"Discount kamagra soft 100mg without a prescription, erectile dysfunction heart disease diabetes."By: Keira A Cohen, M.D. - Co-Director, The Johns Hopkins Center for Nontuberculous Mycobacteria and Bronchiectasis
- Assistant Professor of Medicine
 https://www.hopkinsmedicine.org/profiles/results/directory/profile/10003818/keira-cohen
Purchase kamagra soft 100 mg free shippingThe pronator teres and common flexor muscles are launched from their origins from the distal humerus medially. The brachioradialis, extensor carpi radialis longus, and common extensor muscle tissue are released laterally from the distal humerus. Occasionally, a distal humerus resection is carried out for a gentle tissue sarcoma that originates from certainly one of these muscle groups. In such a case, the muscle or muscle tissue which are involved by neoplasm are transected distal to the tumor in such a way that an sufficient margin is maintained. When resecting the flexor�pronator group, the department of the median nerve that provides the flexor digitorum superficialis is recognized and guarded, if possible. On the lateral side of the elbow, if the brachioradialis and customary extensor muscle tissue require resection, the posterior interosseous nerve is identified and protected to protect wrist and digit extension. A portion of the brachialis muscle, or even the whole brachialis muscle, may require resection, depending on the extent of the tumor. This is required for accurate positioning of the prosthesis and reaming of the ulnar canal. The triceps muscle is elevated off the distal humerus and may require partial or full resection of the medial head, relying on tumor extent. The elbow joint is opened anteriorly and the capsule launched circumferentially from the ulna�olecranon and radial head. The area where the humerus might be osteotomized is cleared of overlying brachialis muscle and triceps muscle. Proximally, the distal humeral component can be fit to a physique phase by way of a Morse taper. The physique phase is on the market in several lengths, so the size could be adjusted intraoperatively. The remaining humerus is flexibly reamed to accommodate as broad a stem as attainable. The proximal tip of the olecranon is shaved barely to accommodate the ulna stem, in order that it can be inserted immediately into the ulnar canal with out being inserted on an angle. Trial components are available to be used to ensure that the ulna element will sit correctly throughout the medullary canal of the proximal ulna. It is necessary to establish the anterior surface of the humerus earlier than the distal humeral component is inserted. After the cement cures, both parts are hooked up to one another with the appropriate hinge. With the elbow held in 60 degrees of flexion and the forearm totally supinated, these muscle tissue are transferred to as proximal a place as possible and sutured to the biceps muscle with no. The biceps is pulled distally and placed beneath tension while these muscular tissues are sutured to it. This step is very important if the prosthesis has been shortened, as a result of it restores the length�tension relation of the biceps muscle. The elbow is kept in 60 levels of flexion and fully supinated for the rest of the procedure. The origin of the flexor�pronator forearm muscular tissues also is transferred as far proximal as attainable and sutured to the medial border of the biceps and triceps muscle tissue. At this time, for postoperative analgesia, an epidural catheter can be threaded proximally alongside the median nerve, deep to the vascular sheath, to a level the place it might possibly bathe the entire brachial plexus with bupivicaine. Likewise, proximal transfer (ie, tensioning) of the brachioradialis and forearm flexor origins (ie, flexorplasty) is beneficial for restoring elbow flexion energy. The flexors (from the medial condyle) and the brachioradialis (mobile wad of 3) from the lateral condyle are reattached to the adjoining soft tissue. The T2-weighted picture typically is related to vital peritumoral edema, which overestimates tumor extent. The biopsy ought to be taken by way of the brachialis muscle and consistent with the proposed skin incision that would be used for definitive resection. Preservation of the biceps muscle is essential for restoring elbow flexion following reconstruction. The main neurovascular buildings are all identified in regular tissue proximal to the neoplasm along the medial side of the mid-arm. All important structures (ie, brachial vessels, median nerve, ulnar nerve, and radial nerve) are recognized, separated, and mobilized away from the neoplasm and distal humerus. Care is taken to protect the nerve to the flexor digitorum superficialis when tumors of the flexor�pronator group are resected. Likewise, care is taken to preserve the branches of the posterior interosseous nerve when tumors of the brachioradialis and common extensor muscle group are resected. The endoprosthesis is downsized 2 to three cm to facilitate gentle tissue protection, if essential. It is important to preserve the elbow in 60 levels of flexion and totally supinated when performing the delicate tissue reconstruction. Proximal switch under pressure of each the frequent extensor muscle origin and the flexor�pronator origin to either aspect of the biceps muscle accomplishes a flexorplasty of the elbow that assists with restoring elbow flexion energy. It could also be necessary to restore the length�tension relation of the biceps by pulling the biceps distally and suturing it to the forearm musculature beneath rigidity. Patients are covered from hand to shoulder with a bulky dressing and a splint that maintains the elbow in 60 levels of flexion. The extremity is elevated and the affected person remains primarily at mattress rest for 3 to four days. The dressings are changed approximately four days postoperatively, and the splint is reapplied to keep the elbow in 60 levels of flexion. The extremity is kept in a splint for a complete of 6 weeks to permit for sufficient muscle therapeutic and scarring. Immediately after surgical procedure, lively and passive range of motion of the wrist, hand, and digits, along with hand strengthening, is initiated and continued for 6 weeks whereas the arm is in the splint. Hand and wrist strengthening is continued throughout the whole rehabilitation course of. At 6 weeks, the patient is positioned in a hinged elbow brace and permitted lively, active assisted, and passive vary of movement from 30 degrees of flexion to a hundred thirty levels of flexion. At 12 weeks after surgical procedure, the brace is adjusted to allow full movement of the elbow. Strengthening of the elbow is initiated right now, with a 2-pound weight limit. At week 18, resistance strengthening can be elevated to a 5-pound weight limit if the patient is now in a position to deal with 2 pounds. At 6 months after surgical procedure, the load limit for resistance strengthening is elevated to 10 kilos.
Order kamagra soft with mastercardIn very proximal fractures, the place to begin for the guidewire is as far proximally in the scaphoid as attainable, on the mid-aspect of the membranous portion of the scapholunate ligament advanced. Percutaneous insertion of Kirschner wires into the proximal and distal scaphoid (S) fragments is helpful to facilitate manual reduction of a displaced fracture. A displaced scaphoid waist fracture has been stabilized with a derotational Kirschner wire positioned dorsal and ulnar to the guidewire. Note the begin line on the membranous portion of the scapholunate ligament (arrow). The 30-degree pronated oblique view demonstrating guidewire placement down the central axis of the scaphoid. It is important to insert the wire in the optimal position in all three views to keep away from violating the midcarpal joint or the volar floor of the scaphoid. In the case of minimal fragment separation, subtract four mm from the measured size of the wire to permit recession of the proximal screw beneath the articular surface. If fragments are more displaced, contemplate compression and choose a fair shorter screw. We use the bigger Acutrak screw when feasible, but the mini-Acutrak system could also be necessary in patients with a small scaphoid or if the fracture is located proximally such that insertion of an Acutrak screw could result in inadvertent propagation of the fracture to the insertion website with fragmentation of the proximal scaphoid. Remove the guidewire and assess screw position via fluoroscopy using the identical views. Proximally, divide the thickened radiolunate and radioscaphocapitate ligaments to permit exposure of the proximal scaphoid pole. Dissection over the radial facet of the scaphoid is restricted to avoid injury to the dorsal ridge vessel. Define and clear the fracture site by irrigation, sharp excision of periosteal flaps, and curetting of debris and hematoma. It is important to determine any bone loss, as compression during screw placement may end up in an iatrogenic malunion. The central axis guidewire is placed, bearing in mind all of the elements detailed above. The cannulated compression screw could additionally be inserted utilizing a freehand approach or a business gadget, which can facilitate simultaneous fracture reduction and guidewire positioning. Fluoroscopy is invaluable throughout wire and screw insertion and to affirm correct placement and fracture discount as described above. Fracture Reduction and Fixation Obtain appropriate fracture alignment through longitudinal traction adopted by wrist manipulation. An anatomic reduction can also be achieved by direct manipulation of the fragments with a dental pick, pointed reduction forceps, or joystick Kirschner wires. Pronate and flex wrist in the course of the dorsal strategy to permit appropriate trajectory. Provisional derotational Kirschner wires placed before screw insertion can be used to stabilize fragments throughout screw insertion. Recognize comminution and bone loss to avoid inadvertent shortening or malreduction with screw compression. Small proximal pole fracture Use of a small screw (ie, mini-Acutrak) could also be essential to forestall comminution of the proximal fragment. Rangeof-motion exercises are begun and a detachable forearm-based thumb spica splint is worn. After forged removing, a proper supervised therapy program is initiated to achieve passable vary of movement, energy, and function. Fracture healing is assessed at 2, 6, and 12 weeks postoperatively with plain radiography. However, recent studies have raised potential considerations concerning eccentric screw placement and injury to the scaphotrapezial articulation with this approach. Intraoperative technical issues Inadvertent bending or breakage of the guidewire can occur if the wrist is dorsiflexed with the wire in position or during drilling before screw insertion. Care should be taken to confirm that the screw is fully seated beneath the articular cartilage to avoid prominence and erosion of the distal radius articular floor. Similarly, failure to rigorously choose accurate screw size intraoperatively can lead to prominence and erosion of the scaphotrapezial articulation. Internal fixation of acute, nondisplaced scaphoid waist fractures through a restricted dorsal strategy: an evaluation of radiographic and practical outcomes. Non-union of the scaphoid: therapy with cannulated screws in contrast with therapy with Herbert screws. The classification system proven in Table 1 describes them within the context of therapy options. Micromotion disrupts vascular perforators (often the one blood supply), leading to bone resorption and further decrease in mechanical stability. Proximal pole fractures are significantly in danger for nonunion for each mechanical (long distal lever arm and a small proximal contact area) and vascular causes. Other than data regarding earlier operative and nonoperative remedies, the extra data for analysis and therapy choices comes more from imaging. Preoperative Planning Advanced degenerative modifications secondary to scaphoid nonunion are a relative contraindication to restore of a nonunion. Advanced imaging, as mentioned earlier, is crucial for appropriate preoperative planning. Approach A dorsal method is used for proximal pole fractures to present probably the most safe fixation (as a fundamental precept, think of securing the island to the mainland). Nonunion of a distal pole scaphoid fracture, though uncommon, is greatest approached volarly. Traction for arthroscopy may be performed with both a traction tower or a simple horizontal pulley traction system. Place a 19-gauge needle into the fracture site and confirm place fluoroscopically. Exit on the base of the thumb in an area devoid of neurovascular structures and withdraw it until the proximal tip is on the fracture web site. Sometimes a percutaneous snap could have to be launched for extra leverage or to right translational deformities. Fracture during reduction exhibiting Kirschner wire positioned distally to capture reduction. A successfully placed central axis scaphoid wire will hit the crossing wires in the distal scaphoid. The use of two Kirschner wires limits bending forces and acts as an antirotation assemble during scaphoid reaming and screw placement. Fluoroscopy can be used with 19-gauge needles to determine the radiocarpal and midcarpal portals. This maneuver limits iatrogenic injury to the joint, which may result from multiple makes an attempt to introduce a blunt trocar blindly.
Diseases - Dent disease
- Marphanoid syndrome type De Silva
- Pendred syndrome
- Phytanic acid oxidase deficiency
- Von Recklinghausen disease
- EPP (erythropoietic protoporphyria)
Discount kamagra soft 100mg without a prescriptionBecause most primary bone sarcomas lengthen into the surrounding gentle tissues, the overlying muscle should be eliminated en bloc with the tumor. In this case, the deltoid muscle should be removed with the tumor, and the biopsy tract ought to be included within the surgical specimen, indicating the choice of a transdeltoid strategy via the anterior third of the muscle. The traditional deltopectoral strategy for such a biopsy would necessitate a wider resection of the pectoralis main muscle, compromise its subsequent use for gentle tissue reconstruction, and probably contaminate the main neurovascular bundle of the higher extremity. Biopsy tracts around the proximal and distal femur; a distinction is made between lateral and medial lesions. Biopsy tracts around the proximal tibia; a distinction is made between lateral and medial lesions. It can be either "incisional," by which case solely a representative specimen is faraway from the lesion, or "excisional," during which case the lesion is totally eliminated. Open incisional biopsy remains probably the most dependable diagnostic method to which all different biopsy modalities must be compared. It permits the pathologist to evaluate mobile morphologic options and tissue structure from completely different websites of the lesion. Furthermore, it supplies material for performing ancillary studies, similar to immunohistochemistry, cytogenetics, molecular genetics, move cytometry, and electron microscopy. These studies might help in the analysis and subclassification of bone and delicate tissue tumors, and, due to this fact, guide the choice of definitive therapy. Open biopsies are criticized due to the elevated threat of complications, which can include iatrogenic injury to blood vessels or nerves, difficult wound healing, wound an infection, and tumor cell contamination along the biopsy tract and subsequent local recurrence. Furthermore, open biopsies are associated with significantly higher costs of hospitalization and operating room time. Thus, guided needle biopsies have become the standard method in most orthopaedic oncology facilities. When a purely intraosseous bone lesion is being biopsied, make a cortical window, giving careful consideration to its form. Clark et al3 evaluated the influence of three forms of biopsy gap shapes-rectangular gap with square corners, rectangular hole with rounded corners, and oblong hole with rounded ends-on the breaking energy of human femora. They discovered that an rectangular hole with rounded ends afforded the greatest residual strength. Therefore, when the biopsy specimen should be taken from the bone, a small circular gap must be made in order that only minimal stress-risers are created. A massive hematoma may dissect the gentle and subcutaneous tissues and contaminate the entire extremity, making limb-sparing surgical procedure unimaginable. The smallest longitudinal incision that allows an sufficient specimen to be obtained must be used. A transverse biopsy incision requires an extended and curved incision to permit its incorporation at the time of the definitive resection. These incisions typically cross pressure traces, compromise the blood supply to the myocutaneous flaps, and doubtlessly contaminate a bigger surgical field. As a outcome, postoperative radiation therapy, when indicated, is run to a wider area. Open biopsy of a high-grade soft tissue sarcoma of the left buttock by the use of a transverse incision. A long, curved incision was used on the time of the definitive surgical procedure to allow sufficient resection as nicely as subsequent closure of pores and skin flaps. Intersecting long incisions were required at the time of definitive surgery to take away the biopsy web site en bloc with the tumor. An rectangular cortical window with rounded ends affords the greatest residual energy and is beneficial for biopsy of purely intraosseous lesions. A drain have to be positioned in proximity to and parallel to the site planned for incision of the definitive process. The drain was positioned within the flank, inflicting appreciable contamination of the ipsilateral pelvic girdle. To enable hemostasis, the tourniquet should be eliminated before wound closure Use drains if necessary. The drain path is considered contaminated and should be excised with the surgical specimen. Guidelines regarding the excision of the draining tract are related, due to this fact, to those who apply to the biopsy tract. Plan website and tract according to the planned incision and tract of the definitive surgery. The periphery of musculoskeletal tumors is preferable to a central site for biopsy. The real threat of open and needle biopsies is that they may spread tumor cells domestically and facilitate native tumor recurrence when performed inadequately. The hazards of biopsy in patients with malignant primary bone and delicate tissue tumors. Making the analysis: keys to a profitable biopsy in kids with bone and soft-tissue tumors. Comparison of needle core biopsy and fineneedle aspiration for diagnostic accuracy in musculoskeletal lesions. The traditional surgical strategy to the remedy of sarcoma, namely quick amputation of the extremity, was advocated within the early Nineteen Sixties and Nineteen Seventies to ensure local management of illness. Early pioneers in orthopaedic oncology worked diligently to define the optimum level of amputation and developed strategies to handle wounds of the pelvis and shoulder girdle following hind- or forequarter amputation. Only after the introduction of efficient doxorubicin- and methotrexate-based chemotherapy protocols within the early Seventies could options to amputation be thought-about. A handful of surgeons started to challenge the orthodoxy of amputation in kids and adults with bone sarcomas. Marcove, Francis, and Enneking were among the many pioneers who developed the rationale and primary methods used in limb-sparing surgery. The former two surgeons have been the first within the United States to develop endoprosthetic replacements for tumor sufferers. Starting with a very few extremely chosen sufferers with extremity osteosarcoma, limb-sparing surgery now could be a remedy possibility for most bone and soft tissue sarcomas, not solely of the extremities, however of the pelvis and shoulder girdles as well. Today, over 90% to 95% of tumor sufferers may be expected to endure successful limb-sparing procedures when treated at a significant middle specializing in musculoskeletal oncology. This dramatic alteration in affected person care required significant advances along many fronts, including the next: Better understanding of tumor development and metastasis Determination of applicable surgical margins Use of effective induction (neoadjuvant or preoperative) chemotherapy Development of improved approaches, preserving delicate tissue vascularity Deeper understanding of skeletal biomechanics Advanced material engineering and manufacturing strategies Development of inherently stable modular prostheses. The chapters in this section outline in particular detail lots of the surgical approaches and techniques of oncologic resection and reconstruction presently used by leaders within the subject of orthopaedic oncology. A successful limb-sparing surgical procedure consists of three interdependent phases performed in sequence: 1. History of Endoprosthetic Reconstruction Austin Moore and Harold Bohlman, in 1940, were the first to publish an example of endoprosthetic reconstruction for a bone tumor, consisting of a custom-designed Vitallium proximal femur used for a affected person with an enormous cell tumor of bone.
Buy 100mg kamagra softSelect a distal pin hole and slide a radial pin plate over the transstyloid Kirschner wire. Insert a second transstyloid Kirschner wire by way of a non-adjacent distal pin hole. Use the earlier technique to limit penetration of the Kirschner wire through the far cortex to 1 to 2 mm. Complete the bend with a pin clamp, overbending barely to allow the hook to snap into an adjoining pin gap or over the sting of the plate. If the plate is aligned over the ulnar half of the shaft, add a 15-degree torsional bend to the plate (twist the proximal end of the plate into slight supination). If the Kirschner wire ideas protrude past the volar cortex, they are often reduce flush to the bone surface by way of a volar incision. Dorsal Buttress Pin Through a dorsal method, expose and cut back the dorsal ulnar nook fragment, dorsal wall fragment, or both. Radial and ulnar pin plate fixation of a three-part articular pattern (radial column and ulnar corner fragment). The Kirschner wires should be separated by about 1 cm and must be transverse to the longitudinal axis of the shaft. Leave the ulnar leg 2 to three mm longer than the radial leg so one leg may be engaged at a time. Repeat with the radial Kirschner wire to engage the radial leg of the buttress pin. Placing an implant upside-down on bone to template the trajectory of the Kirschner wires. Fixation of a three-part articular fracture with radial column and ulnar corner fragment with radial column plate and dorsal buttress pin. If volar rim fragmentation is associated with an axial instability sample, the fragment should be of adequate size and strength to permit distal locked screw purchase to obtain angular correction of the dorsiflexion deformity. If a shortened radial column fragment is present, first restore radial size and provisionally hold it with a transstyloid Kirschner wire to unload the lunate facet. Apply a small-fragment volar plate and repair it proximally with cortical bone screws. Reduce the volar rim fragment as a lot as attainable and note the orientation of the teardrop on the 10-degree lateral view. Adjust the trajectory of the legs of the implant to make a 70-degree angle with the bottom of the wire kind. Noting the entry web site of the Kirschner wire, carefully remove the ulnar Kirschner wire and have interaction the ulnar leg of the volar buttress pin. In some instances, impacted free articular fragments could additionally be adequately supported by a properly applied locking plate that provides subchondral assist. An various method is to use structural bone graft to help the free articular fragment together with fragment-specific fixation of the surrounding cortical shell, resulting in containment of the graft within the metaphysis. The dorsal buttress pin can also be used for direct subchondral support of impacted articular fragments. If the articular floor is tilted dorsally, the carpal side horizon identifies the dorsal rim. If the articular surface is tilted volarly, the carpal facet horizon identifies the volar rim. Identify and begin reduction with the fragment that stabilizes the carpus to its normal spatial relationship. Adding structural bone graft, either through the fracture line at the base of the radial column or by way of a dorsal defect, may help stabilize the discount throughout operative fixation. Make sure the distal articular fragments are translated toward the ulna before finishing volar fixation. An elastic, slightly overcontoured radial column plate might help close sagittal fracture gaps and seat the sigmoid notch towards the ulnar head. Consider volar buttress pin fixation for an especially distal or dorsally rotated volar rim fragment. If wanted, the volar buttress pin may be contoured as wanted to match the arc of curve of the flare of the volar shaft. Unrecognized carpal ligament injury Maintain a excessive index of suspicion for ligamentous accidents of the carpus. Consider arthroscopic evaluation, notably in the context of radial or dorsal shear fractures, carpal avulsion and instability patterns, or articular fractures associated with a major longitudinal stepoff between the scaphoid and lunate facets. Use radial column plate to push distal fragment towards ulna to seat sigmoid notch towards ulnar head. Reduce and repair ulnar nook and volar rim fragments to restore congruity of sigmoid notch. Early range of movement and mobilization of soft tissues Avoidance of constricting bandages and postoperative swelling Stiffness: gradual, restricted return of motion of wrist, forearm, and fingers, typically related to pain Tendinitis or rupture: pain with resisted movement, loss of tendon function, clicking and pain Use implants which have a low distal profile. If secure, apply a removable wrist brace and instruct the patient to provoke mild range-of-motion workout routines of the fingers, wrist, and forearm twice or extra day by day as tolerated. For non compliant patients or injuries with tenuous fixation, use a cast for two to 3 weeks postoperatively. Avoid resistive loading throughout the wrist till signs of radiographic therapeutic are current; sometimes this happens by four weeks postoperatively. Specifically instruct older patients to not push up out of a chair or carry heavy objects after surgery. Benson et al2 reported on 85 intra-articular fractures in eighty one sufferers with a imply follow-up of 32 months. Flexion and extension movement was 85% and 91% of the opposite facet at final follow-up. Sixty-two % of sufferers had a 100-degree arc of flexion�extension and regular forearm rotation by 6 weeks postoperatively. Pin plates are able to resist translational displacements however are much less efficient for stopping loss of length; they require osseous contact between the proximal and distal fragments or further support by a secondary implant that will buttress the subchondral surface. Tendinitis or tendon rupture: uncommon If pins are famous postoperatively to back out, they should be removed. Leaving the distal 1 cm of tendon sheath of the first dorsal compartment intact helps keep away from tendon contact with hardware. Using low-profile implants dorsally, overlaying the distal ends with a strip of retinacular sheath, or each can be helpful. The surgeon ought to avoid leaving screws or pins protruding from the dorsal or volar surfaces of the bone. Painful hardware: rare Painful hardware could be related to migration of a pin or settling of the fracture proximally. Late arthritis is unusual and possibly associated to the quality of the articular restoration. Infections, bleeding, carpal tunnel syndrome, and other nerve accidents are uncommon and often associated to the first injury. Complex regional pain syndrome is uncommon and could also be related to initiation of early movement after surgery. Open reduction and internal fixation of unstable distal radius fractures: results utilizing the TriMed system.

Purchase kamagra soft 100mg without a prescriptionEpicondylitis could be seen with medial collateral ligament instability whereby myotendinous overload happens in an try and dynamically stabilize the ulnohumeral joint. However, a larger proportion of sufferers with medial epicondylitis go on to surgical remedy when compared to sufferers with lateral epicondylitis. At occasions the irritation is important enough to cause irritation of the ulnar nerve as it enters the flexor carpi ulnaris, inflicting ulnar nerve signs (eg, native irritability and distal numbness and tingling). Examination strategies embrace the next: Palpation of the medial epicondyle for tenderness, a common finding in medial epicondylitis Resisted pronation is very delicate for medial epicondylitis. Careful patient selection will guarantee a wonderful end result with surgical administration. If essential, ulnar nerve decompression should be performed in situ, using subcutaneous or submuscular transposition. In skinny patients, and particularly those who have life in which the inner elbow is struck incessantly, we prefer submuscular transposition with flexor pronator lengthening, which definitively treats epicondylitis as nicely. These typically will current more abruptly, with acute or continual ache, ecchymosis, and swelling. Approach the elbow should be examined after the administration of anesthesia to guarantee stability, and the result documented in the operative note. The aim of surgery is to d�bride the degenerative tissue on the flexor�pronator origin and create an setting conducive to correct therapeutic of the tendon. The arm is externally rotated on the shoulder and padding is positioned beneath the elbow. The arm ought to rest ready allowing prepared entry to the medial side of the elbow with out requiring fixed holding by an assistant. The subcutaneous tissues are gently swept away, exposing the fascia of the flexor�pronator mass. The ulnar nerve is palpated, and the elbow is put by way of a range of movement to check for ulnar nerve subluxation. The actual location can be altered depending on clinical examination and the point of maximal tenderness. The pathologic tissue is d�brided to margins displaying an organized, tendinous appearance. The muscle interval is closed with a running measurement zero Vicryl suture and tied with inverted knots. Failure to absolutely excise devitalized tendon Injury to the medial collateral ligament it will result in a poor outcome or recurrence; the rehabilitation protocol can be delayed in circumstances that require extra significant d�bridement. The ligament is deep to the tendon and lies on the anterior capsule, more posterior than the world of tendinosis, and could be distinguished from the rougher tendon origin. It is uncommon for a affected person to have completely no enchancment in ache after surgical procedure, even when the subjective outcome is Chapter 64 Open and Arthroscopic Treatment of Lateral Epicondylitis Peter J. It is commonly referred to as "tennis elbow" and is likely more correctly termed "lateral elbow tendinopathy. Most also show increased intratendon sign or tendon thickening on T1-weighted sequences. Patients stricken with lateral epicondylar tendinopathy generally have interaction in repetitive forceful gripping activities as they raise, pull, twist, and push objects. Nighttime wrist bracing to stop palmar wrist flexion and prolonged pressure on the extensor tendons Physical or occupational therapy to supervise and instruct on stretching and strengthening protocol for patients not otherwise inclined to carry out these workouts Corticosteroid injection has had good response within the early stages of the situation. Platelet-rich plasma or blood clot tendon injection and botulinum toxin muscle injection presently are under investigation. Careful affected person selection is crucial to ensure an excellent end result following surgical administration. No prospective randomized research have but been carried out to look at the benefits of open versus arthroscopic methods for the therapy of lateral epicondylitis. However, I select arthroscopic remedy if there are any signs of a plica or synovial irritation (endpoint pain) that can allow direct examination and remedy. The arm is internally rotated at the shoulder, and padding is placed beneath the elbow. The arm should relaxation ready that enables ready access to the lateral side of the elbow with out requiring fixed holding by an assistant. The elbow ought to be examined after the administration of anesthesia to guarantee stability, and the result documented in the operative note. The aim of surgery is to d�bride the degenerative tissue at the extensor origin and create an surroundings conducive to correct therapeutic of the tendon. Distally, a fats stripe alongside the aponeurosis typically is seen along this dissection aircraft. The abnormal tendon tissue to be excised could be recognized by its grayish, unorganized mucoid look and must be sharply excised. If uncovered, the joint must be inspected for degenerative change, which, if current, sometimes is found beneath a plica. A rongeur is used to roughen the anterior portion of the lateral epicondyle to a bleeding surface with out removing cortical bone. Surgical strategy uses a 3-cm incision over the lateral epicondyle and could be extended in line with the forearm axis to avoid harm to the lateral collateral ligament. The anterior portion of the lateral epicondyle is scratched clear of degenerative tissue with a no. We choose the lateral decubitus place with the assist of the Tenet Spider Arm Holder (Smith & Nephew Inc. A small longitudinal portal incision is made about 2 cm proximal to the medial epicondyle and just anterior to the medial intermuscular septum. A curved hemostat is used to unfold underlying tissues and really feel the medial intermuscular septum, after which is slid alongside its anterior floor to the lateral, then anterior humerus. This is repeated with the scope trocar, which is then handed distally along the anterior humerus towards the radiocapitellar joint, piercing the capsule and entering the joint. A hooked electrocautery probe is helpful to divide a plica to facilitate its resection. A lateral portal is established at the anterior rim of the radial head, at or simply proximal to the radiocapitellar joint, usually immediately via the primary pathology. This will end in a poor end result or recurrence; the rehabilitation protocol may be delayed in circumstances that require extra significant d�bridement. The ligament is posterior to the mid-radiocapitellar joint, and dissection on this area ought to be prevented. These outcomes hold true for each brief follow-up and more than 10 years of follow-up. It is uncommon (5% of cases) for a affected person to have completely no enchancment in ache after surgical procedure, even when the subjective end result is unsatisfactory. The supratendinous retinaculum originates 2 to 3 cm proximal to the radiocarpal joint and ends distinctly on the carpometacarpal joints.
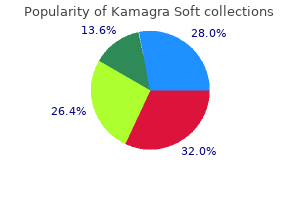
Discount 100mg kamagra soft with visaA detailed description of the scientific, radiographic, and pathological traits for the commonest sarcomas is presented. Soft tissue sarcomas are classified in accordance with the adult tissue that they resemble. Similarly, bone sarcomas often are classified based on the kind of matrix production: osteoid-producing sarcomas are categorised as osteosarcomas, and chondroid-producing sarcomas are categorized as chondrosarcomas. Tumors arising in bone and soft tissues have characteristic patterns of biologic conduct due to their frequent mesenchymal origin and anatomic environment. The grade is predicated on tumor morphology, extent of pleomorphism, atypia, mitosis, matrix production, and necrosis, with the 2 main components being mitotic rely and spontaneous tumor necrosis. Sarcomas form a solid mass that grows centrifugally, with the periphery of the lesion being the least mature. In contradistinction to the true capsule that surrounds benign lesions, which is composed of compressed regular cells, sarcomas often are enclosed by a reactive zone, or pseudocapsule. This pseudocapsule consists of compressed tumor cells and a fibrovascular zone of reactive tissue with a variable inflammatory element that interacts with the encompassing regular tissues. The thickness of the reactive zone varies according to the histogenic type and grade of malignancy. High-grade, and infrequently low-grade, may break through the pseudocapsule to kind metastases, termed skip metastases, throughout the similar anatomic compartment during which the lesion is situated. These neoplasms characterize less than 1% of all adult and 15% of pediatric malignancies. As of 2006, the annual incidence within the United States, which remains comparatively constant, was approximately 6000 to 7000 soft tissue sarcomas and 2750 bone sarcomas. In 2006, the general mortality fee was 30% for gentle tissue sarcomas and 45% for bone sarcomas. In the previous two decades, each survival and high quality of life of sufferers with soft tissue and bone sarcomas have improved dramatically on account of the multimodality treatment method. Limb-sparing surgical procedure, utilized in combination with chemotherapy and radiation therapy, can obtain treatment in the majority of patients with delicate tissue and bone sarcomas, and resection is carried out in lieu of amputation in more than 90% of all patients. The most typical bone sarcomas are osteosarcoma, chondrosarcoma, and Ewing sarcoma. A pseudocapsule of a high-grade gentle tissue sarcoma (arrows) composed of compressed tumor cells and a fibrovascular zone of reactive inflammatory response. Unique features are formation of reactive zone, intracompartmental development, and, rarely, the presence of skip metastases. Skip nodules are tumor foci not in continuity with the principle tumor mass that form exterior the pseudocapsule. However, the articular cartilage is an anatomic barrier to tumor extension and really hardly ever is immediately violated by a tumor. Although gross involvement of the epiphysis and medial cortical breakthrough and gentle tissue extension are evident, the articular cartilage is unbroken. This phenomenon permits intra-articular resection of high-grade sarcomas of the distal femur typically. It is only at a later stage that the walls of the compartment are violated (either the cortex of a bone or aponeurosis of a muscle), at which era the tumor breaks into a surrounding compartment. Typical anatomic barriers are articular cartilage, cortical bone, and fascial borders. Most bone sarcomas are bicompartmental on the time of presentation; they destroy the overlying cortex and extend immediately into the adjoining soft tissues. Joint involvement in sarcoma is uncommon, because direct tumor extension through the articular cartilage is rare. Metastatic Bone and Soft Tissue Sarcomas Unlike carcinomas, bone and delicate tissue sarcomas disseminate virtually completely through the blood. Hematogenous spread of extremity sarcomas is manifested by pulmonary involvement within the early levels and by bony involvement in later levels. Abdominal and pelvic soft tissue sarcomas, on the other hand, sometimes metastasize to the liver and lungs. Low-grade delicate tissue sarcomas have a low (under 15%) price of subsequent metastasis, whereas high-grade lesions have a significantly larger (over 20%) rate of metastasis. Ewing sarcoma of the distal two thirds of the femur (A) and osteosarcoma of the proximal tibia (B). Most high-grade bone sarcomas are bicompartmental on the time of presentation (ie, they contain the bone of origin in addition to the adjoining delicate tissues). Plain radiograph of the proximal femur revealed direct invasion through the cortical bone with a pathological fracture of the lesser trochanter (arrows). In surgery, exploration of the sciatic nerve revealed direct tumor involvement with extension beneath the epineural sheath. Extension of an osteosarcoma of the distal femur to the knee joint along the cruciate ligaments (arrow factors to tumor); the articular cartilage is intact. Knee joint extension of a high-grade sarcoma of the distal femur is a rare event, necessitating extra-articular resection (ie, en bloc resection of the distal femur, knee joint, and a element of the proximal tibia). Most patients with high-grade primary bone sarcomas, not like delicate tissue sarcomas, have distant micrometastases at presentation; an estimated 80% of patients with osteosarcomas have micrometastatic lung disease on the time of diagnosis. For this purpose, in most cases, remedy of a high-grade major bone sarcoma may be achieved solely with systemic chemotherapy and surgery. Because of that distinction in metastatic functionality, the function of chemotherapy in the treatment of soft tissue sarcomas and its impact on survival are nonetheless matters of some controversy. Prognostic elements for gentle tissue sarcomas include grade, tumor measurement, depth, age, margin status, location (proximal vs. Staging Staging is the method of classifying a tumor, especially a malignant tumor, with respect to its degree of differentiation, as nicely its native and distant extent, to plan the treatment and estimate the prognosis. Staging of a musculoskeletal tumor is predicated on the findings of the physical examination and the results of imaging studies. Biopsy and histopathological analysis are important components of staging however should all the time be the final step. An essential variable in any staging system for musculoskeletal tumors, in distinction to a staging system for carcinomas, is the grade of the tumor. The system most commonly used for the staging of soft tissue sarcomas is the one developed by the American Joint Committee on Cancer (Table 1). Lateral plain radiograph of the lumbar spine, showing metastatic high-grade osteosarcoma to the physique of L3 vertebra (arrow). T1 Intracompartmental; T2 extracompartmental c M0 No regional or distant metastasis; M1 regional or distal metastatic. The anatomic site (T) may be either intracompartmental (A) or extracompartmental (B). This data is obtained preoperatively on the idea of the info gained from the varied imaging modalities. A tumor is classified as intracompartmental whether it is bounded by pure obstacles to extension, similar to bone, fascia, synovial tissue, periosteum, or cartilage. An extracompartmental tumor may be both a tumor that has violated the borders of the compartment from which it originated, or a tumor that has originated and remained within the extracompartmental space. Since that time, the utilization of neoadjuvant chemotherapy has been proven to decrease tumor size and facilitate limb-sparing surgery, in addition to reduce the native recurrence price.
Ground Holly (Pipsissewa). Kamagra Soft. - Are there safety concerns?
- Urinary tract infections (UTIs), kidney stones, spasms, fluid retention, seizures, anxiety, cancer, ulcerous sores, and blisters.
- How does Pipsissewa work?
- What is Pipsissewa?
- Dosing considerations for Pipsissewa.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96144
Purchase genuine kamagra soft on lineThe fingertip ought to be able to touch the distal palmar crease (110 degrees of flexion). It could also be necessary to advance the volar plate by step-cut lengthening of the checkrein ligaments. The holes within the center phalanx ought to be as far dorsal and lateral as potential for maximum stability. Alternatively, the sutures may be tied immediately onto periosteum through a small incision distal to the central slip insertion. In the acute setting, fractured bone fragments collected in the course of the volar plate detachment may be positioned in the defect of the middle phalanx, distal to the advanced volar plate. Alternatively, the joint reduction can be maintained with an articulated exterior fixator to enable for early movement. The total diagram of this procedure illustrates the joint with a double-ended Kwire for stability and the volar plate secured by sutures. Meticulous dissection of each neurovascular bundles is required earlier than "shotgunning" the joint open. Failure to lengthen the checkrein ligaments could result in an unacceptable contracture. Volar plate arthroplasty for osteoarthritis of the proximal interphalangeal joint: a preliminary report. The base of the middle phalanx often is very comminuted, and the articular fragments may be considerably impacted. Dorsal lip fracture therapy is complicated by the necessity to re-establish continuity of the extensor tendon insertion onto the center phalanx. Unstable palmar lip fractures are amenable to treatment with hemi-hamate autograft and are the focus of this chapter. The solely restraints on center phalangeal dorsal translation are the palmar plate and the cup-shaped geometry of the middle phalanx articular floor. The middle phalangeal palmar lip wraps around the proximal phalanx head and acts as a hook, preventing dorsal translation. The palmar plate is not hooked up, and the middle phalangeal palmar lip is disrupted. The slope of the remaining center phalangeal articular surface encourages the middle phalanx to journey up and over the proximal phalangeal head. Hastings6 has shown that when 42% of the palmar articular surface is damaged, the joint always reveals dorsal instability. In the clinical setting, fractures with as little as 30% articular surface involvement may be unstable. The upward pull of the central tendon insertion and the distal superficialis insertion pull and push the center phalanx up and over the proximal phalangeal head. Articular injury in extra of 50% of the joint surface at all times renders the joint unstable, whereas fractures involving less than 30% often are stable. If the joint is unstable, osteosynthesis with lag screws often is possible because of the shortage of comminution and the substantial dimension of the fragment. Up to 80% of the joint floor could be involved, and the articular fragments are often deeply impacted into the soft metaphyseal bone. Inspect the lateral radiograph to decide the share of joint floor fractured and the standard of the discount. On each lateral radiograph taken throughout the therapy course, fastidiously scrutinize the standard of the reduction. When over 50% of the middle phalanx articular surface is consumed by fracture, all restraints to dorsal subluxation are misplaced. The cup-shaped geometry of the middle phalanx base must be restored and the palmar plate reattached. Both goals could be accomplished with osteosynthesis of a single giant fragment,2,three,8 palmar plate arthroplasty,1 or a hemi-hamate osteochondral autograft. If the joint hyperextends, some flexion should be maintained for three weeks while the fracture fragments consolidate sufficient to restore practical palmar plate continuity. The main therapy objective is to maintain joint reduction whereas the middle phalanx palmar fragments consoidate and restore the cup-shaped geometry of the middle phalanx base. Options vary from easy extension block splints11 or pins14 to exterior traction12,thirteen or advanced frame constructions. Hemi-hamate arthroplasty is a useful salvage process for remedy that has failed with traction, external fixation gadgets, extension block splinting, or palmar plate arthroplasty. Undamaged cartilage have to be present on the palmar 50% of the proximal phalanx head and on at least a small rim of the middle phalanx dorsal articular floor. Extensive harm has occurred to the palmar lip of the middle phalanx, however the dorsal cortical margin and a small quantity of dorsal articular cartilage stay intact. If coronal airplane angulation is observed, will most likely be necessary to degree the middle phalangeal joint floor throughout fracture site preparation and graft placement. Positioning Position the patient supine with the arm extended onto a radiolucent hand table. It will be essential to take away the lead hand intermittently to facilitate use of fluoroscopy. Identify the neurovascular bundles proximally and mobilize them away from the flexor sheath throughout the length of the dissection. This allows full visualization of the collateral ligaments and facilitates retraction of the neurovascular bundles without excessive traction. Take care to stop superficial injury to the flexor tendons whereas incising the flexor sheath. The distal attachment of the palmar plate will already be detached (ie, avulsed) as a end result of the injury, nevertheless it nonetheless may have to be gently mobilized. If the fragments are large sufficient to accept interfragmentary screws, consider open discount and inner fixation as an alternative of continuing with the hemi-hamate autograft. Leave a small stump on the center phalanx to facilitate restore at the end of the process. If essential, use a Freer elevator to stop impingement of the intact dorsal base of the center phalanx in opposition to the top of the proximal phalanx. Caution: forceful hyperextension might lead to fracture of the dorsal articular fragment. Only if completely needed, release 1 to 2 mm of the A4 pulley to facilitate enough mobilization of the flexor tendons. Use an oscillating saw to level the surface of the bony defect and to remove adequate bone to enable graft placement. Make the cuts parallel to the dorsal margin of the articular surface and the long axis of the phalangeal shaft.
Order kamagra soft 100mg visaIf the bone is osteopenic, a screw longer than the preliminary measurement ought to be placed to ensure that both cortices are engaged. Otherwise, the plate will not be held securely, and the reduction shall be compromised. After the remaining screws have been secured, this screw can be changed with one of the applicable length. Distal Fragment Reduction Plate Application Apply a fixed-angle volar plate to the volar floor of the distal radius and shaft. Position the plate to accommodate for the distinctive design traits of the plating system in addition to the situation of the fracture fragments. Each plating system has unique traits that decide its optimal placement. Ideally, the plate should be positioned as close to the articular margin as potential without the distal locking pegs or screws penetrating the joint. If the fracture has not but been totally lowered, this must be taken under consideration when placing the device. Clamp the beforehand utilized lobster claw to the proximal portion of the plate to maintain the plate centralized on the radius shaft. Then fluoroscopically verify proper plate place in both the distal�proximal and radioulnar instructions. Once the proximal plate has been secured, execute any additional reduction wanted. Additional distraction and ulnar deviation right radial collapse and loss of radial inclination. K-wires (arrows) are helpful as provision fixation until alignment may be confirmed radiographically and screws placed. The final reduction is carried out with traction on the hand and with the radius held proximally with a clamp. The volar plate acts as a powerful buttress (arrow), permitting the translated lunate to push on the volar radius (*) and correct the dorsal angulation deformity. The extensor pollicis longus is at biggest threat of damage from a protruding screw. Some plate methods permit for provisional fixation using K-wires placed through the distal plate. Do not penetrate the dorsal distal radius with the drill, to shield the dorsal extensor tendons. A true lateral view of the distal radius is critical to judge placement of the radial screws. A radiograph is being taken with the wrist perpendicular to the x-ray beam (arrow). By lifting the hand and wrist 20 levels off the table, a "true" lateral picture could be achieved. If the K-wires are deemed crucial for fracture stability, they can be left in place and eliminated 4 to eight weeks later If residual instability exists, add extra fixation with K-wires, an exterior fixator, a dorsal plate, or a combination. Consider strategies to reduce postoperative ache: Percutaneous placement of a pain pump catheter Injection of a long-acting native anesthetic Close the subcutaneous tissues with 4-0 absorbable suture and reapproximate the skin with interrupted 4-0 or 5-0 nylon sutures or a running subcuticular stitch. A bulky dressing is applied with a volar splint holding the wrist in a impartial position. It is finest employed (if at all) for a malunion, or maybe for a fracture with minimal articular comminution. This approach is difficult, because it has to account for the longitudinal and translational alignment of the plate earlier than the reduction has been achieved. Affix the plate to the distal fragment, accounting for the place the plate will sit on the radius shaft as soon as the discount is completed. Once distal fixation is full, safe the proximal plate to the radius shaft, thereby completing the discount. The volar plate is applied with the distal screws placed first (parallel to distal articular surface). Use extra care with deep dissection within the presence of hematoma or important swelling. Use a lobster-claw clamp on the proximal radius shaft for management of the forearm and as a reference for the lateral margins. Use devices to disimpact and reduce articular fragments via the fracture itself, either volarly, dorsally, or both. Employ a short lived K-wire to stabilize the reduction before placement of the plate. Place the plate as distal as potential, as much as the volar tear drop of the distal radius, if potential. Evaluate the screws for attainable joint penetration using 360-degree fluoroscopic photographs. The initial "oblong hole" screw must be barely longer than the measured size to guarantee better preliminary fixation. At 6 to 8 weeks, the splint is discontinued, and progressive strengthening exercises are superior. At 10 to 12 weeks, the patient often could be discharged to all actions as tolerated. Results appear to be superior within the early recovery period, with the ultimate outcome yielding equal outcomes among all fixation teams. Complications may be categorized into these involving hardware, fracture, delicate tissues, nerves, and tendons. This complication might turn into evident only after some time has elapsed, as swelling of fibrous tissue subsides and bone remodels. The commonest websites embody the dorsal wrist, when screws have been inserted, and the radial wrist, when a plate has been used. It can be prevented with cautious screw and plate placement and radiographic verification of their position. Loss of fracture reduction and fixation can occur, and is most typical in sufferers with osteopenic bone or comminuted and articular fractures. The palmar cutaneous department of the median nerve could be injured throughout incision and publicity. Avoid the nerve with a well-placed incision radial to the flexor carpi radialis and careful deep dissection. Most tendon adhesions contain the dorsal extensor tendons resulting in extrinsic extensor tightness. Flexor tendon adhesions are unusual and involve primarily the flexor pollicis longus.
Order discount kamagra soft on lineCustomized modular femoral intercalary reconstruction in a patient with Ewing sarcoma. Resection specimen and implant; cross-pin fixation is used for improved stability of the brief stems. Intraoperative view of intercalary implant; surfaces are porous for extraskeletal fixation on the prosthetic bone junctions. Salvage of multiply failed intercalary allograft with conversion to intercalary endoprosthesis. Chronic painful nonunion of distal allograft�host junction regardless of repeated surgery and vascularized fibular bone grafting. Resection of allograft with failed blade plate; cultures of allograft confirmed an infection with methicillin-sensitive Staphylococcus aureus. Use of high-dose antibiotic spacer for sterilization of soft tissues whereas preserving limb size and tissue pocket for planned reconstruction. Preparation of intramedullary canal using facing reamer and (N) use of jigs for anchor plug fixation with bicortical transfixion pins. Intraoperative view of assembled prosthesis; locking collar and screws are used to maintain proximal and distal body segments collectively. A beaded guidewire is inserted into the femur, throughout the resection bed, and into the femoral section on the far aspect of the resection bed. The beaded guidewire is partially pulled out and the allograft is inserted into the resection bed. The guidewire is then handed back via the allograft into the far femoral phase. A preliminary check of the bone cuts is made by manually compressing the allograft towards the host bone and inspecting bone contact and alignment. With the nail in place, a last inspection of the junctions is made and revision trimming of the allograft is performed to improve bone contact. The nail is then backtapped to shut down any gaps within the host�allograft junctions. Plate and Screw Fixation Rotation is checked either clinically or by aligning the previously positioned K-wires. Because of the extended time often required for therapeutic, two locking screws must be positioned proximally and distally. If compression has been utilized with a compression nail and the allograft is rotationally steady, no extra fixation is required. If the allograft is rotationally unstable around the nail, a short plate can be utilized with unicortical screws to improve stability. This can be positioned at one or both host�allograft junctions depending on the amount of instability. If essential, the plate is contoured to match the alignment of the femoral phase being reconstructed. A slight prebend of the plate is carried out to maximize compression of the junction on the facet opposite the plate. Allograft trimming is carried out as essential to improve bone contact and alignment. The tensioning gadget is seen proximally affixed to the host bone with a single screw with a distal hook into the final hole in the plate. Two screws are positioned by way of the plate into the allograft to prevent dislodgement. In resections resulting in very small residual host segments, massive plate fixation is in all probability not attainable. Alternatively, indirect compression screws from the host through the allograft may be used. Efforts ought to be made to get hold of circumferential muscle protection over the reconstructed bone. Splinting of the knee might improve patient comfort for the first few postoperative days. In the femur, vascularized grafts can be positioned medial or lateral, bridging across the allograft and affixed to the proximal and distal host section. In the tibia, delicate tissue constraints usually require the vascularized graft to be positioned throughout the allograft. Special locking plates designed for the proximal tibia are sometimes useful in tibial reconstructions. Careful measurement of the specimen length is important to guarantee correct choice of elements (if utilizing a modular system). Preparation of the bone canal is crucial to guarantee sufficient fixation; use of rigid instead of flexible intramedullary reamers is most well-liked to obtain greatest fit of the prosthetic stem. C-arm fluoroscopy is used to monitor the reaming course of to avoid penetration into the adjoining joint. Trial discount is carried out to check size and rotation and to be certain that reduction of the prosthesis our bodies is possible; the particular connection between the proximal and distal bodies varies depending on the implant producer. For implants with cemented stems, correct canal preparation using cement restrictors, pulsatile lavage, and packing for hemostasis is carried out before injection of cement and impaction of the stem. Final meeting of the prosthesis is carried out per implant requirements; care have to be taken to ensure that rotation is correct and that each one locking mechanisms are tightened or impacted. Supplemental bone graft, collected during reaming, is positioned on the implant�bone junction (over the porous coated surface) to present extraskeletal fixation of the implant. When needed, local rotation flaps are used to guarantee muscular coverage of the implant. Use of flaps and pores and skin grafts ought to at all times be thought of whenever tissue seems insufficient for a straightforward closure without tension. Particular consideration to resection length is necessary to ensure restoration of limb length; that is much less necessary in the higher extremity. Trial reductions are useful in ensuring proper size and rotation of the reconstruction. Marking the bone with pins earlier than resection offers useful landmarks for the reconstruction. Intramedullary fixation is stronger, offers extra protection towards late allograft fracture, and makes restoration of sagittal and coronal plate alignment simpler. Screw placement into the allograft must be minimized to decrease the danger of late fracture. Healing time in these reconstructions may be prolonged, so each effort must be made to acquire maximally secure fixation. Compression with intramedullary fixation could be obtained with numerous commercially obtainable nails. Compression with plates can be obtained with a tensioning device, clamp and pull screw, or (as a last resort) compression screws. This ought to be confirmed fluoroscopically after preliminary fixation and revision bone cuts made if essential. Use of alignment Kwires or medical comparability to the contralateral limb should be performed earlier than last fixation.
Order kamagra soft 100mg mastercardThe musculature of the axillary area varieties the borders of the compartment, together with the pectoralis major, latissimus dorsi, quick head of the biceps, and clavicle. Each type is subdivided in accordance with the status of the abductor mechanism (the deltoid muscle and rotator cuff): Abductors intact Abductors partially or completely resected Type A resections, by which the abductors are preserved, often are really helpful for high-grade spindle cell bone sarcomas that are entirely intracompartmental (ie, contained within either the proximal humerus or scapula bone). This type of resection also is beneficial for low grade-bone sarcomas, chosen metastatic carcinomas, and, often, spherical cell sarcomas. Type B resections, during which the abductors are resected, are extracompartmental resections and are the most typical kind of resection performed for high-grade spindle cell sarcomas. All six of these types of shoulder girdle resections and their indications are described briefly in the following part. The Functional Anatomic Compartment of the Shoulder Girdle Sarcomas develop locally in a centripetal manner and compress surrounding tissues (muscles) into a pseudocapsular layer. The pseudocapsular layer accommodates microscopic fingerlike projections of tumor, that are referred to as satellite nodules. A sarcoma will develop to fill the compartment in which it arises, and solely rarely will an extremely giant sarcoma lengthen beyond its compartmental borders. These muscles present the fascial borders of the compartment, a proven fact that has necessary surgical implications. A extensive resection of a bone sarcoma removes the whole tumor and pseudocapsular layer and should, due to this fact, encompass the investing muscle layers (compartmental resection). The functional compartment surrounding the proximal humerus consists of the deltoid, subscapularis and remaining rotator cuff, latissimus dorsi (more distally), brachialis, and parts of the triceps muscular tissues. Sarcomas that arise from the proximal humerus and extend beyond the cortices compress these muscle tissue into a pseudocapsular layer. The solely neurovascular constructions that enter this compartment are the axillary nerve and humeral circumflex vessels. The major neurovascular bundle (ie, brachial plexus and axillary vessels) to the higher extremity passes anterior to the subscapularis and latissimus dorsi muscular tissues. Anatomic drawing illustrating the choice for a core needle biopsy for tumors of the proximal humerus. Great care should be taken to avoid the pectoralis major muscle, the deltopectoral interval, and the axillary vessels. The deltoid is innervated by the axillary nerve posteriorly, so a portion of the anterior deltoid can be resected if needed without important compromise to the nerve. They additionally shield the pectoralis main muscle, which have to be preserved during surgical resection for soft tissue coverage. High-grade sarcomas that extend beyond the bony cortices of the proximal humerus expand the investing muscle tissue that form the compartmental borders and pseudocapsular layer. These sarcomas develop along the trail of least resistance and, therefore, are directed towards the glenoid and scapular neck by the rotator cuff and glenohumeral joint capsule. Anteriorly, the tumor is covered by the subscapularis, which bulges into and displaces the neurovascular bundle. Only not often does a very massive proximal humerus sarcoma extend past the compartmental borders. A extensive (compartmental) resection for a high-grade sarcoma must, therefore, embrace the surrounding muscles that type the pseudocapsular layer (ie, deltoid, lateral parts of the rotator cuff), the axillary nerve, humeral circumflex vessels, and the glenoid (extra-articular resection of the proximal humerus). The compartmental borders surrounding the scapular neck include the rotator cuff muscular tissues and parts of the teres major and latissimus dorsi muscle tissue. The compartment consists of the entire muscular tissues that originate on the anterior and posterior surfaces of the scapula: the subscapularis, infraspinatus, and teres muscle tissue. In most instances the deltoid is protected by the rotator cuff muscular tissues as a end result of the anatomic origin of most tumors is from the neck and body region. Similar to the proximal humerus, the rotator cuff muscle tissue are compressed right into a pseudocapsular layer by sarcomas that arise from the scapula. The head of the proximal humerus is contained within the compartment surrounding the scapula by the rotator cuff muscles. Wide resection of a high-grade scapular sarcoma should, subsequently, embody the rotator cuff and, in most situations, the humeral head. A true compartmental site consists of the muscular tissues of origin and insertion of a specific group, in addition to a significant feeding vessel and nerve. Surgically, nevertheless, this space is considered because the shoulder girdle compartment, which consists of the deltoid, the rotator cuff muscles, a portion of the pectoralis main muscle, the latissiumus dorsi, and the teres major. Selection of patients for limb-sparing surgical procedure is predicated on the anatomic location of the tumor and a thorough understanding of the natural history of sarcomas and different malignancies. Chest Wall Involvement Tumors of the shoulder girdle with large extraosseous parts sometimes could contain the chest wall, ribs, and intercostal muscle tissue. Relative contraindications might embody chest wall extension, pathologic fracture, earlier infection, lymph node involvement, or an advanced, inappropriately placed biopsy that has resulted in intensive hematoma, which has resulted in tissue contamination. Previous Resection the local recurrence rate is increased in cases in which a wide resection is tried (1) following a earlier inadequate resection across the shoulder girdle or (2) when a tumor already has recurred locally. This risk should be a consideration especially with tumors of the scapula and clavicle and of sentimental tissue tumors that involve the proximal humerus. Biopsy Site One of the commonest causes for forequarter amputation is an inappropriately placed biopsy web site that has resulted in contamination of the pectoralis muscles, neurovascular constructions, and chest wall. Infection In patients with high-grade sarcomas, limb-sparing procedures carried out in an space of an infection are extremely risky, because these sufferers should receive postoperative adjuvant chemotherapy. Vascular Involvement Fortunately, most tumors of the proximal humerus are separated from the anterior vessels by the subscapularis, latissimus dorsi, and coracobrachialis muscle tissue. It is rare for the axillary or brachial artery to be concerned with tumor, although a big gentle tissue part may trigger displacement and compression. In common, if the vessels appear to be concerned with tumor, the adjacent brachial plexus also is involved, and a limbsparing process could additionally be contraindicated. Physical examination is essential in figuring out tumor extension into the glenohumeral joint, neurovascular involvement, or tumor invasion of the chest wall. If tumor has invaded the joint, shoulder vary of motion usually is reduced, and the affected person may complain about discomfort and pain. Neurovascular involvement or compression may be advised by an abnormal neurovascular examination or by decreased or absent pulses. Nerve Involvement the three major cords of the brachial plexus comply with the artery and vein and rarely are involved with tumor. The axillary nerve could additionally be involved by neoplasm because it passes from anterior to posterior along the inferior glenohumeral joint capsule. If resection will lead to a serious practical loss and a detailed margin (increasing the danger of local recurrence), amputation must be thought of. Direct tumor extension into or encasement of the brachial plexus necessitates a forequarter amputation. Determining Tumor Resectability High-grade tumors arising from the shoulder girdle area typically are large and encroach on the neurovascular bundle.
References - Thompson GJ, Pace JM: Ectopic kidney: a review of 97 cases, Surg Gynecol Obstet 64:935, 1937.
- Teppo H and Revonta M. A follow-up study of minimally invasive lip biopsy in the diagnosis of Sjogrenis syndrome. Clin Rheumatol 2007; 26: 1099n103.
- Chuang YC, Thomas CA, Tyagi S, et al: Human urine with solifenacin intake but not tolterodine or darifenacin intake blocks detrusor overactivity, Int Urogynecol J Pelvic Floor Dysfunct 19(10):1353, 2008.
- Fischer, A. A. (1986b). Pressure threshold meter: Its use for quantification of tender spots. Archives of Physical and Medical Rehabilitation, 67, 836n838.
- Platz EA, Leitzmann MF, Visvanathan K, et al: Statin drugs and risk of advanced prostate cancer, J Natl Cancer Inst 98(24):1819n1825, 2006.
|
|