfold of disease is between contiguous organs suspended in the peritoneal cavity or in the extraperitoneum and is throughout fascial planes. Tumor cells disseminate and deposit on the serosa of the bowel, the mesentery, and peritoneal lining of the peritoneal cavity, creating peritoneal carcinomatosis. The key observation on this technique of spread is the monitoring of the illness alongside the blood vessels throughout the ligaments, mesentery, and mesocolon. Subperitoneal Spread Along Mesenteric Planes the ligaments, mesenteries, and mesocolon develop from two peritoneal layers that include adipose tissue and cover the vessels, nerves, and lymphatics that provide the bowel and suspended organs. Disease processes similar to an infection, gasoline from bowel perforation, hematoma from bleeding, and tumors from the solid organs or bowel might unfold throughout the subperitoneal space and contain noncontiguous organs. This developmental and anatomic relationship types the conduit by which disease from the pancreas might spread to the hilum of the spleen by way of the splenorenal ligament along the splenic artery and vein, and to the larger curvature of the abdomen by way of the gastrosplenic ligament alongside the left gastroepiploic vessels and the brief gastric vessels. Lymphoma of the sigmoid colon with tumor infiltration throughout the sigmoid mesocolon. This a part of the ventral mesogastrium later develops in to the gastrohepatic ligament and hepatoduodenal ligament, offering the potential pathway for disease to talk between these organs. The gastrohepatic ligament carries the best gastric and left gastric vessels alongside the lesser curvature of the stomach and the accent or changed left hepatic artery and aberrant left gastric vein in to the ligamentum venosum and the left hilar fissure of the liver, whereas the hepatoduodenal ligament carries the hepatic artery, portal vein, bile duct communicating the hilum of the liver to the duodenum and the top of the pancreas. The transverse mesocolon, the mesentery, the sigmoid mesocolon, and the mesorectum type the conduit by which disease from the small bowel and colon can forty six a four. Extension of inflammatory process from pancreatitis alongside the splenorenal ligament along with a pseudocyst within the gastrosplenic ligament spreading alongside the greater curvature of the stomach and the gastrocolic ligament. The outpouching of the dorsal mesogastrium between the spleen and the greater curvature of the abdomen leads to the event of the gastrocolic ligament and the omentum, which attaches the anterior wall of the transverse colon forming an ``apron' anterior to the bowel within the abdominal cavity. The gastrocolic ligament, also referred to as supracolic omentum, supplies the conduit for illness spread between the stomach and the transverse colon. Gastric lymphoma with subperitoneal spread alongside the gastrohepatic ligament in to the fissure of the ligamentum venosum (arrows). Note lymphomatous mass around the left kidney (K) and within the jejunal mesentery (J). The mesocolon between the hepatic flexure of the transverse colon and the second portion of the duodenum (D) is also known as the duodenocolic ligament. Metastatic melanoma to the adrenal glands and hemorrhage from the left adrenal mass extending by way of the extraperitoneum and in to the left transverse mesocolon. Note the hematoma dissecting in to the transverse mesocolon (arrows) that can be traced to the band of tissue medial to the left transverse colon in image (a). Lymphoma of the jejunum with perforation in to the mesentery tracking towards its root. Hematoma within the root of the mesentery caused by bleeding from the ileocolic artery. Hemorrhage from the ileocolic vessel dissects in to the foundation of the mesentery and the ascending mesocolon. Metastatic lobular carcinoma of the breast to the abdomen infiltrating in the gastrocolic ligament. Note the hyperdense gentle tissue infiltrate (arrowheads) along the greater curvature of the abdomen. Subperitoneal Spread by Transvenous Spread 55 Subperitoneal Spread by Lymphatics and Lymph Node Metastasis Lymph node metastasis is a common method of unfold for most malignant tumors. They are all located in the subperitoneal space inside the ligaments, mesentery, mesocolon, and extraperitoneum. The key to understanding the pathways of lymphatic drainage of each individual organ is to understand the ligamentous, mesenteric, and mesocolic attachments and the arterial supply and venous drainage of that organ. First, when the first web site of the tumor is thought, it permits precise identification of the expected websites of nodal metastases by following the arterial provide or venous drainage within the ligaments, mesentery, or mesocolon attached to that organ. Third, it additionally permits identification of the expected site of recurrent illness or nodal metastasis or the pattern of illness development after remedy by wanting at the nodal station beyond the treated web site. This mode of tumor spread can additionally be categorized as subperitoneal spread as a result of the artery and the nerve run within the subperitoneal area with the ligaments, mesentery, and mesocolon. However, periarterial and perineural invasion extending exterior the organs may have an impact on clinical administration in two main areas. For example, pancreatic tumor infiltrates alongside the inferior pancreaticoduodenal artery to involve the superior mesenteric artery, or alongside the gastroduodenal artery to the common hepatic artery, rendering the tumor unresectable or resectable with a optimistic margin. Second, perineural infiltration outdoors the organ extending to a serious nerve plexus such because the celiac plexus can produce a continual debilitating ache that is a presenting symptom and requires correct pain control. Infection from the gastrointestinal tract or air within the bowel wall, a consequence of ischemia, can also unfold by way of the splanchnic veins in to the liver. By following the ileocolic vessels to the root of the mesentery, the anticipated pathway of nodal metastases of carcinoma of the cecum can be recognized. The analysis of carcinoma of the esophagus would be troublesome to make based mostly on this finding alone. Recurrent illness after resection of a carcinoma of sigmoid colon with a fistula to the jejunum. It follows the anticipated path of lymphatic drainage from the sigmoid mesocolon to a node on the origin of the inferior mesenteric artery.
Buy 10 mg maxolon fast deliveryMay contain fluid attenuation regions as a result of necrosis or focal aneurysmal bone cyst part. Expansile, lytic lesion with thin sclerotic margins; may contain partially calcified matrix. Giant cell tumor In spine, peak incidence are second and third many years of life, with female preponderance. Chordoma appears as a damaging vertebral body mass with osseous erosion and enlargement, sparing posterior elements. A massive associated soft tissue mass of low attenuation with extension in to the perivertebral house will be the dominant finding. Extension alongside nerve roots and enlargement of neural foramina mimics peripheral nerve sheath tumors. Destructive lesion, extra permeative, less expansile with related soft tissue mass. When the tumor breaks out of the vertebral body in an anterior path, the prevertebral portion of the perivertebral house is concerned early with epidural extension occurring late. Early epidural involvement with average perivertebral space tumor is seen when the metastatic illness breaks out of the vertebral body in a posterior, epidural direction. Lytic, permeative bone destruction with enhancing, poorly defined delicate tissue mass, involving adjoining buildings (epidural, paraspinal muscles). They embody malignant fibrous histiocytoma, fibrosarcoma, synovial sarcoma, and rhabdomyosarcoma. Originates from the sacrum and coccyx region (50%), sphenooccipital area (35%), and backbone (15%), particularly C2�C5 and lumbar. Cervical backbone chordomas happen in 40- to 60-y-old sufferers (M:F 2:1) and current with gradual onset of neck ache, numbness, and motor weak spot. Ewing sarcoma, chondrosarcoma, and osteosarcoma originate occasionally in the cervical backbone. Lymphoma Both in Hodgkin disease and non�Hodgkin lymphoma, bone involvement is often secondary (hematogenous unfold, or invasion from adjoining delicate tissues and lymph nodes). Most common presenting symptom is pain, most commonly in sufferers between the ages of forty and 70 y. Ovoid or rounded, unilocular, low-density cyst (isodense to cerebrospinal fluid), nonenhancing with no discernible wall. If infected, peripheral wall is thicker and enhances, and the density of content will increase. Uni- or multiloculated, nonenhancing fluid-filled mass with imperceptible wall, which tends to invaginate between normal structures. Rapid enlargement of the lesion, areas of excessive attenuation values, and fluid�fluid ranges suggest prior hemorrhage. Second branchial cleft cysts can occur anywhere alongside the line from the tonsillar fossa to the supraclavicular region. Lymphatic malformation (cystic hygroma, lymphangioma) Lymphatic malformations characterize a spectrum of congenital low-flow vascular malformations, differentiated by measurement of dilated lymphatic channels. Sixty-five p.c are present at birth; 90% are clinically obvious by three y of age. External or blended laryngocele extending from laryngeal ventricle with lateral extensions by way of thyrohyoid membrane. It is usually unwell outlined, enhancing, and extending along fascial planes and in to subcutaneous tissues beneath thickened skin. Abscesses could appear as a poorly marginated soft tissue mass in the expanded anterior cervical space with single or multiloculated low-density middle, with or with out gas collections, and usually thick abscess wall. It might outcome from extension of cellulitis or abscess from adjoining areas or after direct penetrating trauma. Malignant neoplasms Contiguous tumor extension Obliteration of the fat of the anterior cervical house because of an infiltrating mass with its heart within the adjacent infrahyoidal cervical spaces. These malignant tumors break out of their house of origin and invade the anterior cervical house. Also seen are associated cellulitis with obliteration of adjoining fat planes, thickening of the left sternocleidomastoid muscle and platysma, and infiltration of the subcutaneous fats. Radial tears of the anulus fibrosus are often clinically important and are associated with disk herniations. The term disk herniation usually refers to extension of the nucleus pulposus via an annular tear beyond the margins of the adjacent vertebral body finish plates. Posterior and posterolateral herniations can cause compression of the thecal sac and contents, in addition to compression of epidural nerve roots in the lateral recesses or within the intervertebral foramina. Lateral and anterior disk herniations are much less common however could cause hematomas in adjoining buildings. Disk herniations that occur superiorly or inferiorly end in focal depressions of the vertebral cortical end plates. The distal end of the conus medullaris is normally located on the T12�L1 degree in adults. Lesions within the thecal sac are categorized as intradural intra- or extramedullary. The higher two cervical vertebrae have different configurations than the opposite vertebrae. The atlas (C1) has a horizontal ringlike configuration with lateral plenty that articulate with the occipital condyles superiorly and the superior aspects of C2 inferiorly. The dorsal margin of the higher dens is secured in place in relation to the anterior arch of C1 by the transverse ligament. Various anomalies happen on this region, such as atlanto-occipital assimilation, segmentation. The lower five cervical vertebral bodies have rectangular shapes with progressive enlargement inferiorly. Superior and lateral projections from the C3 to C7 cervical vertebral our bodies kind the uncovertebral joints. The transverse processes are located anterolateral to the vertebral bodies and include the foramina transversaria within which the vertebral arteries and veins are situated. The posterior elements include paired pedicles, articular pillars, laminae, and spinous processes. The 12 thoracic vertebral bodies and 5 lumbar vertebral our bodies progressively enhance in dimension caudally. The posterior components embody the pedicles, transverse processes, laminae, and spinous processes. The transverse processes of the thoracic vertebrae even have articulation sites for ribs.
Discount maxolon lineAdenomyosis is described as an enlarged, globular, "boggy" uterus on physical exam. They can originate from the cervix, uterus, or adnexa, or from other organ methods. The main diagnostic checks are: Physical examination, pelvic ultrasound, and a negative pregnancy take a look at. This affected person presents with symptoms common for a ruptured ovarian cyst, which can require surgical intervention. Just like the unique follicle, the ovarian cyst is granulosa cell lined and incorporates a transparent to yellow estrogen-rich fluid. The sonogram demonstrates echogenic fluid (F) within the cul-de-sac and a big cystic mass with internal echoes (arrows) within the left adnexa. This affected person was known to have pelvic inflammatory illness and was efficiently treated with antibiotics. The larger the scale, the more pain they cause and the upper the risk of ovarian torsion. Acute pelvic pain (ie, rebound and guarding) typically signifies rupture of the ovarian cyst. May show an ovarian cyst or fluid in the cul-de-sac, which is consistent with a ruptured cyst. If the cyst is unresolved after 2 months, laparotomy/laparoscopy is indicated to evaluate/rule out neoplasia/endometriosis. Large ovarian cysts (> 5 cm) increase the danger of ovarian torsion, which is a medical emergency. Lutein Cysts There are two forms of lutein cysts: corpus luteum cysts and theca lutein cysts. If this ruptures, the patient will present with acute lower-quadrant pain and vaginal bleeding and may develop indicators of shock and hemoperitoneum. Treat with broadspectrum antibiotics (includes coverage for gram positive, gram unfavorable, and anaerobic organisms). They are generally referred to as "chocolate cysts" as a outcome of the thick, brown, tarlike fluid that they comprise. Endometriosis is a situation during which endometrial glands and stroma occur outside the uterine cavity and are located on the ovary. Definitive diagnosis is made by laparoscopy and a biopsy containing hemosiderin laden macrophages. Conservative surgical procedure (ovarian cystectomy): Entire cyst (endometrioma) could be excised by laparoscopy of laparotomy. She is afebrile and on examination, her left ovary palpates to 5-cm with mild tenderness, and the best ovary is regular size and nontender. An ultrasound performed within the workplace reveals a 5-cm, left hypoechoic unilocular cyst containing calcifications and inner particles. The various tissue discovered within a teratoma is believed to develop from the genetic materials in a single oocyte. Oocytes that are able to develop in to teratomas bear an arrest in improvement after meiosis I. Cystic teratomas can have a consistency ranging from fully cystic to completely stable. A young woman with a dermoid cyst may be handled with a cystectomy and not an oophorectomy-and the ovary can be preserved. These tumors include serous, mucinous, endometrioid, clear cell, and transitional cell. Sex-cord stroma: these embrace granulosa cell, Sertoli cell, Sertoli-Leydig, and steroid. Germ cells: these embody teratoma, dysgerminoma, yolk-sac, and embryonal choriocarcinoma. Ultrasound is useful in distinguishing between masses which may be prone to be malignant and benign (see Table 23-1). Differential Diagnoses Complete surgical staging must be performed for all women with ovarian cancer. In a girl with early-stage ovarian most cancers an stomach hysterectomy with bilateral salpingo-oophorectomy, omentectomy, lymphadenectomy, and peritoneal washings would be performed. With more superior disease, aggressive elimination of all seen illness improves survival. Ovarian most cancers is among the few cancers during which "surgical debulking" even in the presence of distant metastasis is helpful. Pelvic Sonographic Findings Suggestive of Malignancy Solid component of mass, not hyperechoic, nodularity Multiloculated (fluid trapped in different compartments) Thick septations (thick partitions between compartments) Presence of ascites Peritoneal masses, matted bowels, enlarged nodes 265 Seventy-five percent of girls are recognized with advanced disease after regional or distant metastases have occurred. Differential Diagnoses Rarely do leiomyomas (fibroids) progress to malignancy (leiomyosarcoma). Leiomyomas are localized, benign, easy muscle tumors of the uterus, that are hormonally responsive. Subserosal fibroids, which turn out to be pedunculated, could present with acute ache and torsion. Cervical dysplasia describes abnormal cells of the cervix that might be precursors to most cancers. Papanicolaou (Pap) smears are carried out regularly to assess for cervical dysplasia. Infection can occur via contaminated intact pores and skin, mucous membranes, or bodily fluids from an infected companion. Cells are scraped from the ectocervix with a spatula, then from the endocervix using an endocervical brush. The cells are smeared on a glass slide, fixative spray is applied, and the cells are examined. New method: Cervix is scraped and swabbed as above, but the sample is positioned in liquid medium (thin prep). Routine annual screening Pap tests should start at age 21; girls between the ages of 21 and 29 ought to receive screening Pap tests every 2 yr. Two totally different systems exist that describe the attainable findings of a Pap smear: 1. A Pap smear ought to be carried out every 4�6 months after remedy for no less than 12 months. A procedure that makes use of staining and a low-magnification microscope, mounted on a stand, for the viewing of the cervix, vagina, and vulva. Provides illuminated, magnified view, which aids in identifying lesions and biopsying suspicious areas to acquire histologic diagnosis.
Order 10 mg maxolon overnight deliveryFive-letter pacemaker identification code First letter Chamber paced O = None A = Atrium V = Ventricle D = Dual (A and V) Second letter Chamber sensed O = None A = Atrium V = Ventricle D = Dual (A and V) Third letter Response to sensing O = None I = Inhibits pacing T = Triggers pacing D = Dual (I and T) Fourth letter Programmable functions O = None P = Simple programmable M = Multiprogrammable C = Communication R = Rate responsive Fifth letter Antitachycardia features O = None P = Antitachycardia pacing S = Shock D = Dual (P and S) Pacemaker phrases Pacemaker firing A pacemaker produces a programmed present (stimulus) at a set price to the myocardium. This energy travels from the pacemaker generator via the lead wires to the myocardial muscle. Basic pacemaker operation consists of a closed-loop circuit during which electrical present flows between two steel poles (one negative, the opposite positive). Unipolar pacing has one pole (electrode) inside the heart, with the other pole being the metallic case of the pulse generator. The circuit travels between the electrode on the distal tip of the pacing lead in touch with the myocar- dium (the negative pole) to the pacemaker generator situated in gentle tissue (the constructive pole). The current travels between the electrode on the distal tip of the pacing lead (negative pole) to the proximal electrode situated a quantity of millimeters above the distal tip (the constructive pole). Capture the time period capture refers to the profitable stimulation of the myocardium by a pacemaker stimulus, resulting in depolarization. Atrial depolarization from a pacing stimulus leads to a pacing spike followed by atrial exercise (P wave). Automatic interval (pacing interval) the automated interval refers to the center fee at which the pacemaker is set. This interval is measured from one pacing spike to the subsequent consecutive pacing spike. This known as the A-A interval, analogous to the P-P interval of intrinsic waveforms. This is identified as the V-V interval, analogous to the R-R interval of intrinsic waveforms. The pacing stimulus has no impact for the rationale that ventricle is already being depolarized. The fusion beat has traits of each pacemaker and patient forces, although one often dominates the Pacemaker rhythm Stimulation of the atria for one beat is identified as an atrial paced beat. The identical concepts apply to permanent pacemakers, however correction of malfunctions requires using a pacemaker programmer or an precise surgical procedure to reposition the pacing lead or exchange the generator. Disconnection in the system - Check the connections between the generator, bridging cable, and lead; reconnect or tighten connections. Fracture of lead or lead insulation - Do an overpenetrated chest X-ray to detect fractures; have the doctor exchange the lead. Most malfunctions could be traced to problems with the generator (parameter settings, battery failure), the lead (problems on the interface between the catheter tip and the endocardium, fracture within the lead or its insulating surface), or to a disconnection within the system. This part features a description of pacemaker malfunctions, frequent causes, and interventions. Pacemaker is turned off - Make certain the pacemaker is turned on; the generator must be secured away from the affected person. Over a period of days, inflammation or fibrin formation on the catheter tip might raise the stimulation threshold, requiring a better mA output. Lead is out of place or lying in infarcted tissue - the electrode tip should be in contact with the endocardium for the electrical stimulus to cause depolarization. If the catheter is out of place, a brief maneuver is to flip the patient on his left side (gravity might permit the catheter to contact the endocardium). Electrolyte imbalance - Electrolyte imbalances can alter the flexibility of the heart to reply to a pacing stimulus. Analyzing pacemaker strips (ventricular demand type) 267 Causes and interventions for undersensing 1. Sensitivity set too low - Increase sensitivity by turning sensitivity dial clockwise to a decrease quantity. Pacing catheter out of place or lying in infarcted tissue - the electrode tip must keep up a correspondence with the endocardium to sense appropriately. If the catheter is out of place, a brief maneuver is to turn the affected person on his left facet, which can permit migration of the catheter in to a better place. Pacemaker set on asynchronous (fixed rate) mode - With asynchronous pacing, the sensing circuit is off. Oversensing the pacemaker is too delicate ("sees" too much) and is sensing the mistaken indicators (large P waves, giant T waves, muscle movement), inflicting the pacemaker to fireplace later than it ought to. Sensitivity set too excessive - Decrease sensitivity by turning the sensitivity dial counterclockwise to higher quantity. The computerized interval measurement will help you in figuring out if the pacemaker fired on time, too early, too late, or under no circumstances. Step two - Starting on the left facet of the strip, analyze each pacing spike you see. Note: Using the automated interval marks on index card, place proper mark on spike of late paced beat. Interpretation: Ventricular paced rhythm with one intrinsic beat and one episode of failure to seize (abnormal pacemaker function). Note: #6 represents an undersensing downside with out seize, while #8 represents an undersensing downside with seize. Interpretation: Ventricular paced rhythm with one fusion beat, three intrinsic beats, and two episodes of undersensing (abnormal pacemaker function). Interpretation: Ventricular paced rhythm with one pseudofusion beat and two intrinsic beats (normal pacemaker function). Step three - Identify the pacing spike to be analyzed (only analyze one spike at a time). Using the marked index card, place the left mark on the spike of the paced beat or R wave of the native beat immediately preceding the pacing spike being analyzed. Analysis: Interpretation: 11 For arrhythmia strips Posttest Posttest: All rhythm groups Follow the 5 fundamental steps in analyzing a rhythm strip. For pacemaker strips Follow the four primary steps for analyzing pacemaker rhythm strips. Interpretation: Ventricular paced rhythm with one intrinsic beat (normal pacemaker function) Strip 10-2 Analysis: the first three beats are ventricular paced beats adopted by two intrinsic beats, a pacing spike that happens too early, an intrinsic beat, a fusion beat, and two ventricular paced beats. Interpretation: Ventricular paced rhythm with three intrinsic beats, one fusion beat, and one episode of undersensing (abnormal pacemaker function) Strip 10-3 Analysis: the first complicated is an intrinsic beat adopted by two ventricular paced beats, an intrinsic beat, and two ventricular paced beats. Interpretation: Ventricular paced rhythm with two intrinsic beats (normal pacemaker function) Strip 10-4 Analysis: the primary two complexes are ventricular paced adopted by a pacing spike with failure to seize, a ventricular paced beat, a pacing spike with failure to capture, an intrinsic beat, a ventricular paced beat, a pacing spike with failure to seize, and an intrinsic beat. Interpretation: Ventricular paced rhythm with two intrinsic beats and three episodes of failure to seize (abnormal pacemaker function) Strip 10-5 Analysis: No patient or paced beats are seen; pacing spikes are present that fail to seize the ventricles. Interpretation: Failure to seize within the presence of ventricular standstill Strip 10-6 Analysis: the primary five complexes are intrinsic beats adopted by two ventricular paced beats, two intrinsic beats, and one ventricular paced beat. Interpretation: Ventricular paced rhythm with seven intrinsic beats (normal pacemaker function) Strip 10-7 Analysis: the first advanced is an intrinsic beat adopted by a ventricular paced beat that occurs too early, two ventricular paced beats, a fusion beat, an intrinsic beat, a pacing spike that occurs too early, and three intrinsic beats.
Maxolon 10mg visaFurthermore, pelvic illness, particularly involving the rectosigmoid, could spread cephalad in to the perirenal and pararenal compartments. Cysts may be solitary or a quantity of and are usually round and positioned in the cortex. Light gray area: anterior pararenal house; medium grey space: perirenal space; dark gray area: posterior pararenal house; short arrows: anterior renal fascia; lengthy arrows; posterior renal fascia; arrowhead: lateroconal fascia. Truly high-density cysts happen and are caused by proteinaceous material or "milk of calcium" within the cystic fluid, an infection, or hemorrhage in to the cyst. Thin intracystic septation occasionally happens in benign renal cysts, however other entities, such as multilocular renal nephromas, Wilms tumors, and abscesses, should be thought-about. The Bosniak classification is usually used to assess cystic renal lesions (Table 27. A renal mass of homogeneous density close to water displacing the left kidney anteriorly is seen on this nonenhanced scan. An isodense anterolateral enlargement of the left kidney containing a tiny calcification (arrow) is seen on this nonenhanced scan. In this place, the tiny calcification (arrow) is shifting to the most dependent portion of the kidney. A well-demarcated cyst without enhancement can be differentiated from the enhanced normal renal parenchyma. The tiny intracystic calcification is located at the most dependent portion of the renal cyst. Solid renal mass lesions are often irregularly shaped with poor demarcation from the traditional renal parenchyma. A strong renal mass lesion must be thought of malignant till proven otherwise and requires prompt scientific workup, including surgical exploration. The renal mass may be indeterminate for technical reasons, similar to respiration artifacts and volume-averaging effects. They correspond to types 3 and 4 in the Bosniak classification of cystic renal lesions and normally require prompt scientific workup, including percutaneous biopsy or surgical exploration. Calcifications in a focal renal lesion happen in each benign and malignant situations. A poorly defined lesion with less distinction enhancement than the adjoining normal renal parenchyma is seen within the lateral facet of the kidney. In addition to calcified renal cysts, aneurysms and arteriovenous malformation should be considered. In hydatid (echinococcal) disease, a bigger partially calcified cyst with a skinny or thick wall containing daughter cysts is diagnostic. Amorphous or punctate calcifications associated with a strong or partially cystic mass are found in a selection of benign. Diffuse renal parenchymal calcifications (nephrocalcinosis) happen most often in the renal medulla, particularly within the renal papilla, the place the biggest urine focus is attained. Medullary nephrocalcinosis is found with medullary sponge kidney, hyperoxaluria, and conditions related to hypercalcemia and hypercalcinuria. Cortical nephrocalcinosis is uncommon and limited to diseases primarily involving the renal cortex. Nonopaque calculi account for roughly 10% of all renal calculi and encompass uric acid, xanthine, or matrix (mucoprotein/mucopolysaccharide). Perinephric fluid collections complicating a renal transplant are attributable to lymphocele, urinoma, hematoma, and abscess formation. Lymphoceles are the commonest peritransplant fluid collections, characteristically occurring within 2 to 3 weeks after transplantation. A well-demarcated, hypodense lesion mimicking a cyst is clear within the lateral side of the left kidney on this contrast-enhanced scan. A massive fluid collection (arrow) is visible in the proper hemipelvis after renal transplantation. The density of the lymph within the lymphocele is similar to the urine within the adjacent distended bladder. Urinomas can occur at any time after transplantation and are brought on by an anastomotic leak or are secondary to a vascular harm causing a focal necrosis with subsequent leak in the urinary system. Nevertheless, a rapid improve within the dimension of a failing transplant suggests acute rejection. The differentiation of focal lesions in the kidney and perinephric space is mentioned in Tables 27. In horseshoe kidneys, the lower poles of each kidneys are fused by a parenchymal or fibrous isthmus across the midline at L4�L5 between the aorta and inferior mesenteric artery. The lengthy renal axis is medially oriented, and renal pelvises and ureters are situated anteriorly. Comments In longitudinal ectopy, the kidney is malpositioned in any location from the thorax to the sacrum. Pelvic kidney is the commonest location and frequently related to vesicoureteral reflux, hydronephrosis, hypospadia, and contralateral renal agenesis. In crossed ectopy, the malpositioned kidney is commonly fused with the contralateral kidney. A massive kidney with traditional outline and two collecting methods on one facet and an absent kidney on the contralateral side are diagnostic. In renal fusion, the fused kidneys are located in the midline and will assume the form of a horseshoe, disk, or pancake. Differential analysis: A malpositioned kidney may be brought on by a big adjacent mass. In full renal and ureteral duplication, the ureter draining the higher system inserts ectopically medial and below the orthotopic ureter in to the bladder trigonum or urethra and could additionally be associated with an ectopic ureterocele. Other congenital renal anomalies are partial duplication, supernumerary kidney, and renal hypoplasia or agenesis. Upper pole moiety is subject to obstruction and may simulate an higher pole mass on excretory urography when completely obstructed. The decrease poles of each kidneys are fused by a parenchymal isthmus, with the renal pelves and ureters being situated anteriorly. The right kidney is rotated and displaced medially by a big right retroperitoneal abscess containing an extended air�fluid degree. Differential diagnosis: renal duplication the place both the upper or lower pole moiety is malfunctioning. It might lead to concentric encroachment of the renal amassing system (trumpetlike pelvocaliceal system on urography), however with out obstruction. Dilated accumulating system evident as water-density structure within regular or enlarged kidney on nonenhanced photographs. After enhancement, a persistent nephrogram and delayed and decreased distinction medium excretion are characteristic. In long-standing obstruction, the kidney seems as a fluid-filled cyst with a thin rim of stable renal tissue draped around it. Comments Etiology: (1) regular improve of sinus fat with getting older and in obesity; (2) vicarious proliferation of sinus fat with renal atrophy of any trigger; (3) fibrolipomatosis induced by extravasation of urine in to the renal sinus. Early hydronephrosis could be differentiated from an extrarenal pelvis and postobstructive uropathy by the persistent nephrogram and delayed urinary distinction materials excretion after distinction enhancement.

Buy discount maxolon 10mg on lineParaseptal emphysema is proscribed in extent and often not associated with scientific illness, excluding a spontaneous pneumothorax. Irregular (paracicatricial or scar) emphysema is always related to localized. Clinical abnormalities in this type of emphysema are mainly associated to the underlying lung disease. Bullae are incessantly related to emphysema however may be found as a localized course of in otherwise regular lungs (primary bullous disease). A bulla is outlined as an air-filled thinwalled ("hairline") intrapulmonary cavity 1 cm in diameter. The pulmonary interstitium is the supporting construction of the lung and could be divided in to two compartments: (1) the central or axial interstitial space, consisting of the connective tissue surrounding main airways and pulmonary vessels, and (2) the peripheral interstitial space, together with the connective tissue of interlobular septa, as properly as across the centrilobular arterioles and bronchioles. From an anatomical point of view, any distinction between the central and peripheral interstitium is arbitrary. A key discovering of interstitial lung illness is thickening of interlobular septa (reticular thickening), primarily seen in the peripheral. Depending on the underlying illness, different typical findings embrace nodular and nonnodular thickening of interlobular septa, centrilobular nodules, and honeycombing. Nodular thickening of interlobular septa and peribronchial noduli are generally associated with interstitial ailments affecting the lymphatics, similar to metastatic spread. A bronchocentric sample impacts the acinus, including all constructions distal to the end-terminal bronchiole. It is initiated by way of inhalation of particles and subsequent mural infection/ inflammation. The peripheral V Thorax 596 16 Lungs a coexistence of pulmonary fibrosis and obstructive airway illness with cystic areas varying from 1 to 10 cm in diameter. Typically observed in sufferers with asbestosis, but additionally those with pulmonary fibrosis and lymphangitic carcinomatosis, are thin subpleural traces, 2 to 10 cm lengthy, paralleling the chest wall (curvilinear subpleural lines), in addition to nontapering bands of fibrous tissue radiating from the lung periphery. Irregular and serrated thickening of bronchi and vessels suggests fibrosis, whereas a clean thickening of these constructions favors edema and infiltrates. Besides these edematous and infectious processes, central interstitial thickening is associated with lymphangitic carcinomatosis, lymphoma, and sarcoidosis. In air-space (alveolar) disease, the air in peripheral airways is changed by fluid, cells, or stable substances, resulting in an increased regional lung density. The following conditions may be underlying causes: (1) low osmotic blood stress. With progression of the illness, these nodules coalesce and form bigger areas of consolidation, obscuring pulmonary vessels and causing characteristic air bronchograms. However, air bronchograms are also encountered in atelectasis and, hardly ever, in in depth interstitial illness, similar to sarcoidosis. Diffuse air-space disease tends to involve central portions of the lungs, whereas diffuse interstitial processes are predominantly observed within the lung periphery. Relatively excessive attenuation values are present in acute pulmonary hemorrhage and continual renal failure, probably due to dystrophic microcalcifications. Diffuse interstitial and/or micronodular densities with elevated attenuation are associated with mitral stenosis or different circumstances with chronically elevated left atrial pressure, as nicely as with healed disseminated infections, corresponding to tuberculosis, histoplasmosis and varicella pneumonitis, silicosis, radiopaque dust inhalation, amyloidosis, and alveolar microlithiasis. Thickening of the interlobular septa, which can be nodular (B); observe additionally the thickening of the centrilobular artery and bronchiole. Also evident are tubular bronchiectasis and the adjacent pulmonary arterial department cut perpendicular. Parenchymal bands or scars terminating in interlobular septa on the pleural floor (G). Expiratory scans show mosaic perfusion (thickening of paper-thin bronchioles resulting in regional air trapping). The lymphatics kind two pulmonary networks: a central network alongside arteries and airways right down to the respiratory bronchioles and a peripheral community alongside pulmonary veins, interlobular septa, and pleura. In the lymphatic pattern, centrilobular nodules 5 mm are found in a peribronchiolar, periseptal, and subpleural distribution. However, it could still be initiated by way of inhalation of particles; thus, differentiation between a bronchocentric and lymphatic sample often is troublesome. Uniform cystic areas ranging in diameter from 5 to 10 mm with thick partitions are attribute. Honeycombing is caused by a restricted variety of ailments, together with idiopathic pulmonary fibrosis, scleroderma, rheumatoid lung illness, eosinophilic granuloma, lymphangioleiomyomatosis, pneumoconiosis. It is particularly evident in each lower lobes apart from eosinophilic granuloma, sarcoidosis, and silicosis, which show upper zone predominance of honeycombing. These densities are noticed in circumstances in which either air within the acini is just partially replaced by delicate tissue-equivalent materials or the walls of the acini are diffusely thickened. This appearance is nonspecific and may be discovered with any early manifestation of a diffuse acinar or interstitial course of. Thus, ground-glass opacities could be caused by intra-alveolar fluid/inflammation, and simply characterize an alveolitis, or be affected by gentle thickening of the septal or alveolar interstitium. Ground-glass opacities are additionally often associated with a mosaic pattern, air trapping, "crazy paving," and fibrosis. A mosaic pattern merely describes regional variations in parenchymal density due to either air trapping or zones of elevated consolidation. Air trapping is extremely indicative of an airway disease and appears as normal parenchyma on inspiratory scans and low attenuating regions on expiratory scans. By distinction, zones of increased consolidation remain unaltered throughout expiratory scans. Crazy paving describes a sample by which thickened, polygonal interlobular septa are superimposed on ground-glass opacities. Differentiation between benign and malignant lesions stays a significant drawback, however. In case of sepsis or metastatic unfold, normally quite a few similar-sized pulmonary lesions are discovered. A vessel entering a small nodule is suggestive of a hematogenous metastasis, however it could also be related to septic emboli. A solitary pulmonary nodule may be assumed benign if it stays stable in volume over a 2-y interval. Benign calcifications (including histoplasmoma) are inclined to be either centrally situated or diffusely distributed throughout the lesion, whereas eccentric calcifications may also be found in malignant lesions. The demonstration of fat within the lesion normally suggests a benign hamartoma or, less generally, a lipomatous lesion, fat embolus, or lipoid pneumonia. Thus, any solitary nodule with smooth borders measuring 2 cm in diameter in an a-symptomatic affected person younger than forty y is prone to be benign and should be monitored. Additional findings embrace a notch in the mass, heterogeneity of the lesion, and a surrounding halo of lower density (hemorrhage/lymphangiosis).
Diseases - Chromosome 4, Trisomy 4p
- Ramer Ladda syndrome
- Focal dermal hypoplasia
- Schizophrenia, paranoid type
- Mucopolysaccharidosis type V
- Schizophrenia mental retardation deafness retinitis
- Pellagra
- AIDS dementia complex
- Candidiasis familial chronic
Cheap 10 mg maxolon fast deliveryEscape beats or rhythms - A time period used when the sinus node slows down or fails to initiate an impulse and a secondary pacemaker website assumes pacemaker control of the guts. Escape beats could come up from the atrium (atrial escape beat), the atrioventricular junction (junctional escape beat), or the ventricles (ventricular escape beat). Examples of escape rhythms are junctional escape rhythm and ventricular escape rhythm. Excitability - the power of a cardiac cell to reply to an electrical stimulus. The left main bundle department divides in to an anterior fascicle and a posterior fascicle, which form the two main divisions of the left bundle branch before it divides in to the Purkinje fibers. His-Purkinje system - the part of the electrical conduction system consisting 372 Glossary of the bundle of His, the bundle branches, and the Purkinje fibers. Hypertrophy - An increase in the thickness of a coronary heart chamber because of a continual increase in pressure and/or volume within the chamber. Infarction - Death (necrosis) of tissue caused by an interruption of blood supply to the affected tissue. Inferior vena cava - One of two massive veins that empty venous blood in to the proper atrium. Consists of three pathways of specialised conducting tissue positioned in the partitions of the best atrium. Ischemia - Reduced blood move to tissue attributable to narrowing or occlusion of the artery supplying blood to it. Contains the heart, trachea, esophagus, and great vessels (pulmonary arteries and veins, aorta, and the superior and inferior vena cava). Glossary 373 Overdrive pacing - Pacing the center at a fee sooner than the tachycardia to terminate the tachyarrhythmia. Papillary muscular tissues - Projections of myocardium arising from the walls of the ventricles related to fibrous cords called chordae tendineae, which are attached to the valve leaflets. During ventricular contraction the papillary muscle tissue contract and pull on the chordae tendineae, thus preventing inversion of the atrioventricular valve leaflets in to the atria. Stimulation of this technique decreases the guts fee, slows conduction by way of the atrioventricular node, decreases the force of ventricular contraction, and causes a drop in blood strain. Paroxysmal - A time period used to describe the sudden onset or cessation of an arrhythmia. Proarrhythmic - the impact of certain drugs (especially antiarrhythmics) to induce or worsen ventricular arrhythmias. Purkinje fibers - A community of fibers that carry electrical impulses on to ventricular muscle cells. Rate suppression - A lower within the heart rate for several cycles following a pause within the primary rhythm. Relative refractory period - the time frame during ventricular repolarization during which the ventricles can be stimulated to depolarize by an electrical impulse stronger than ordinary. Examples of reperfusion rhythms embrace sinus bradycardia, accelerated idioventricular rhythm, premature ventricular contractions, ventricular tachycardia, and ventricular fibrillation. Repolarization - An electrical course of by which a depolarized cell returns to its resting state (negative charge) as a outcome of the motion of ions across a cell membrane. Retrograde - Moving backward or in the reverse direction to that which is taken into account normal. Stimulation of the ventricle right now could precipitate repetitive ventricular contractions, resulting in ventricular tachycardia or fibrillation. Sick sinus syndrome - A degenerative illness of the sinus node leading to bradyarrhythmias alternating with tachyarrhythmias. This syndrome is commonly accompanied by symptoms such as dizziness, fainting, chest ache, dyspnea, and congestive coronary heart failure. Permanent pacemaker implantation is beneficial once the patient becomes symptomatic. Sinus arrest - An arrhythmia caused by a failure of the sinoatrial node to initiate an impulse (a dysfunction of automaticity). Sinus arrhythmia is a traditional phenomenon associated with the phases of respiration. Sinus exit block - An arrhythmia attributable to a block in the conduction of the electrical impulse from the sinoatrial node to the atria (a disorder of conduction). Sinus node - the dominant pacemaker of the center located within the wall of the right atrium close to the inlet of the superior vena cava. Superior vena cava - One of two large veins that vacant venous blood in to the best atrium. Supernormal interval - the last section of repolarization during which the cardiac cell could be stimulated to depolarize by a weaker than regular electrical stimulus. This interval happens near the tip of the T wave simply earlier than the cells have utterly repolarized. Supraventricular - A basic time period used to describe arrhythmias that originate in sites above the bundle branches. Glossary 375 Stimulation of this system increases coronary heart price, speeds conduction through the atrioventricular node, increases the drive of ventricular contraction, and causes an increase in blood strain. Electrical impulses are conducted from an exterior power source (pacing generator) through the lead wire to the best ventricle. Vagal maneuvers - Methods used to stimulate vagal (parasympathetic) tone in an try to sluggish the guts rate. Methods embody coughing, bearing down (Valsalva maneuver), squatting, breath-holding, carotid sinus strain, stimulation of the gag reflex, and immersion of the face in ice water. Valsalva maneuver - Forceful act of expiration with mouth and nose closed producing a "bearing down" action. Vasovagal reaction - An excessive body response that causes marked bradycardia (due to vagal stimulation) and marked hypotension (due to vasodilation). Ventricles - the two thick-walled decrease chambers of the center; they obtain blood from the atria and pump it in to the pulmonary and systemic circulation. Ventricular fibrillation - An arrhythmia arising from a disorganized, chaotic electrical focus in the ventricles during which the ventricles quiver instead of contracting successfully. Ventricular tachycardia - An arrhythmia arising from an ectopic web site within the ventricles. Vulnerable interval - the time period during ventricular repolarization by which the ventricles could be stimulated to depolarize by a strong electrical stimulus. This period corresponds to the down slope of the T wave (relative refractory period). Electrical stimuli occurring in the course of the weak interval could lead to ventricular tachycardia or ventricular fibrillation. Wandering atrial pacemaker - An arrhythmia arising from multiple pacemaker websites in the atria. The synovial membrane intima is only one or two cell layers thick and accommodates two major cell varieties: kind A synoviocytes, which bear macrophage markers, and type B synoviocytes, which have fibroblastic traits. The matrix of the intima is rich in proteoglycans and glycosaminoglycans, in particular hyaluronic acid.

Safe maxolon 10mgPolyp (adenomatous or hamartomatous) May be hereditary or nonhereditary, with or with out different associated lesions. Diagnostic pearls: Annular strong enhancing mass of soft tissue density discovered on the bowel wall. Large, well-defined, strongly enhancing inhomogeneous mass with or without necrosis and calcifications. Diagnostic pearls: Either diffuse bowel wall thickening or segmental annular mass with ulcerations with or without mesenteric lymphadenopathy. Single or multiple, sessile or pedunculated plenty of sentimental tissue density that enhance with distinction and should comprise ulcerations. Diagnostic pearls: Mesenteric mass of soft tissue density with spiculated margins; retraction of the bowel loops toward itself is attribute. Diagnostic pearls: Heterogeneous appearance-soft tissue nodules, scirrhous lesions, intramural deposits, or polypoid intraluminal masses. Greatest portion of metastatic deposits is normally situated in the mesentery adjoining to the wall of the small bowel. Diagnostic pearls: May be hypo- or hyperattenuating on postcontrast scans; calcified in 30% of cases. Leiomyosarcoma Approximately 50% of small bowel smooth muscle tumors are malignant. After liver metastasis, typical clinical indicators include flush, diarrhea, and cardia-related signs. Most common primary tumors embrace carcinomas of the lung, breast, colon, pancreas, kidney, uterus, and skin. Prognosis is determined by the completeness of surgical resection (5-y survival 15%�67%). Segmental annular lesion on the degree of the navel with mucosal ulceration (central hyperdensity) but without lymphadenopathy (a). Diffuse thickening of the horizontal portion of the duodenum related to cumbersome mesenteric and retroperitoneal lymphadenopathy (b). Small bowel metastasis of pancreas carcinoma (hypodense mural nodule) infiltrating the horizontal portion of the duodenum. Diagnostic pearls: "Whirl" signal: Small bowel loops and their mesenteric attachment converge centrally at the level of torsion. Diagnostic pearls: Cockade signal: Three concentric layers forming a gentle tissue mass (inner layer representing the lumen of the intussuscepted bowel; the middle layer, mesenteric fat; and the outer layer, the intussuscipiens). Mechanical obstruction of the small bowel through intraintestinal impaction of gallstones. One or a quantity of grossly distended, fluid-filled U-shaped loops with two adjacent limbs exhibiting a zone of abrupt transition. Strangulating obstruction: Slight circumferential wall thickening and enhancement (target sign) and engorgement of mesenteric vessels indicate mild ischemia. Increased bowel wall attenuation, mesenteric hemorrhage, and pneumatosis point out severe ischemia and infarction. Diagnostic pearls: Small bowel diverticula, segmental mural thickening, and luminal narrowing in combination with mesenteric stranding are extremely suspicious for small bowel diverticulitis. Always rule out inflammation, tumors (benign and malignant), and diverticula (Meckel diverticulum). Typical extrinsic causes are diverticulitis, appendicitis, hernias, adhesions, and peritoneal carcinomatosis. Volvulus with "whirl" signal due to twisting of the small bowel round its mesenteric axis (a). Another patient exhibiting a typical "coffee bean" sign of dilated small bowel loops (c). Axial scan reveals typical cockade sign up the right lower abdomen (arrow), as well as proximal bowel distention and distal "hungry" bowel loops (a). Dilated small bowel with no overlying omental fats displacing both hepatic flexures inferiorly and posteriorly and the principle mesenteric trunk to the proper. The proper hepatic flexure is stoolfilled; the left hepatic flexure distinction, media-filled. Diagnostic pearls: Markedly dilated small bowel loops and segmental wall thickening; clots in inside mammary artery and vein; three-layered appearance of bowel on postcontrast scans (target sign): low-attenuating edematous submucosa framed by hyperdense mucosa and serosa. Diagnostic pearls: Oval to spherical pericolonic fatty mass with hyperattenuating ring, surrounded by stranding of mesenteric fatty tissue. Precipitating elements embody bowel obstruction, vascular thrombosis, and recent surgical procedure. Ischemic colitis is a predominantly left-sided, segmental, or diffuse disease and will mimic pseudomembranous colitis. Prognosis is decided by the speed of therapy and the amount of small bowel affected. Diagnostic pearls: Inhomogeneous wall thickening of the cecum and ascending colon; often, spreading to the distal ileum and/or appendix. Clostridium difficile�induced acute inflammation of the colonic mucosa with or with out submucosa. Diagnostic pearls: Pancolitis with nodular circumferential wall thickening (15 mm). Histologically, an inflammatory means of the mucosa with deep ulcerations and necrosis because of native ischemia. Usually a complication of antibiotic remedy with copious nonbloody diarrhea, stomach cramps, and tenderness. Dilation of the descending colon and segmental wall thickening with "goal" sign (a). Restriction of adjustments to the left-sided colon is indicative of ischemic origin (b). Oval to spherical pericolonic fatty mass (arrow) within the left decrease stomach with hyperattenuating ring, surrounded by stranding of mesenteric fatty tissue. Pancolitis with nodular circumferential wall thickening ("accordion" sign) (a) and targetlike look of colonic wall (b). Diagnostic pearls: Actinomycosis: Predominantly in the ileocecal and rectosigmoid colon. Salmonellosis/yersiniosis: Predominantly ileum, but can also spread to cecum and proper colon. Schistosomiasis: Multiple polypoid filling defects in the sigmoid colon or rectum. Worm infestation (Ascaris and Trichuris): Bolus of ascariasis could cause a solitary filling defect. Trichuriasis may induce extreme mucus manufacturing and quite a few irregular filling defects.
Generic 10mg maxolon visaIf carcinoma, seek the guidance of gynecologic oncology to determine the best treatment (chemotherapy, radiation, or surgery). If ache persists, regardless of medical therapy, a surgical intervention may be thought of. The diagnosis and management for the ache is tailored to the organ system concerned. Pelvic ache accounts for 12% of hysterectomies, 20% of diagnostic laparoscopies, and 40% of repeat office visits. Symptoms cause vital misery or impairment in social, occupational, or different important areas of functioning (eg, missed work, homebound, depression, sexual dysfunction). Pain traits: Pain may be constant, intermittent, or with monthly menses (cyclic). Associated symptoms/relieving components: Pain may be associated with positional adjustments, fever, or nausea/vomiting. Adhesions are fibrous tissue that varieties between two inside organs and may be a source of ache. Social history (marital discourse, depression, stress, historical past of physical or sexual abuse): Pelvic ache has been identified to be associated with psychiatric factors and childhood sexual abuse. Physical examination: Look for: Masses on stomach and pelvic examination might suggest an enlarged ovary or a uterine fibroid. Bladder pain: May counsel interstitial cystitis; anterior vagina may be tender on palpation. Imaging research: Pelvic sonogram: Best to consider ovarian cyst/neoplasms or uterine fibroids. Referrals Gastroenterology referral for colonoscopy to evaluate for diverticulosis, irritable bowel syndrome, or inflammatory bowel disease. An ultrasound reveals a normal-size left ovary and a 4-cm proper ovary, with a small amount of fluid within the cul-de-sac (pouch of Douglas). Since she is hemodynamically secure, she ought to have a diagnostic laparoscopy to diagnose and treat, as a substitute of a laparotomy. Pelvic Pain An ovarian ruptured cyst is the most typical explanation for acute pelvic ache. History: Include temporal characteristics (cyclic, intermittent, or noncyclic), location, and severity of pain. Physical exam: Look for localized/point tenderness, cervical movement tenderness, adnexal tenderness, and stomach tenderness. Look for indicators of an acute stomach corresponding to guarding, rebound, or severe tenderness. Pelvic sonogram: Look for ovarian cysts/neoplasm, ovarian torsion, an intrauterine/ectopic pregnancy, uterine fibroids, or a tubo-ovarian abscess. She states that her menses started at age 13 and happens on common 28-day intervals. She complains of severe month-to-month pain 1 week earlier than each menses and ache with intercourse. On rectovaginal examination, she has uterosacral nodularity and a fixed, retroflexed uterus. What diagnostic take a look at can be essentially the most applicable at this point to make the prognosis Answer: the affected person has classical symptoms of endometriosis, particularly dysmenorrhea and dyspareunia. The tissue biopsy would present endometrial glands, stroma, and hemosiderin-laden macrophages. It responds to hormones and goes by way of cyclic modifications, similar to menstrual bleeding. The result of this ectopic tissue is "ectopic menses," which causes bleeding, peritoneal irritation, ache, fibrosis, and, finally, adhesions. Though the mechanisms and etiology are unknown, there are four theories commonly cited. It is likely that multiple theories could explain the diverse nature of this dysfunction: Retrograde menstruation: Endometrial tissue fragments are retrogradely transported via the fallopian tubes and implant there or intraabdominally with a predilection for the ovaries and pelvic peritoneum. Mesothelial (peritoneal) metaplasia: Under sure conditions, peritoneal tissue develops in to functional endometrial tissue, thus responding to hormones. Vascular/lymphatic transport: Endometrial tissue is transported by way of blood vessels and lymphatics. This can explain endometriosis in places exterior of the pelvis (ie, lymph nodes, pleural cavity, kidneys). Iatrogenic dissemination: Endometrial glands and stroma may be implanted during a procedure (eg, c-section). Adhesions trigger infertility, and small bowel obstruction, pelvic ache, and difficult surgeries. Endometriosis and Adenomyosis A girl with a first-degree relative affected with endometriosis has a 7% chance of being equally affected as in contrast with 1% in unrelated individuals. With a constructive family historical past, a patient might develop endometriosis at an earlier age than the member of the family. Dyspareunia (painful intercourse) because of implants on pouch of Douglas; occurs generally, with deep penetration. Congenital anomalies that promote retrograde menstruation could additionally be a common related finding in adolescents. Ovarian endometriomas: Tender, palpable, and freely cell implanted lots that happen throughout the ovarian capsule and bleed. This creates a small blood-filled cavity within the ovary, classically generally recognized as a "chocolate cyst. Laparoscopy or laparotomy: Ectopic tissue should be biopsied for definitive prognosis. The gold commonplace for prognosis is laparoscopy with biopsy proven hemosiderin laden macrophages. Tissue biopsy (cardinal features): Positive findings comprise endometrial glands, stroma, and hemosiderin-laden macrophages. Symptomatic patients may have increasing ache and potential bowel ache and potential bowel problems. The main goal is to induce amenorrhea and trigger regression of the endometriotic implants. Depo-Provera (progesterone [+/� estrogen]): Creates a pseudopregnancy (amenorrhea). Surgical Conservative (if reproductivity is to be preserved): Laparoscopic lysis and ablation of adhesions and implants. On physical examination, the uterus is 14 weeks in measurement, boggy, slightly tender, and cell.
Generic maxolon 10mg without prescriptionThere is a further lateral extraconal mass involving the left lacrimal gland (G). Layering hyperdense fluid-fluid levels correspond to blood merchandise from spontaneous hemorrhage. Comments Congenital hamartomatous lymphatic and venous vascular malformation; orbital lymphangiomas are inclined to populate the extraconal space but are sometimes transspatial. Lymphangiomas progressively and progresssively enlarge in the course of the rising years (do not involute). Orbital lymphatic-venous malformations occur in youngsters and younger adults, with slight feminine predominance. Most frequent clinical signal is progressive, painless proptosis with intermittent worsening. Rarely, one might even see a rim enhancement in this location or a small assortment of fuel. Demineralization, thinning, or lack of bone manifests inflammation or localized osteomyelitis of the adjoining bone. Cellulitic modifications with stranding and streaking of the intraconal fats, enhancing and swollen extraocular muscles, or solid enhancing phlegmon retrobulbar may precede or follow abscess formation. Progression might result in intraorbital abscess, superior ophthalmic vein thrombosis, cavernous sinus thrombosis, and intracranial extension. Accumulation of pus between (usually medial) orbital wall and orbital periosteum, secondary to acute sinusitis and phlebitic transmission, or direct extension through dehiscence within the adjoining orbital bone (lamina papyracea). Patients present with edema of the lids, painful proptosis, chemosis, eye muscle paralysis, visual disturbance, sinusitis, upper respiratory an infection, and headache, fever, and chills. Benign neoplasms Meningioma Sphenoid wing meningioma is the most typical meningioma in the extraconal space. A barely hyperdense mass, with or with out calcifications, and intense and uniform contrast enhancement is seen with sclerotic or lytic involvement of the adjoining orbital bone. Extraconal meningiomas from the orbital wall periosteum or randomly situated arachnoidal nests are rare. Meningiomas can involve the dura and contiguous bone of the orbital roof and higher wing of the sphenoid. Lesions can also involve the roof of the ethmoid or planum sphenoidale and can involve the sphenoid within the environs of the optic canal. Present most frequently in the fourth or fifth decade, occurring twice as typically in females. Ossifying fibroma of the orbit and paraorbital area is often diagnosed by the way, predilects to (black) ladies. Ossifying fibroma Well-circumscribed, expansile, mineralized mass, surrounded by a thick or skinny radiodense rimming. The most attribute feature is the presence of quite a few round or oval calcified bodies of assorted sizes, representing the psammomatoid (cementicle) our bodies. The lesion has an aggressive appearance with cortical break and extension in to surrounding tissue. Well-circumscribed, sharply delineated, spherical intrasinus mass, connected to the sinus wall broad-based or by a brief pedicle, often 2 cm in size. Rarely, massive osteoma in the frontal or ethmoid area may displace globe forward and cause proptosis. Very not often, an osteoma may erode by way of the dura, resulting in rhinorrhea or intracranial an infection. Psammomatoid active ossifying fibroma Psammomatoid energetic ossifying fibroma typically occurs in the sinonasal tract (ethmoid sinus, supraorbital frontal region) and doubtlessly might behave aggressively with locally invasive and damaging capabilities. Occurs in youthful age teams (first and second decades), with no gender predilection. Osteomas are benign mature bone-forming hamartomatous lesions which are almost exclusively recognized in the craniofacial skeleton (most widespread within the frontal and ethmoid sinuses). Symptoms related to paraorbital osteomas embody complications, facial swelling or deformity, and proptosis and ocular disturbances. Paraorbital osteomas are more widespread in males, most often within the second to fourth many years of life. Head websites of involvement embrace the mandible, maxilla, temporal bone, paranasal sinuses, and orbit. Giant cell tumors of the top and neck are unusual (sites of prevalence include the sphenoid, temporal, and ethmoid bones). Symptoms of lesions of the paraorbital region embody headache, diplopia, decreased vision, and proptosis. Chondromas of the paraorbital area, together with the sinonasal tract (nasal cavity septum, ethmoid sinus) and nasopharynx are rare. Symptomatic patients might current with nasal obstruction, enlarging, painless mass, proptosis, and complications. Other, uncommon benign osseous neoplasms in the orbital region: chondroblastoma and chondromyxoid fibroma. Giant cell tumor (osteoclastoma) Lobulated, expansile, intraosseous, mildly hyperdense delicate tissue mass with marked homogeneous or heterogeneous contrast enhancement. Malignant neoplasms Osteosarcoma Destructive, poorly delineated osteolytic, osteosclerotic, or mixed mass lesion, with minimal or large tumor bone formation inside the tumor proper and invading surrounding tissue. May be seen as a nondestructive, fairly properly delineated or harmful, and poorly delineated osteolytic or combined lesion with coarse calcifications. Craniofacial osteosarcomas occur in the jaws, paranasal sinuses, cranium, and orbital area. They have an equal gender predilection and happen generally a decade or two later than these with extrafacial osteosarcomas. Craniofacial chondrosarcomas are barely extra widespread in men than in women and primarily occur within the fourth to seventh a long time of life. Also seen are outward displacement of dislocated fragments after an orbital floor fracture and mucosal thickening in the left and opacification of the proper maxillary sinus. A soft tissue mass extending from the abnormal bone in to the extraconal area or outside the orbit is usually seen. A low-density or delicate tissue mass extending from outdoors the orbit in to the extraconal space, sharply or poorly marginated, with or without contrast enhancement, with transforming and bowing or with bony erosion and destruction of bony walls. Comments the most typical major malignant tumor of the orbit (excluding the globe) in children. Patients present with quickly progressive unilateral proptosis, ptosis, palpable mass, and ophthalmoplegia. Metastatic illness to the bony orbit mostly happens in the larger sphenoid wing and could additionally be limited to the bone or may have associated delicate tissue components within the extraconal house or in the contiguous extraorbital location. Malignant and benign tumors, including cysts, of the sinonasal cavities may invade the orbit. Orbital invasion of intracranial tumors through the skull base may be current, both through natural foramina or by bone destruction. Malignant neoplasms of the oral cavity can lengthen alongside the perineural-perivascular pathway in to the pterygopalatine fossa and then in to the orbit.
References - Zmora O, Tulchinsky H, Gur E, et al: Gracilis muscle transposition for fistulas between the rectum and urethra or vagina, Dis Colon Rectum 49:1316n1321, 2006.
- Morse FP 3rd, Dretler SP: Diagnosis and treatment of colovesical fistula, J Urol 111(1):22n24, 1974.
- Kenfield SA, Stampfer MJ, Chan JM, et al: Smoking and prostate cancer survival and recurrence, JAMA 305(24):2548n2555, 2011.
|
|