"Generic aspirin 100pills with visa, pain treatment wellness center."By: Joshua C Briscoe, MD - Medical Instructor in the Department of Psychiatry and Behavioral Sciences
- Medical Instructor in the Department of Medicine
 https://medicine.duke.edu/faculty/joshua-c-briscoe-md
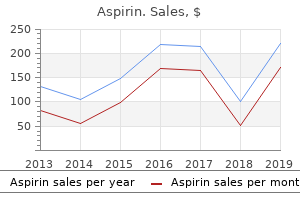
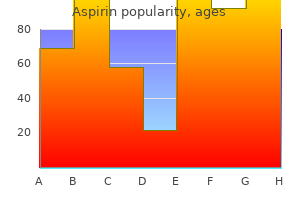
Purchase aspirin 100pills without prescriptionFormation o the brachial plexus initially entails merging o the superior and inerior pairs o roots, resulting in three trunks that every divide into anterior and posterior divisions. The fbers traversing anterior divisions innervate exors and pronators o the anterior compartments o the limb, whereas the fbers traversing posterior divisions innervate extensors and supinators o the posterior compartments o the limb. Five o the six divisions merge to orm three cords that encompass the axillary artery. Two o the three cords give rise in turn to fve nerves, and the third (lateral cord) offers rise to three nerves. In addition to the nerves arising rom the cords, more nerves come up rom other parts o the plexus. Most nerves arising rom the plexus are multisegmental, containing fbers rom two or more anterior rami o adjoining spinal nerves. Two sorts o movement occur between the arm and orearm on the elbow joint: fexion�extension and pronation�supination. The muscles perorming these movements are clearly divided into anterior and posterior groups, separated by the humerus and medial and lateral intermuscular septae. The chie action o both groups is at the elbow joint, however some muscular tissues also act at the glenohumeral joint. The superior half o the humerus offers attachments or tendons o the shoulder muscles. Muscles o Arm O the our major arm muscles, three fexors (biceps brachii, brachialis, and coracobrachialis) are within the anterior (fexor) compartment, equipped by the musculocutaneous nerve, and one extensor (triceps brachii) is in the posterior compartment, provided by the radial nerve. A distally positioned assistant to the triceps, the anconeus, also lies inside the posterior compartment. Thereore, conditioning o the triceps is o specific importance in aged or disabled persons. The two heads o the biceps arise proximally by tendinous attachments to processes o the scapula, their feshy bellies uniting just distal to the center o the arm. In either case, a single biceps tendon orms distally and attaches primarily to the radius. Although the biceps is situated in the anterior compartment o the arm, it has no attachment to the humerus. The biceps is a "three-joint muscle," crossing and capable o eecting motion at the glenohumeral, elbow, and radio-ulnar joints, though it primarily acts at the latter two. Its motion and eectiveness are markedly aected by the position o the elbow and orearm. When the elbow is prolonged, the biceps is an easy fexor o the orearm; however, as elbow fexion approaches 90� and extra energy is needed towards resistance, the biceps is capable o two powerul movements, depending on the place o the orearm. When the elbow is fexed close to 90� and the orearm is supinated, the biceps is most ecient in producing fexion. Alternately, when the orearm is pronated, the biceps is the first (most powerul) supinator o the orearm. The biceps barely operates as a fexor when the orearm is pronated, even against resistance. Arising rom the supraglenoid tubercle o the scapula, and crossing the pinnacle o the humerus inside the cavity o the glenohumeral joint, the rounded tendon o the long head o the biceps continues to be surrounded by synovial membrane as it descends within the intertubercular sulcus o the humerus. A broad band, the transverse humeral ligament, passes rom the lesser to the higher tubercle o the humerus and converts the intertubercular groove into a canal. Distally, the major attachment o the biceps is to the radial tuberosity via the biceps tendon. However, a triangular membranous band, the bicipital aponeurosis, runs rom (continued on p. In this dissection o the right arm, the veins have been removed, besides or the proximal half o the axillary vein. Note the courses o the musculocutaneous, median, and ulnar nerves and the brachial artery along the medial (protected) side o the arm. Their programs typically parallel the medial intermuscular septum that separates the anterior and posterior compartments within the distal two thirds o the arm. In this transverse section o the proper arm, the three heads o the triceps and the radial nerve and its companion vessels (in contact with the humerus) lie in the posterior compartment. The pectoralis main and minor muscles are reected superolaterally, and the lateral and medial cords o the brachial plexus are reected superomedially. All major vessels and nerves arising rom the medial and lateral cords o the brachial plexus (except or the musculocutaneous nerve arising rom a segment o the lateral cord) are removed. The posterior twine, ormed by the merging o the posterior divisions o all three trunks o the brachial plexus, is demonstrated. It offers rise to fve peripheral nerves, our o which supply the muscle tissue o the posterior wall o the axilla and posterior compartments o the higher limb. It attaches not directly by means o the ascia to the subcutaneous border o the ulna. The proximal half o the aponeurosis could be easily elt the place it passes obliquely over the brachial artery and median nerve. The aponeurosis aords safety or these and different buildings in the cubital ossa. It additionally helps lessen the stress o the biceps tendon on the radial tuberosity during pronation and supination o the orearm. To test the biceps brachii, the elbow joint is fexed towards resistance when the orearm is supinated. It acts throughout both slow and fast actions and in the presence or absence o resistance. Unlike the biceps, the brachialis fexes the orearm in all the coracobrachialis is an elongated muscle in the superomedial part o the arm. For instance, the musculocutaneous nerve pierces it, and the distal half o its attachment indicates the situation o the nutrient oramen o the humerus. The coracobrachialis helps fex and adduct the arm and stabilize the glenohumeral joint. Because its long head crosses the glenohumeral joint, the triceps helps stabilize the adducted glenohumeral joint by serving as a shunt muscle, resisting inerior displacement o the head o the humerus. The medial head is the workhorse o orearm extension, lively at all speeds and in the presence or absence o resistance. The lateral head is the strongest but is it recruited into exercise primarily towards resistance (Hamill and Knutzen, 2014). Just proximal to the distal attachment o the triceps is a riction-reducing subtendinous olecranon bursa, between the triceps tendon and the olecranon. Its energy ought to be comparable with the contralateral muscle, given consideration or lateral dominance (right or let handedness). The lateral head o the triceps brachii is divided and displaced to show the constructions traversing the quadrangular area and the radial nerve and prounda brachii artery. The uncovered bone o the radial groove, which is devoid o muscular attachment, separates the humeral attachments o the lateral and medial heads o the triceps. The anconeus assists the triceps in extending the orearm and tenses the capsule o the elbow joint, stopping its being pinched throughout extension. It is also mentioned to exert an abducting orce on the ulna throughout pronation o the orearm.
Order aspirin paypalPeritoneal ormations and subdivisions o peritoneal cavity: Continuities and connections between the visceral and parietal peritoneum happen where the gut enters and exits the abdominopelvic cavity. Parts o the peritoneum also occur as double olds (mesenteries and omenta, and subdivisions known as ligaments) that convey neurovascular structures and the ducts o accessory organs to and rom the viscera. As a outcome o the rotation and exuberant development o the gut throughout development, the disposition o the peritoneal cavity turns into complicated. The main part o the peritoneal cavity (greater sac) is divided by the transverse mesocolon into supracolic and inracolic compartments. A smaller part o the peritoneal cavity, the omental bursa (lesser sac) lies posterior to the abdomen, separating it rom retroperitoneal viscera on the posterior wall. The complex disposition o the peritoneal cavity determines the ow and pooling o extra (ascitic) uid occupying the peritoneal cavity throughout pathological circumstances. When the stomach cavity is opened to examine these organs, it becomes evident that the liver, stomach, and spleen almost ll the domes o the diaphragm. Because they bulge into the thoracic cage, they obtain safety rom the decrease thoracic cage. Partially protected by the lowest ribs, the right kidney is lower than the let kidney, owing to the mass o the liver on the best aspect. Overview o alimentary system, consisting o the digestive tract rom the mouth to the anus, with all o its accessory glands and organs. Sigmoid colon Descending colon Larynx Trachea Esophagus Liver Thoracic (descending) aorta Esophagus Mouth Tongue Pharynx Stomach 5 wall as ar ineriorly because the umbilicus. The at-laden higher omentum, when in its typical position, conceals virtually all o the intestine. Food passes rom the mouth and pharynx via the esophagus to the stomach, where it mixes with gastric secretions. Peristalsis, a series o ring-like contraction waves, begins around the middle o the abdomen and moves slowly toward the pylorus. It is accountable or mixing the masticated (chewed) ood mass with gastric juices and or emptying the contents o the abdomen into the duodenum. Absorption o chemical compounds occurs principally in the small gut, a coiled 5- to 6-m-long tube (shorter in lie, when tonus is present, than in the cadaver) consisting o the duodenum, jejunum, and ileum. The stomach is continuous with the duodenum, which receives the openings o the ducts rom the pancreas and liver, the most important glands o the alimentary system. The giant gut consists o the cecum (which receives the terminal part o the ileum), appendix, colon (ascending, transverse, descending, and sigmoid), rectum, and anal canal. Feces orm within the descending and sigmoid colon and accumulate within the rectum beore deecation. The esophagus, stomach, and small and large intestines represent the gastrointestinal tract and are derived rom the primordial oregut, midgut, and hindgut. The arterial supply to the belly half o the alimentary system is rom the belly aorta. The three major branches o the aorta supplying it are the celiac trunk and the superior and inerior mesenteric arteries. The three unpaired branches o the belly aorta provide, in succession, the derivatives o the oregut, midgut, and hindgut. The nutrient-rich blood rom the gastrointestinal tract and that rom the spleen, pancreas, and gallbladder all drain to the liver by way of the portal vein. The black arrow indicates the communication o the esophageal vein with the azygos (systemic) venous system. Abdominal Viscera 451 the hepatic portal vein is ormed by the union o the superior mesenteric and splenic veins. It is the principle channel o the portal venous system, which collects blood rom the abdominal part o the alimentary tract, pancreas, spleen, and most o the gallbladder and carries it to the liver. Esophagus the esophagus is a muscular tube (approximately 25 cm [10 inches] long) with a median diameter o 2 cm that conveys ood rom the pharynx to the abdomen. Diaphragmatic constriction: where it passes through the esophageal hiatus o the diaphragm, roughly 40 cm rom the incisor teeth. The esophagus ollows the curve o the vertebral column as it descends via the neck and mediastinum-the median partition o the thoracic cavity. The esophagus begins on the stage o the cricoid cartilage and descends posterior to the trachea. The transverse part o the esophagus shows the double muscular and plicated mucosal layers o its wall. A coronal section o the inerior esophagus, diaphragm, and superior stomach is shown. The phrenico-esophageal ligament connects the esophagus exibly to the diaphragm; it limits upward motion o the esophagus while permitting some movement during swallowing and respiration. The phrenic ampulla, which is seen only radiographically, is the distensible half o the esophagus superior to the diaphragm. In its superior third, the exterior layer consists o voluntary striated muscle; the inerior third consists o smooth muscle, and the center third is made up o each sorts o muscle. Food passes by way of the esophagus rapidly because o the peristaltic motion o its musculature, aided by however not depending on gravity (one can nonetheless swallow i inverted). The esophagus is hooked up to the margins o the esophageal hiatus within the diaphragm by the phrenico-esophageal ligament. This ligament permits independent movement o the diaphragm and esophagus during respiration and swallowing. Its anterior surace is roofed with peritoneum o the greater sac, steady with that masking the anterior surace o the abdomen. The posterior surace o the abdominal part o the esophagus is roofed with peritoneum o the omental bursa, steady with that overlaying the posterior surace o the abdomen. The right border o the stomach esophagus is steady with the lesser curvature o the stomach; nonetheless, its let border is separated rom the undus o the stomach by the cardial notch between the esophagus and undus. The esophagogastric junction lies to the let o the T11 vertebra on the horizontal airplane that passes via the tip o the xiphoid process. Immediately superior to this junction, the musculature o the best crus o the diaphragm orming the esophageal hiatus unctions as an extrinsic physiological inerior esophageal sphincter that contracts and relaxes, often in live performance with a variably thickened muscular coat around the cardial orice o the abdomen. Radiologic research present that ood stops here momentarily and that the sphincter mechanism is normally ecient in preventing refux o gastric contents into the esophagus. Details regarding the neurovasculature o the cervical and thoracic portions o the esophagus are supplied in Chapters 2, Back, and 9, Neck. The arterial provide o the abdominal part o the esophagus is rom the let gastric artery, a branch o the celiac trunk, and the let inerior phrenic artery. The venous drainage rom the submucosal veins o this half o the esophagus is each to the portal venous system by way of the let gastric vein. The lymphatic drainage o the belly half o the esophagus is into the let gastric lymph nodes. The esophagus is innervated by the esophageal plexus, ormed by the vagal trunks (becoming anterior and posterior gastric branches), and the thoracic sympathetic trunks through the higher (abdominopelvic) splanchnic nerves and periarterial plexuses around the let gastric and inerior phrenic arteries.
Diseases - Cutis verticis gyrata
- Noonan like syndrome
- Thalamic degeneration symmetrical infantile
- Spastic paraplegia facial cutaneous lesions
- Osteopoikilosis
- Erythermalgia
Generic aspirin 100pills with visaTendons o the lengthy fexors o the digits cross through the distal half o the orearm, wrist, and palm and proceed to the medial our ngers. The fexor digitorum supercialis fexes the center phalanges, and the fexor digitorum proundus fexes the center and distal phalanges. The ollowing dialogue offers extra particulars, beginning with the muscle tissue o the supercial and intermediate layers. The pronator teres, a usiorm muscle, is probably the most lateral o the supercial orearm fexors. I acting usually, the muscle is prominent and could be palpated on the medial margin o the cubital ossa. In the middle o the orearm, its feshy stomach is changed by a protracted, fattened tendon that becomes cord-like as it approaches the wrist. To take a look at the fexor carpi radialis, the individual is requested to fex the wrist towards resistance. It has a short belly and a long, cord-like tendon that passes supercial to the fexor retinaculum and attaches to it and the apex o the palmar aponeurosis. The tendon lies deep and barely medial to this nerve beore it passes deep to the fexor retinaculum. The ulnar nerve enters the orearm by passing between the humeral and ulnar heads o its proximal attachment. This muscle is phenomenal amongst muscle tissue o the anterior compartment, being ully innervated by the ulnar nerve. To test the fexor carpi ulnaris, the person puts the posterior side o the orearm and hand on a fat table and is then requested to fex the wrist towards resistance while the examiner palpates the muscle and its tendon. The median nerve and ulnar artery enter the orearm by passing between its humero-ulnar and radial heads. The our tendons are enclosed (along with the our tendons o the fexor digitorum proundus) in a synovial frequent fexor sheath. To test the fexor digitorum supercialis, one nger is fexed at the proximal interphalangeal joint towards resistance and the opposite three ngers are held in an extended place to inactivate the fexor digitorum proundus. The ascial aircraft between the intermediate and deep layers o muscular tissues makes up the first neurovascular airplane o the anterior (fexor�pronator) compartment; the primary neurovascular bundles exclusive to this compartment course inside it. Each tendon is capable o fexing two interphalangeal joints, the metacarpophalangeal joint and the wrist joint. The half o the muscle going to the index nger normally separates rom the rest o the muscle relatively early within the distal half o the orearm and is succesful o unbiased contraction. To take a look at the fexor digitorum proundus, the proximal interphalangeal joint is held within the extended place while the particular person attempts to fex the distal interphalangeal joint. The integrity o the median nerve in the proximal orearm could be tested by perorming this check utilizing the index nger, and that o the ulnar nerve may be assessed by utilizing the little nger. To test the fexor pollicis longus, the proximal phalanx o the thumb is held and the distal phalanx is fexed towards resistance. The pronator quadratus additionally helps the interosseous membrane hold the radius and ulna together, particularly when upward thrusts are transmitted by way of the wrist. The extensor muscular tissues are within the posterior (extensor� supinator) compartment o the orearm, and all o them are innervated by branches o the radial nerve. Muscles that stretch and abduct or adduct the hand on the wrist joint (extensor carpi radialis longus, extensor carpi radialis brevis, and extensor carpi ulnaris). Muscles that reach the medial our ngers (extensor digitorum, extensor indicis, and extensor digiti minimi). Muscles that extend or abduct the thumb (abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus). The extensor muscles o the orearm are organized anatomically into supercial and deep layers. Four o the supercial extensors (extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris) are hooked up proximally by a typical extensor tendon to the lateral epicondyle. The proximal attachment o the other two muscle tissue in the supercial group (brachioradialis and extensor carpi radialis longus) is to the lateral supraepicondylar ridge o the humerus and adjacent lateral intermuscular septum. The our fat tendons o the extensor digitorum move deep to the extensor retinaculum to the medial our ngers. The common tendons o the index and little ngers are joined on their medial sides near the knuckles by the respective tendons o the extensor indicis and extensor digiti minimi (extensors o the index and little ngers, respectively). The brachioradialis, a usiorm muscle, lies supercially on the anterolateral surace o the orearm. As talked about beforehand, the brachioradialis is outstanding among muscle tissue o the posterior (extensor) compartment in that it has rotated to the anterior side o the humerus and thus fexes the orearm on the elbow. It is especially lively throughout quick actions or in the presence o resistance during fexion o the orearm. The distal part o the tendon is covered by the abductors pollicis longus and brevis as they pass to the thumb. To check the brachioradialis, the elbow joint is fexed in opposition to resistance with the orearm within the midprone place. To test the extensor carpi radialis longus, the wrist is extended and abducted with the orearm pronated. I appearing normally, the muscle can be palpated ineroposterior to the lateral aspect o the elbow. The distal extensor tendons have been eliminated rom the dorsum o the hand without disturbing the arteries as a end result of they lie on the skeletal plane. The ascia on the posterior facet o the distal-most orearm is thickened to orm the extensor retinaculum, which is anchored on its deep side to the radius and ulna. Three outcropping muscle tissue o the thumb (star) emerge rom between the extensor carpi radialis brevis and extensor digitorum: abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus. The urrow rom which the three muscles emerge has been opened proximally to the lateral epicondyle, exposing the supinator muscle. This transverse part o the orearm shows the superfcial and deep layers o muscle tissue in the posterior compartment (pink), provided by the radial nerve, and the anterior compartment (gold), equipped by the ulnar and median nerves. Observe that the six synovial tendon sheaths (purple) occupy six osseofbrous tunnels ormed by attachments o the extensor retinaculum to the ulna and especially the radius, which give passage to 12 tendons o nine extensor muscular tissues. The tendon o the extensor digitorum to the little fnger is shared between the ring fnger and continues to the little fnger through an intertendinous connection. This barely indirect transverse part o the distal end o the orearm shows the extensor tendons traversing the six osseofbrous tunnels deep to the extensor retinaculum. The two muscular tissues act together to numerous degrees, normally as synergists to other muscles. Their synergistic action with the extensor carpi ulnaris is important in steadying the wrist throughout tight fexion o the medial our digits (clenching the st), a unction in which the longus is more active. The extensor digitorum, the principal extensor o the medial our digits, occupies much o the posterior surace o the orearm.
Generic 100pills aspirin mastercardThe vascular submucosa is especially thickened in the let lateral, proper anterolateral, and right posterolateral positions, orming anal cushions, or threshold pads, on the level o closure o the anal canal. Superior to the pectinate line, the lymphatic vessels drain deeply into the inner iliac lymph nodes and through them into the frequent iliac and lumbar lymph nodes. Vessels and nerves superior to the pectinate line are visceral; these inerior to the pectinate line are parietal or somatic. Inerior to the pectinate line, the lymphatic vessels drain supercially into the supercial inguinal lymph nodes, as does most o the perineum. The nerve supply to the anal canal superior to the pectinate line is visceral innervation rom the inerior hypogastric plexus, involving sympathetic, parasympathetic, and visceral aerent bers. Parasympathetic bers inhibit the tonus o the interior sphincter and evoke peristaltic contraction or deecation. The superior half o the anal canal, just like the rectum superior to it, is inerior to the pelvic ache line (see Table 6. All visceral aerents journey with the parasympathetic bers to spinal sensory ganglia S2�S4. Superior to the pectinate line, the anal canal is delicate solely to stretching, which evokes sensations at both the conscious and unconscious (refex) ranges. For instance, distension o the rectal ampulla inhibits (relaxes) the tonus o the internal sphincter. The nerve provide o the anal canal inerior to the pectinate line is somatic innervation derived rom the inerior anal (rectal) nerves, branches o the pudendal nerve. Thereore, this half o the anal canal is delicate to ache, contact, and temperature. Somatic eerent bers stimulate contraction o the voluntary external anal sphincter. Cystocele: Prolapse o the anterior vaginal wall involving the bladder (see the previous Clinical Box "Cystocele, Urethrocele, and Urinary Incontinence"). Enterocele: Prolapse o the higher posterior vaginal wall involving the rectovaginal pouch. It relies on specic measurements o nine dened factors, with the point o reerence being the hymenal ring. Maximum descent o the organ Treatment or pelvic organ prolapse consists of pelvic foor. Episiotomy During vaginal surgical procedure and labor, an episiotomy (surgical incision o the perineum and ineroposterior vaginal wall) could also be made to enlarge the vaginal orice, with the intention o decreasing excessive traumatic tearing o the perineum and uncontrolled jagged tears o the perineal muscle tissue. Once routinely perormed, episiotomies at the second are markedly less generally perormed in vaginal deliveries within the United States (Gabbe et al. Because the incision extends solely partially into this brous tissue, some surgeons imagine that the incision is extra likely to be sel-limiting, resisting urther tearing. Recent studies point out median episiotomies are associated with an elevated incidence o severe lacerations, associated in turn with an elevated incidence o long-term incontinence, pelvic prolapse, and anovaginal stulae. The incision is initially a median incision, which then turns laterally because it proceeds posteriorly, circumventing the perineal body and directing urther tearing away rom the anus. Fractures o the pelvic girdle, particularly these resulting rom separation o the pubic symphysis s and puboprostatic ligaments, oten cause a rupture o the intermediate part o the urethra. This injury normally results rom a orceul blow to the perineum (straddle injury), corresponding to alling on a steel beam, or, much less commonly, rom the incorrect passage (alse passage) o a transurethral catheter or device that ails to negotiate the angle o the urethra in the bulb o the penis. Rupture o the corpus spongiosum and spongy urethra leads to urine passing rom it (extravasating) into the supercial perineal space. The attachments o the perineal ascia decide the course o fow o the extravasated urine. Urine may cross into the unfastened connective tissue within the scrotum, around the penis, and, superiorly, deep to the membranous layer o subcutaneous connective tissue o the inerior anterior stomach wall. Plane of coronal sections Pelvirectal space Levator ani Obturator internus Pudendal canal Peri-anal abscess in ischio-anal fossa (A) Fistula Pectinate line Inferior transverse rectal fold Rectum Internal rectal plexus forming anal cushion External anal sphincter Starvation and Rectal Prolapse the at our bodies o the ischio-anal ossae are among the many last reserves o atty tissue to disappear with starvation. In the absence o the support offered by the ischio-anal at, rectal prolapse is relatively common. Anal Fissures; Ischio-Anal and Peri-Anal Abscesses the ischio-anal ossae are occasionally the sites o inection, which may result in the ormation o ischio-anal abscesses. Inections may attain the ischio-anal ossae in a quantity of ways: Ater cryptitis (infammation o anal sinuses). Diagnostic signs o an ischio-anal abscess are ullness and tenderness between the anus and the ischial tuberosity. A peri-anal abscess may rupture spontaneously, opening into the anal canal, rectum, or peri-anal skin. Because the ischioanal ossae communicate posteriorly by way of the deep postanal house, an abscess in one ossa might spread to the other one and orm a semicircular "horseshoe-shaped" abscess around the posterior side o the anal canal. In chronically constipated individuals, the anal valves and mucosa could additionally be torn by hard eces. An anal ssure (slit-like lesion) is usually located in the posterior midline, inerior to the anal valves. It is painul as a end result of this region is provided Perineum 645 by sensory bers o the inerior rectal nerves. A peri-anal abscess could ollow inection o an anal ssure, and the inection could unfold to the ischio-anal ossae and orm ischioanal abscesses or unfold into the pelvis and orm a pelvirectal abscess. An anal stula could result rom the unfold o an anal inection and cryptitis (infammation o an anal sinus). One end o this abnormal canal (stula) opens into the anal canal, and the other end opens into an abscess within the ischio-anal ossa or into the peri-anal skin. Hemorrhoids Internal hemorrhoids (piles) are prolapses o rectal mucosa (more specically o the "anal cushions") containing the usually dilated veins o the internal rectal venous plexus. Internal hemorrhoids outcome rom a breakdown o the muscularis mucosae, a smooth muscle layer deep to the mucosa. Internal hemorrhoids that prolapse into or via the anal canal are oten compressed by the contracted sphincters, impeding blood fow. Because o the presence o ample arteriovenous anastomoses, bleeding rom internal hemorrhoids is characteristically bright purple. External hemorrhoids are thromboses (blood clots) in the veins o the exterior rectal venous plexus and are coated by skin. Predisposing actors or hemorrhoids embody pregnancy, chronic constipation and prolonged bathroom sitting and straining, and any disorder that impedes venous return, together with increased intra-abdominal pressure. The anastomoses between the superior, center, and inerior rectal veins orm clinically essential communications between the portal and systemic venous methods. The superior rectal vein drains into the inerior mesenteric vein, whereas the center and inerior rectal veins drain by way of the systemic system into the inerior vena cava.
Buy 100pills aspirin with mastercardThe more inerior spinal (T1 by way of Co1) nerves bear the same alphanumeric designation because the vertebrae orming the superior margin o their exit (Table 2. First cervical nerves lack posterior roots in 50% o folks, and the coccygeal nerve could additionally be absent. By the top o the embryonic interval (8th week), the tail-like caudal eminence has disappeared, and the number o coccygeal vertebrae is decreased rom six to our segments. During the etal interval, the vertebral column grows aster than the spinal cord; consequently, the wire "ascends" relative to the vertebral canal. Arising rom the tip o the conus medullaris, the flum terminale descends among the many spinal nerve roots in the cauda equina. The lum terminale is the vestigial remnant o the caudal part o the spinal cord that was within the tail-like caudal eminence o the embryo. Its proximal finish (the flum terminale internum or pial half o the terminal lum) consists o vestiges o neural tissue, connective tissue, and neuroglial tissue coated by pia mater. The lum terminale perorates the inerior finish o the dural sac, gaining a layer o dura and persevering with through the sacral hiatus as the flum terminale externum (or dural half o the terminal lum, also recognized as the coccygeal ligament) to connect to the dorsum o the coccyx. The lum terminale is an anchor or the inerior end o the spinal cord and spinal meninges. The spinal dura is separated rom the periosteumcovered bone and the ligaments that orm the partitions o the vertebral canal by the epidural area. This house is occupied by the interior vertebral venous plexus embedded in a atty matrix (epidural at). The vertebral arches and the posterior aspect o the sacrum have been removed to expose the spinal cord in the vertebral canal. The spinal dural sac has also been opened to reveal the spinal twine and posterior nerve roots, the termination o the spinal twine between the L1 and the L2 vertebral stage, and the termination o the spinal dural sac at the S2 phase. Three membranes (the spinal meninges) cowl the spinal cord: dura mater, arachnoid mater, and pia mater. L5 S1 S2 S1 S3 S2 S4 Spinal sensory ganglia in dural S3 sleeves S4 S5 S5 Sacrum Filum terminale externum 2. Nerve bers are distributed to the spinal dura by the (recurrent) meningeal nerves. Note the dural sleeves extending rom the dural sac, enclosing the spinal sensory ganglia. The spinal dura orms the spinal dural sac, a long tubular sheath within the vertebral canal. The sac is anchored ineriorly to the coccyx by the lum terminale externum (coccygeal ligament). The spinal dural sac is evaginated by every pair o posterior and anterior roots as they extend laterally toward their exit rom the vertebral canal. Thus, tapering lateral extensions o the spinal dura surround each pair o posterior and anterior nerve roots as dural root sheaths, or sleeves. Bleeding into this layer creates a pathological house on the dura�arachnoid junction in which a subdural hematoma is ormed. The spinal pia additionally instantly covers the roots o the spinal nerves and the spinal blood vessels. The spinal wire is suspended within the dural sac by the lum terminale and the right and let denticulate ligaments 134 Chapter 2 Back Denticulate ligament Spinal wire (covered with pia mater) Reflected arachnoid and spinal dura mater Subarachnoid space Arachnoid mater Posterior view Posterior rootlets* Anterior roots of spinal nerve Posterior rootlets* (cut) (L. The 20�22 sawtooth-like processes attach to the inner surace o the arachnoid-lined dural sac. The most superior course of o the right and let denticulate ligaments attaches to the cranial dura instantly superior to the oramen magnum, and the inerior process extends rom the conus medullaris, passing between the T12 and the L1 nerve roots. The spinal dura and arachnoid mater have been cut up and pinned at to expose the spinal cord and denticulate ligaments between posterior and anterior spinal nerve roots. The lateral projections point out extensions o the subarachnoid house into the dural root sheaths across the spinal nerve roots. Spinal wire, anterior and posterior nerve rootlets and roots, spinal ganglia, spinal nerves, and meninges. The posterior spinal arteries generally orm anastomosing channels within the pia mater. By themselves, the anterior and posterior spinal arteries can provide only the brief superior half o the spinal cord. The circulation to much o the spinal twine depends on segmental medullary and radicular arteries operating alongside the spinal nerve roots. The anterior and posterior segmental medullary arteries are derived rom spinal branches o the ascending cervical, deep cervical, vertebral, posterior intercostal, and lumbar arteries. The segmental medullary arteries happen primarily in association with the cervical and lumbosacral enlargements, regions where the need or a good blood provide is best. The nice anterior segmental medullary artery (o Adamkiewicz), which is on the let side in about 65% o people, reinorces the circulation to two thirds o the spinal twine, including the lumbosacral enlargement. The posterior and anterior roots o the spinal nerves and their coverings are supplied by posterior and anterior radicular arteries (L. Segmental medullary arteries exchange the radicular arteries at the irregular levels at which they happen. Most radicular arteries are small and supply solely the nerve roots; however, some o them could assist with the provision o supercial components o the gray matter in the posterior and anterior horns o the spinal cord. Three longitudinal arteries provide the spinal cord: an anterior spinal artery and paired posterior spinal arteries. These arteries run longitudinally rom the medulla o the brainstem to the conus medullaris o the spinal twine. The anterior spinal artery, ormed by the union o branches o the vertebral arteries, runs ineriorly within the anterior median ssure. Sulcal arteries arise rom the anterior spinal artery and enter the spinal cord via this ssure. The sulcal arteries provide approximately two thirds o the cross-sectional space o the spinal twine (Standring, 2016). Each posterior spinal artery is a department o either the vertebral artery or the posteroinerior cerebellar artery In basic, the veins o the spinal twine have a distribution much like that o the spinal arteries. The spinal veins are organized longitudinally, communicate reely with each other, and are drained by as much as 12 anterior and posterior medullary and radicular veins. The veins o the spinal cord be a part of the inner vertebral (epidural) venous plexuses in the epidural house. The inside vertebral venous plexuses cross superiorly through the oramen magnum to communicate with dural sinuses and vertebral veins in the skull. The inner vertebral plexuses also talk with the exterior vertebral venous plexuses on the external surace o the vertebrae.
Syndromes - Fluids through a vein (by IV)
- Chemistry panel
- Infertility
- Do you have difficulty breathing?
- Respiratory symptoms
- Alcohol
- Eye movement abnormalities
- Endometriosis
- Quit smoking.
Purchase aspirin without prescriptionHorizontal mattress pledgetted sutures are placed on the degree of the annulus and anchor the posterior two-thirds of the annulus with one of the three posts of the valve mendacity posteriorly. Alternatively, electrical fibrillation can be utilized and within the absence of aortic regurgitation is properly tolerated. When the outflow patch has been dissected free the center is fibrillated at a systemic temperature of 30�32�C. A sizer is placed at the stage of the pulmonary annulus to select an applicable bioprosthesis. This has the effect of tilting the valve appropriately down into the main pulmonary artery. Attempting an aortic fashion of implantation with the sutures being tied on the outflow aspect of the sewing ring tilts the valve towards the sternum. The mitral valve has a useful delivery gadget that avoids sutures being inadvertently looped around the posts of the valve stent. Pledgetted horizontal mattress sutures are positioned across the annulus the place remnants of the pulmonary valve can usually be seen. Usually we place one of many three stent posts posteriorly so that improved clearance from the chest wall is achieved anteriorly. Thus the annular sutures are positioned via the posterior two-thirds of the stitching ring. At the extent of the prosthesis a running Prolene suture can be used to anchor the patch to the stitching ring. The Dacron patch is trimmed and is used to close the rest of the incision within the original outflow patch. However, subsequent re-replacement may be necessary to maintain practical enchancment. Progressive aortic root dilatation in adults late after repair of tetralogy of Fallot. Technical problem of transfemoral aortic valve implantation in a affected person with severe aortic regurgitation. Left ventricular endsystolic wall stress-velocity of fiber shortening relation: a load-independent index of myocardial contractility. Aortic valve restore and substitute after balloon aortic valvuloplasty in kids. Extended aortic valvuloplasty for recurrent valvular stenosis and regurgitation in youngsters. Morphologic determinants favoring surgical aortic valvuloplasty versus pulmonary autograft aortic valve alternative in kids. Pericardial leaflet extension for aortic valve restore: methods and late results. Complex aortic valve repair as a sturdy and efficient various to valve substitute in youngsters with aortic valve illness. Intermediateterm results of restore for aortic, neoaortic, and truncal valve insufficiency in kids. Aortic root replacement in children: a word of warning about valve-sparing procedures. The developmental complicated of "parachute mitral valve," supravalvular ring of left atrium, subaortic stenosis and coarctation of aorta. They concluded that younger age at the time of pulmonary valve alternative and valve oversizing in patients lower than 20 years of age at the time of pulmonary valve alternative were significant predictors of structural valve deterioration. They advised that these findings may probably affect the timing of pulmonary valve substitute and the extent of valve oversizing in babies. No statistically important difference in valve efficiency was seen between bioprosthetic valve sorts at short-term follow-up. On the contrary, they found that they perform properly and lead to a much decrease reoperation fee than has been reported after allograft usage. Congenitally bicuspid aortic valve causing extreme, pure aortic regurgitation without superimposed infective endocarditis. Quadricuspid aortic valve related to fibromuscular subaortic stenosis and aortic regurgitation treated by conservative surgery. Pathogenetic mechanisms of prolapsing aortic valve and aortic regurgitation associated with ventricular septal defect. Mechanisms of aortic valve incompetence: finite-element modeling of Marfan syndrome. Current administration of severe congenital mitral stenosis: outcomes of transcatheter and surgical remedy in 108 infants and youngsters. Left ventricular apical strategy for the surgical remedy of congenital mitral stenosis. Aortic valve-preserving procedure for enlargement of the left ventricular outflow tract and mitral annulus. Left atrialleft ventricular conduit for reduction of congenital mitral stenosis in infancy. Systemic atrioventricular conduit for extracardiac bypass of hypoplastic systemic atrioventricular valve. Mitral valve repair for congenital mitral valve stenosis in the pediatric population. Surgical repair of congenital mitral valve malformations in infancy and childhood: a single-center 36-year expertise. Surgical therapy of congenital mitral valve illness: midterm outcomes of a repairoriented coverage. Clinical course and hemodynamic observations after supraannular mitral valve substitute in infants and youngsters. Surgical reconstruction strategies for mitral valve insufficiency from lesions with restricted leaflet motion in infants and children. Toward complete assessment of mitral regurgitation utilizing cardiovascular magnetic resonance. Repair versus replacement for degenerative mitral valve disease with coexisting ischemic coronary heart illness. The long-term outcomes of commissure plication annuloplasty for congenital mitral insufficiency. Uber einen sehr seltenen Fall von lnsufficienz der Valvular tricuspidalis, bedingt durch eine angeborene hochgradige Missbildung deselben. Pulmonary valve replacement in tetralogy of Fallot: impact on survival and ventricular tachycardia. Younger age and valve oversizing are predictors of structural valve deterioration after pulmonary valve alternative in patients with tetralogy of Fallot. A new approach for replacement of the mitral valve by a semilunar valve homograft. It lies centrally deep inside the coronary heart immediately adjacent to the 2 atrioventricular valves. In many instances obstruction occurs at a number of levels and though the degree of obstruction in anybody space will not be extreme, the mixed effect of obstruction at multiple levels is clinically important.
Buy aspirin australiaDuring childbirth, contraction o the myometrium is hormonally stimulated at intervals o decreasing length to dilate the cervical os and expel the etus and placenta. The endometrium is actively concerned within the menstrual cycle, diering in structure with every stage o the cycle. The amount o muscular tissue within the cervix is markedly less than in the body o the uterus. The cervix is generally brous and is composed mainly o collagen with a small amount o easy muscle and elastin. Externally, the ligament o the ovary attaches to the uterus postero-inerior to the uterotubal junction. These two ligaments are vestiges o the ovarian gubernaculum, associated to the relocation o the gonad rom its developmental place on the posterior belly wall. The broad ligament o the uterus is a double layer o peritoneum (mesentery) that extends rom the edges o the uterus to the lateral partitions and foor o the pelvis. The two layers o the broad ligament are steady with one another at a ree edge that surrounds the uterine tube. Laterally, the peritoneum o the broad ligament is prolonged superiorly over the vessels because the suspensory ligament o the ovary. Between the layers o the broad ligament on both sides o the uterus, the ligament o the ovary lies posterosuperiorly and the round ligament o the uterus lies antero-ineriorly. The uterine tube lies in the anterosuperior ree border o the broad ligament, within a small mesentery referred to as the mesosalpinx. Similarly, the ovary lies inside a small mesentery known as the mesovarium on the posterior facet o the broad ligament. The largest half o the broad ligament, inerior to the mesosalpinx and mesovarium, which serves as a mesentery or the uterus itsel, is the mesometrium. The principal helps o the uterus holding it on this place are both passive and active or dynamic. Its tone throughout sitting and standing and active contraction during periods o increased intra-abdominal stress (sneezing, coughing, etc. Passive help o the uterus is provided by its position-the way by which the normally anteverted and antefexed uterus rests on high o the bladder. The cervix is the least cellular half o the uterus as a end result of o the passive assist provided by connected condensations o endopelvic ascia (ligaments), which can additionally comprise smooth muscle. Together, these passive and lively helps keep the uterus centered within the pelvic cavity and resist the tendency or the uterus to all or be pushed via the vagina (see the Clinical Box "Disposition o Uterus"). The disposition o the uterus is demonstrated in situ (A) and in isolation (B) in median sections. The two major elements o the uterus, the physique and cervix, are separated by the isthmus. Knowledge o urther subdivisions o the principle components is particularly essential, or instance, or describing the situation o tumors and websites o attachment o the placenta and contemplating the results. Note in (A) and (C) that the axes o the urethra and vagina are parallel, and the urethra is adherent to the anterior vaginal wall. A transverse part via the inerior emale pelvic organs as they penetrate the pelvic oor through the urogenital hiatus (the gap between the best and the let sides o the levator ani) demonstrates the standard disposition o the nondistended lumina. The peritoneum is refected anteriorly rom the uterus onto the bladder and posteriorly over the posterior part o the ornix o the vagina to the rectum. Anteriorly, the uterine physique is separated rom the urinary bladder by the vesico-uterine pouch, where the peritoneum is refected rom the uterus onto the posterior margin o the superior surace o the bladder. Posteriorly, the uterine body and supravaginal part o the cervix are separated rom the sigmoid colon by a layer o peritoneum and the peritoneal cavity and rom the rectum by the recto-uterine pouch. In the transition between the 2 ligaments, the ureters run anteriorly slightly superior to the lateral half o the vaginal ornix and inerior to the uterine arteries, often approximately 2 cm lateral to the supravaginal part o the cervix. The blood provide o the uterus derives primarily rom the uterine arteries, with potential collateral provide rom the ovarian arteries. The uterine veins enter the broad ligaments with the arteries and orm a uterine venous plexus on both sides o the cervix. Temporary retroversion and retroexion end result when a ully distended urinary bladder quickly retroverts the uterus and decreases its angle o exion. The vaginal orice, exterior urethral orice, and ducts o the greater and lesser vestibular glands open into the vestibule o the vagina, the clet between the labia minora. The supravaginal part o the cervix is related to the bladder and is separated rom it by only brous connective tissue. Posteriorly: the recto-uterine pouch containing loops o small gut and the anterior surace o rectum. Only the visceral pelvic ascia uniting the rectum and uterus right here resists increased intra-abdominal strain. Laterally: the peritoneal broad ligament fanking the uterine physique and the ascial cardinal ligaments on every the vagina is normally collapsed. The vaginal orice is often collapsed towards the midline so that its lateral walls are in contact on all sides o an anteroposterior slit. The vagina lies posterior to the urinary bladder and urethra, the latter projecting alongside the midline o its inerior anterior wall. The vagina lies anterior to the rectum, passing between the medial margins o the levator ani (puborectalis) muscle tissue. The vaginal ornix, the recess across the cervix, has anterior, posterior, and lateral parts. The posterior vaginal ornix is the deepest part and is closely associated to the recto-uterine pouch. Four muscular tissues compress the vagina, acting as sphincters: pubovaginalis, external urethral sphincter, urethrovaginal sphincter, and bulbospongiosus. The peritoneum is unbroken, lining the pelvic cavity and masking the superior facet o the bladder, undus and body o uterus, and much o the rectum. In this supine cadaver, the uterine tube and mesosalpinx on both sides are hanging down, obscuring the ovaries rom view. The spherical ligament o the uterus ollows the same subperitoneal course as the ductus deerens o the male. The arteries supplying the middle Pubovaginalis Pubovesicalis Rectovesicalis Vagina Bladder Rectum Coccyx and inerior parts o the vagina derive rom the vaginal and inner pudendal arteries. The vaginal veins orm vaginal venous plexuses along the sides o the vagina and throughout the vaginal mucosa. These veins are continuous with the uterine venous plexus because the uterovaginal venous plexus and drain into the inner iliac veins through the uterine vein. Only the inerior one th to one quarter o the vagina is somatic in phrases o innervation.
Buy aspirin with american expressThe anastomosis to the right ventricle is supplemented with a hood of autologous pericardium. The proven truth that numerous surgical approaches were described within the first a long time of cardiac surgical procedure suggests that outcomes till the final decade have been unsatisfactory. In 1969, Waldhausen and colleagues84 described the usage of the Glenn shunt to alleviate bronchial obstruction. Litwin and colleagues87 described an innovative process in which the left pulmonary artery was faraway from the mediastinum and changed anterior to the ascending aorta utilizing a tubular prosthetic interposition graft. Layton and associates88 reported profitable use of a valved homograft in two teenage patients in 1972. Fate of the pericardial monocusp pulmonary valve for proper ventricular outflow tract reconstruction. Reliability of Doppler color circulate mapping in the identification and localization of a number of ventricular septal defects. Effectively, a Lecompte maneuver is performed to bring the right pulmonary artery anterior to the ascending aorta. Not all facilities agree that homograft substitute of the central pulmonary arteries is necessary even for symptomatic infants. The operative survival charges at 1, 5, and 10 years were eighty three, eighty, and 78%, respectively. Risk components for operative mortality by multivariate analysis have been the presence of respiratory distress (p = zero. In patients with respiratory distress, survival with homograft replacement of the central pulmonary arteries was 73 versus 41% with different methods (p = 0. There have been no vital differences in freedom from reintervention charges among the surgical teams (p = 0. Anomalous left coronary artery from the best pulmonary artery with aortic fusion. Cerebral metabolic recovery from deep hypothermic circulatory arrest after therapy with arginine and nitro-arginine methyl ester. Cognitive perform and age at restore of transposition of the great arteries in youngsters. Primary repair minimizing the use of conduits in neonates and infants with tetralogy or double-outlet right ventricle and anomalous coronary arteries. Anastomose zwischen System- und Lungenarterie mit Hilfe von Kunststoffprothesen bei Cyanotischen Herzvitien. Surgery of pulmonary stenosis (a case by which pulmonary valve was successfully divided). Intracardiac surgical procedure with the assist of a mechanical pump-oxygenator system (Gibbon type): report of eight cases. Indikationsstellung und operative technik fur die korrektur der Fallotschen tetralogy. Intramural residual interventricular defects after repair of conotruncal malformations. Valved homograft alternative of aneurysmal pulmonary arteries for severely symptomatic absent pulmonary valve syndrome. Surgical therapy of absent pulmonary valve syndrome in infants: relief of bronchial obstruction. Congenital absence of the pulmonary valve: report of eight instances with evaluation of the literature. Surgical therapy of absent pulmonary valve syndrome related to bronchial obstruction. Pulmonary homograft monocusp reconstruction of the right ventricular outflow tract: outcomes to the intermediate term. The syndrome of absent pulmonary valve and ventricular septal defects anatomical options and embryological indications. In untreated patients with transposition and intact ventricular septum, demise happens early in infancy, generally following ductal closure at a quantity of days of age. Not surprisingly, therefore, there were many makes an attempt within the early years of open coronary heart surgery in the 1950s to undertake surgical correction for these unlucky blue infants. However, it was not until the late 1980s that anatomical correction within the type of the arterial switch procedure grew to become the standard of care. Balloon atrial septostomy, launched by Rashkind in Philadelphia,1 was one of the first broadly applied interventional catheter techniques. The embryology of the conotruncal malformations is described in greater element in Chapter 28, DoubleOutlet Right Ventricle. This results in fibrous continuity between the pulmonary and mitral valves, a hallmark of transposition. With a d-loop the ventricles lie of their ordinary relationship with the morphological left ventricle on the left and the morphological proper ventricle anterior on the right. In contrast, levo or l-loop transposition (congenitally corrected transposition) has a wholly different pathophysiology relative to d-loop transposition (see Chapter 33, Congenitally Corrected Transposition of the Great Arteries). Embryology of thE Coronary artEriEs in D-transposition the coronary circulation develops in an analogous fashion to the pulmonary arterial and pulmonary venous circulation. For example, the distal pulmonary venous system is derived from 371 372 Comprehensive Surgical Management of Congenital Heart Disease, Second Edition the original systemic venous system and invests the primitive foregut because it buds to type the primitive bronchi and, subsequently, the lungs. The unique communications of the pulmonary veins with the systemic veins resorb via a system of programmed cell dying just like apoptosis. This resorption occurs when communication has been established with the primordial pulmonary vein which buds from the posterior floor of the left atrium. Failure of the pulmonary bud to link with the venous advanced results in persistence of the systemic venous connection and hence whole anomalous pulmonary venous connection. In an analogous trend, the proximal primary coronary arteries arise as buds within the sinuses of Valsalva (usually the aortic but typically the pulmonary). These buds should fuse with a primitive vascular plexus that types from angioblasts in the mesoderm of the developing coronary heart tube. As Van Praagh has pointed out,5 the very name coronary artery reflects their circular course at the atrioventricular septum (corona = crown (Latin)). Each ventricle, proper and left, has its own distinct and completely different coronary arterial pattern. Similarly, the best major coronary artery passes directly from the closest sinus to the right-sided atrioventricular groove. In addition to the various variations in the connections of the main coronary trunk into the sinuses of Valsalva, there could be anomalies of the coronary buds themselves. This may end up in coronary ostial atresia, coronary ostial stenoses, indirect origin of the coronary ostium, and intramural coronary arteries. One of the most important distinguishing features of transposition is that the aortic valve is lifted away from the other three valves of the center by an infundibulum or conus. In hearts with d-loop transposition the pulmonary valve is in fibrous continuity with the mitral valve in the identical method that the aortic valve is in fibrous continuity with the mitral valve when the nice vessels are usually associated. An important effect of the subaortic conus in d-transposition is that the aortic valve lies at a higher stage than the pulmonary valve. The ascending aorta often lies instantly anterior to the main pulmonary artery or barely to the best (S,D,D).
Quality 100pills aspirinIt can be found in association with a quantity of different anomalies or sometimes be isolated. Surgical administration is indicated if the left to right shunt is calculated to be larger than 1. It may be essential to undertake catheterization to quantitate the diploma of shunting. The ascending vertical vein is split just under its junction with the left innominate vein. It is partially filleted open and is anastomosed to the base of the left atrial appendage which is opened longitudinally. Alternative strategies could additionally be applied for different forms of partial anomalous pulmonary venous connection. Scimitar Syndrome the arterial blood provide to the proper lung should be rigorously defined preoperatively. Pursestringing can lead to subsequent issues with growth associated narrowing of the pulmonary venous pathway. However, there was a relatively excessive incidence of postoperative pericardial effusions and postpericardiotomy syndrome. A comprehensive prospective evaluation of both intraoperative course and postoperative course was undertaken. Postoperative comparisons included ache scores at 6, 12, and 24 hours, frequency of emesis, analgesic requirements, respiratory price and gas change, and size of intensive care unit and total hospital keep. No significant variations had been identified between the mini- and full sternotomy approaches. Only improved cosmesis was recognized as a bonus for the mini-sternotomy method. The authors additionally concluded that the mini-sternotomy strategy leads to a cosmetically superior end result for the affected person with out compromising security. The function of thoracoscopic and robotic surgical strategies proceed to be explored, significantly in Asia the place the high value of gadget closure has slowed the introduction of this system. Innovative image-guided strategies that make use of new fixation strategies for patch closure have been described. The mean age of the sufferers on the time of surgery was 20 years reflecting the truth that many of those patients had been postpubertal. The problem of predicting the submammary fold in prepubertal patients is a crucial one. No procedure required conversion to a full sternotomy and no cannulation try was deserted for an alternate website. Cross-clamp and cardiopulmonary bypass instances have been equivalent to a concurrent group of sufferers who underwent a full sternotomy. Further particulars relating to the postoperative recovery of sufferers after mini-sternotomy have been documented in a paper by Laussen et al. Nineteen of the sufferers had surgical repair and forty three had closure with an Amplatzer gadget. None of the patients receiving devices required management in the intensive care unit or transfusion with blood products. The median values for postoperative pain rating, analgesia use, and convalescence time were greater for surgical patients. A whole of 442 sufferers had been assigned to system closure and 154 sufferers to surgery. There were differences between the groups together with the age at the time of the process and the scale of the defect. The process was unsuccessful in 4% of the catheter assigned group and none of the surgical group. The authors concluded that there were no statistical variations within the success rates of sufferers in whom the process could probably be completed although the complication fee was decrease and size of hospital keep was shorter for device closure. In 11% of sufferers, the try and close the defect with a device was unsuccessful. However, the time spent in hospital and away from work or school was shorter for the system group. Transcatheter closure utilizing the Amplatzer device has fewer short-term issues, avoidance of cardioplegia and cardiopulmonary bypass, shorter hospitalization, decreased want for blood merchandise and fewer patient discomfort. There had been essential differences between the two groups including the age at the time of assessment. Patients in the gadget group had been smaller on the time of closure and had smaller defects. However, there have been some exams by which surgical patients performed better than the system patients. The solely bypass-related variable that had any pattern toward significance was lowest hematocrit. These surgical patients were operated on in a timeframe when hematocrits as little as 13% had been tolerated and not occasionally occurred because of bigger priming volumes and fewer subtle circuits than can be found at present. Three patients required emergency surgery, together with one patient for hemopericardium with tamponade due to late cardiac perforation. The total 30-year actuarial survival was 74% in contrast with 85% amongst matched controls. However, amongst sufferers within the younger two quartiles, there have been no differences in survival relative to controls, namely, 97 and 93%. When restore was carried out in older patients, late cardiac failure, stroke, and atrial fibrillation had been significantly extra frequent. The authors concluded that surgical closure was superior to medical treatment in lowering total mortality and cardiovascular events. Out of those forty patients, 26 underwent surgical closure and 14 received medical remedy. All four surgically treated patients with a complete pulmonary resistance of higher than 15 units/m2 died. However, 11 of thirteen infants had related cardiac malformations and 9 had massive systemic arterial collateral vessels to the best lung. Seven patients had anomalies involving the left side of the guts, significantly hypoplasia of the left heart or aorta and 6 of those patients died. The authors concluded that the presence of pulmonary hypertension in infancy considerably elevated the chance of death or severe issues. Similar findings have been reported by the European Congenital Heart Surgeons Association who described the results of surgical procedure for 68 sufferers with Scimitar syndrome. Minimal access strategy for the repair of atrial septal defect: the initial one hundred thirty five sufferers. A 5-year expertise with surgical restore of atrial septal defect employing limited publicity. Repair of atrial septal defect through a proper posterolateral thoracotomy: a cosmetic method for female sufferers.
Buy aspirin 100pills overnight deliveryThe at bodies provide supportive packing that may be compressed or pushed apart to allow the momentary descent and growth o the anal canal or vagina or passage o eces or a etus. Anal canal: the anal canal is the terminal part o both the large intestine and the digestive tract, the anus being the external outlet. Closure (and thus ecal continence) is maintained by the coordinated motion o the involuntary inside and voluntary external anal sphincters. The sympathetically stimulated tonus o the inner sphincter maintains closure, except throughout illing o the rectal ampulla and when inhibited throughout a parasympathetically stimulated peristaltic contraction o the rectum. During these moments, closure is maintained (unless deecation is permitted) by voluntary contraction o the puborectalis and external anal sphincter. Internally, the pectinate line demarcates the transition rom visceral to somatic neurovascular supply and drainage. The anal canal is surrounded by supericial and deep venous plexuses, the veins o which usually have a varicose look. Thromboses within the supericial plexus and mucosal prolapse, together with parts o the deep plexus, constitute painul exterior and insensitive inside hemorrhoids, respectively. The intramural and prostatic components are described with the pelvis (earlier on this chapter). Details regarding all our elements o the male urethra are provided and in contrast in Table 6. The intermediate (membranous) half o the urethra begins on the apex o the prostate and traverses the deep perineal pouch, surrounded by the external urethral sphincter. It then penetrates the perineal membrane, ending because the urethra enters the bulb o the penis. Posterolateral to this part o the urethra are the small bulbo-urethral glands and their slender ducts, which open into the proximal part o the spongy urethra in the bulb o the penis. The spongy (penile) urethra begins on the distal finish o the intermediate half o the urethra and ends on the male external urethral orifce, which is slightly narrower than any o the other elements o the urethra. On all sides, the slender ducts o the bulbo-urethral glands open into the proximal part o the spongy urethra; the orices o these ducts are extraordinarily small. There are also many minute openings o the ducts o mucus-secreting urethral glands into the spongy urethra. The arterial supply o the intermediate and spongy components o the urethra is rom branches o the dorsal artery o the penis. Lymphatic vessels rom the intermediate part o the urethra drain primarily into the interior iliac lymph nodes (Table 6. The innervation o the intermediate part o the urethra is similar as that o the prostatic part: autonomic (eerent) innervation through the prostatic nerve plexus, arising rom the inerior hypogastric plexus. The sympathetic innervation is rom the lumbar spinal cord levels by way of the lumbar splanchnic nerves, and the parasympathetic innervation is rom the sacral levels through the pelvic splanchnic nerves. The visceral aerent bers ollow the parasympathetic bers retrogradely to sacral spinal sensory ganglia. The dorsal nerve o the penis, a department o the pudendal nerve, supplies somatic innervation o the spongy part o the urethra. The bilateral embryonic ormation o the scrotum is indicated by the midline scrotal raphe. The urethra has our parts: the vesicular half (in the bladder neck), the prostatic urethra, the intermediate part (membranous urethra), and the spongy (cavernous) urethra. The ducts o the bulbo-urethral glands open into the proximal half o the spongy urethra. Internally, deep to the scrotal raphe, the scrotum is split into two compartments, one or every testis, by a prolongation o the dartos ascia, the septum o the scrotum. The testes and epididymides and their coverings are described with the abdomen (see Chapter 5, Abdomen). Anterior scrotal arteries, terminal branches o the exterior pudendal arteries (rom the emoral artery), provide the anterior side o the scrotum. Posterior scrotal arteries, terminal branches o the supercial perineal branches o the interior pudendal arteries, supply the posterior aspect. The scrotum additionally receives branches rom the cremasteric arteries (branches o the inerior epigastric arteries). Lymphatic vessels rom the scrotum carry lymph to the supercial inguinal lymph nodes (Table 6. The anterior aspect o the scrotum is supplied by derivatives o the lumbar plexus: anterior scrotal nerves, derived rom the ilio-inguinal nerve, and the genital department o the genitoemoral nerve (Table 6. The posterior aspect o the scrotum is provided by derivatives o the sacral plexus: posterior scrotal nerves, branches o the supercial perineal branches o the pudendal nerve, and the perineal branch o the posterior cutaneous nerve o thigh. Sympathetic bers conveyed by these nerves help in the thermoregulation o the testes, stimulating contraction o the graceful dartos muscle in response to cold or stimulating the scrotal sweat glands while inhibiting contraction o the dartos muscle in response to extreme heat. It consists o three cylindrical cavernous bodies o erectile tissue: the paired corpora cavernosa dorsally and the one corpus spongiosum ventrally. In the anatomical place, the penis is erect; when the penis is faccid, its dorsum is directed anteriorly. Supercial to the outer overlaying is the deep ascia o the penis (Buck ascia), the continuation o the deep perineal ascia that orms a robust membranous overlaying or the corpora cavernosa and corpus spongiosum, binding them collectively. The corpora cavernosa are used with one another in the median plane, besides posteriorly the place they separate to orm the crura o the penis. Internally, the cavernous tissue o the corpora is separated (usually incompletely) by the septum penis. The scrotum is divided into right and let halves by the cutaneous scrotal raphe, which is steady with the penile and perineal raphes. The dorsum o the circumcised penis and the anterior surace o the scrotum are shown. The pores and skin o the penis extends distally as the prepuce, overlapping the neck and corona o the glans penis. The root o the penis, the hooked up part, consists o the crura, bulb, and ischiocavernosus and bulbospongiosus muscular tissues. The root is positioned in the supercial perineal pouch, between the perineal membrane superiorly and the deep perineal ascia ineriorly. Each crus is connected to the inerior half o the internal surace o the corresponding ischial ramus. The enlarged posterior part o the bulb o the penis is penetrated superiorly by the urethra, persevering with rom its intermediate part. Except or a ew bers o the bulbospongiosus muscle near the basis o the penis and the ischiocavernosus muscle that embrace the crura, the physique o the penis has no muscle tissue. The penis consists o skinny pores and skin, connective tissue, blood and lymphatic vessels, ascia, the corpora cavernosa, and corpus spongiosum containing the spongy urethra. Distally, the corpus spongiosum expands to orm the conical glans penis, or head o the penis. The margin o the glans projects beyond the ends o the corpora cavernosa to orm the corona o the glans.
References - Snyder, M., & Wieland, J. (2003). Complementary and alternative therapies: What is their place in the management of chronic pain? Nursing Clinics of North America, 38, 495n508.
- Monti PR, Lara RC, Dutra MD, et al: New techniques for construction of efferent conduits based on the Mitrofanoff principle, Urology 49:112n115, 1997.
- Meyerson M, Enders GH, Wu CL, et al: A family of human cdc2-related protein kinases, EMBO J 11:2909n2917, 1992.
|
|