"Cheap artrichine 0.5mg otc, antibiotic essentials 2015."By: Carlos A Pardo-Villamizar, M.D.
 https://www.hopkinsmedicine.org/profiles/results/directory/profile/0008959/carlos-pardo-villamizar
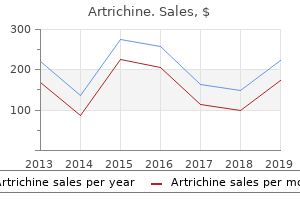
Generic artrichine 0.5 mg lineSeptal deviations, concha bullosa, and different anatomic variations that may hinder entry b. Viability of a nasoseptal flap: Prior surgical procedure or septal perforation might obviate using the flap. Examination of the ears and audiogram: Because of their close proximity to the center ear, Eustachian tube, and hearing/vestibular apparatus, petroclival lesions can produce abnormalities in hearing and steadiness. Delivers information regarding bone erosion/remodeling, osteitis, and sinusitis b. History Many lesions of the petrous apex are small benign lesions which will remain asymptomatic for years and are sometimes by the way diagnosed on imaging carried out for other causes. Videofluoroscopy If dysphagia is current preoperatively, videofluoroscopic evaluation of swallowing function should be performed. Best delineates tumor size, extent, and the intrinsic traits of the tumor b. Although not widespread for petrous apex pathology, preoperative embolization of specific pathology can lower intraoperative bleeding. It is fundamental to adapt the surgical strategy to the affected person and never the opposite way around. Individual dangers and benefits primarily based on symptoms, extent of disease, and natural historical past of the illness have to be thought of. Small lesions in asymptomatic sufferers could be followed up every 6 months with serial imaging. A multidisciplinary staff with an experienced Otolaryngologist and Neurosurgeon is necessary. Lesions with lateral extension and those with involvement of crucial neurovascular structures must be analyzed for an open or combined method. A line by way of the modiolus of the cochlea and the inner auditory canal (dashed white line) divides the petrous bone into an anterior and posterior compartment. Most lesions are located anterior to this line because about 10%�30% of sufferers have anterior compartment pneumatization; in distinction, the posterior petrous bone (osseous labyrinth) rarely pneumatizes. In instances the place neurovascular shunting is important, an open or combined endoscopic-assisted strategy is favored. A lateral element of the lesion could additionally be higher accessed via a lateral strategy. Patients must be informed in regards to the risks related to tumor excision, including vascular and neural damage, in addition to the potential for cranium base reconstruction and the necessity to convert to an open process. Dietary supplements similar to vitamin E, fish oil, Echinacea, aloe, and garlic extract additionally could be a source of bleeding disorders, and their use ought to be discontinued. Note how the lesion eroded the bone over the carotid and displaced from its location the paraclival and petrous segments of the interior carotid artery superiorly and laterally (red circles), making an endonasal endoscopic strategy perfect for this sort of case. Adequate blood strain is needed to preserve perfusion through the circle of Willis and the collateral circulation. Hypercapnia produces vasodilatation, while normocapnia or delicate hypocapnia minimizes bleeding and optimizes the surgical area throughout endoscopic endonasal surgery. Meticulous care with positioning is important to keep away from strain ulcers or traction on the brachial plexus with head positioning. A reverse Trendelenburg place improves hemostasis of the surgical area when compared to the supine place. If a Mayfield cranium clamp system is used, it ought to be positioned on the stage or above the temporal line. For patients with a historical past of continual bacterial rhinosinusitis, prior culture outcomes ought to guide perioperative antibiotic use. Blood loss have to be precisely monitored, as underestimating blood loss could result in poor fluid resuscitation with subsequent shock and organ harm. Neurophysiologic monitoring (somatosensory evoked potentials): early detection of ischemia/hypoxia before irreversible damage occurs. Electrophysiologic monitoring of cranial nerves, particularly the abducens nerve Instruments and Equipment to Have Available 1. Image guidance system: optical or electromagnetic image steerage system with stealth merge functionality 9. Hemostatic material, similar to Surgicel (Johnson & Johnson, New Brunswick, New Jersey), thrombin-soaked gelatin foam (Floseal Baxter International Inc. DuraGen (Integra Lifescience Corporation, Plainsboro, New Jersey) and Alloderm (Lifecell Corporation, Branchburg, New Jersey) can be utilized for dural reconstruction. In such cases, dissection should proceed from a medial to a lateral path, beginning at the anterior margin of the floor of the sphenoidal sinus with identification of the Vidian canal and foramen rotundum laterally. The pterygoid process is closely related to three foramina that should be identified prior to the drilling of the pterygoid plates: 1) Palatovaginal canal 2) Vidian canal 3) Foramen rotundum b. Drilling and resection of the bottom of the pterygoid plates enable entry to the inferior side of the petrous bone. Surgical Technique the surgeon must choose the best surgical hall for each particular person lesion. A 0-degree, 4-mm, rigid nasal endoscope attached to a high-definition video system is used for virtually all of the operation. Thirty-, 45-, 70-, and 90-degree endoscopes must be out there for evaluation of laterally extending lesions. If a large surgical defect is anticipated, a vascularized nasoseptal flap primarily based on the posterior nasal branch of the sphenopalatine artery is raised via electrocautery. The flap should be harvested from the contralateral facet, if the ipsilateral sphenopalatine artery is clipped during a transpterygoid method. The petrous apex may be approached by way of a bilateral paraseptal approach or a transpterygoid strategy. The whole anterior wall of the sphenoid sinus together with the intersinus septum, sphenoid rostrum, and vomer is removed with Kerrison rongeurs and high-speed drill with a 3- or 4-mm coarse diamond burr. Incomplete removing of bony edges of the anterior wall of the sphenoid and throughout the sphenoid may limit the mobility of the instruments. To attain the petrous apex, the medial aspect of the pterygoid course of and the medial pterygoid plate are exposed superior to the Eustachian tube, and the Vidian canal is identified. The palatovaginal artery can be cauterized the place it exits the pterygopalatine area. For inferior extension, a transclival method can be carried out along side this approach. For lateral extension, a transethmoidal-sphenoidal or a transethmoidal-pterygo-sphenoidal approach can be used. Left petrous apex adenocarcinoma post-resection considered with 30-degree angle scope. It could additionally be necessary to transect the dense fibrocartilage between the foramen lacerum and the eustachian tube with scissors. Transethmoidal-Pterygo-Sphenoidal Approach this permits for extra entry laterally to the inferior aspect of the petrous bone (infrapetrous approach). In addition to the bilateral transphenoidal approach, the next steps are taken: 1. The antrostomy is extended posteriorly to the extent of the pterygoid process, and the posteromedial wall of the maxillary sinus is eliminated.
Purchase artrichine 0.5 mg with mastercardThe intranasal cavity, together with the inferior and middle turbinates, basal lamella, and anterior wall of the sphenoid sinus medial to the center turbinate are infiltrated with 1% xylocaine with 1:100,000 epinephrine, and zero. Fellowship: the top and neck surgeon must be educated in both open and endoscopic approaches to the anterior cranial base. The staff have to be prepared to control huge bleeding, though uncommon, from the carotid artery. Fluid resuscitation: Communication with anesthesiology on blood loss and size of surgery is mandatory for applicable management of fluid and blood products during surgery to stop hypotension and underperfusion of the mind. Preoperative and scheduled dosing of antiseizure medications corresponding to levetiracetam may be useful in certain circumstances. Scalp and flap necrosis: Protection of the supraorbital arteries and hydration of the pericranial flap with saline-soaked gauze will restrict harm. Facial nerve damage: the temporal branches are in danger with elevation of the scalp. Orbital harm: Inadvertent harm to the ophthalmic artery can result in blindness. Vancomycin if the affected person is allergic to penicillin or cephalosporins Monitoring None needed Instruments and Equipment to Have Available 1. Various handpieces and drill bit sizes are available for open, craniotomy, and cranium base entry. Endoscopic pistol-grip Hemoclip applier Surgical Technique Bicoronal Approach � Vasoconstriction the planned incision is infiltrated with zero. Using a curved hemostat to separate the tissue layers, the lateral incision is extended to the fascia of the temporalis muscle (deep temporal fascia). The coronal scalp incision may be extended in a preauricular pores and skin crease to present extra lateral exposure. Preservation of the artery is important for sustaining the blood provide to the temporoparietal fascial flap and to the scalp in revision surgical procedure and post-radiation therapy. The pericranial flap is incised in a U-shaped style based mostly on the supraorbital and supratrochlear vessels. If publicity of the lateral orbital rim is critical, a horizontal incision is made within the outer layer of the deep temporal fascia several centimeters above the zygomatic arch. Elevation continues in this adipose layer to the zygomatic arch, thereby avoiding injury to the frontozygomatic branches of the facial nerve. If the orbital rim should be eliminated for a subfrontal method, the periorbita is elevated in a subperiosteal plane medially to the frontoethmoid suture line and laterally to the inferior orbital fissure. The temporalis muscle is elevated from the temporal bone toward the temporal fossa. A small cuff of periosteum is left at the margins to reapproximate the muscle throughout closure. Traction sutures or hooks are then used to mirror the scalp, pericranium, and temporalis muscle and secured to the surgical drapes for constant publicity. A moist laparotomy towel is placed over these tissues to keep away from desiccation and lack of tissue. Neurosurgical methods for exposure of intracranial contents are past the main target of this chapter but could additionally be found in varied textbooks on neurosurgery. Exposure permits release of the septum from the anterior cranial base, and elimination of the lamina papyracea detaches the lateral nasal wall and maxilla from the orbital roof. The pericranial flap is dissected from the galea by sharp dissection to the extent of the orbital rim. The scalp is elevated to the orbital rims with preservation of the supraorbital neurovascular bundle (arrowheads). The vascular pedicle of the pericranial flap is dependent on the supraorbital vessels (arrows). The most commonly used flap for this closure is the pericranial flap, as discussed earlier. The pericranial flap can cowl the anterior cranium base, including the cribriform plate, planum sphenoidale, fovea ethmoidalis, and orbital roof. The arc of rotation of the pericranial flap can be elevated through the use of a unilateral blood supply or incising the base of the flap. The distal edge of the flap is secured to the sting of the intact dura on the posterior border of the cranium base defect. Suturing is then performed from posterior to anterior alongside the cut dural edges or periorbita to type a watertight seal. Prior to replacement of the bone grafts, all remaining mucosa inside the frontal sinuses should be eliminated so as to enable cranialization of the frontal sinus. Blunt stripping of the mucosa with a Freer elevator and then "sprucing" all edges and crevasses with a 3- to 4-mm high-speed diamond drill with continuous irrigation are recommended. This dissection is carried into the frontal recess bilaterally, and temporalis muscle plugs are used to obliterate the recess. Care should be taken to not compress the pericranial flap at the inferior fringe of the supraorbital bone. It is really helpful to remove an additional 2 to 3 mm of bone to keep away from this complication. The bone flaps are secured with titanium microplates and 3- to 4-mm self-tapping screws. Subperiosteal elevation of the frontal scalp reveals the supraorbital nerve exiting from a completely enclosed bony foramen. After resection of the neoplasm, a large defect of the anterior cranial base stays and communicates with the paranasal sinuses. Various segments of the frontal bone and supraorbital rims could additionally be eliminated to provide enough exposure of the anterior cranial base. Bone defects could additionally be coated with titanium burr-hole covers to forestall a postoperative deformity. Transcranial and Endonasal Approaches to the Anterior Cranial Base 787 positioned into the wound. The drain exit ought to be posterolateral to the bicoronal scalp incision and secured with a 2-0 Prolene suture. The scalp is then repaired in layered fashion with 3-0 Vicryl sutures to reapproximate deep tissues and staples to reapproximate the pores and skin edges. Endoscopic Approach Endoscopic methods can be utilized to strategy malignant and benign tumors of the ethmoid roof and cribriform area of the anterior cranial base. All of these strategies may be mixed with open approaches per surgeon choice. Using a headlight, roughly 10 mL of 1% lidocaine with 1:100,000 epinephrine is injected into the septum, center turbinate, uncinate process, and the anterior wall of the sphenoid sinus.
Cheap artrichine 0.5mg otcRecent studies have instructed that within the case of laryngeal cancer, the shift to nonsurgical therapies might have decreased survival. First, the rise in total survival in the research was principally attributable to the elevated survival in patients receiving radiation and no surgical procedure. It can additionally be notable that research in laryngeal and oropharyngeal carcinoma have demonstrated a survival good thing about chemoradiation remedy when compared with radiotherapy alone. Many of the surgical approaches for most cancers of the hypopharynx are related in oropharyngeal and laryngeal most cancers as well. Partial pharyngectomy (sometimes referred to as "restricted pharyngectomy") applies to both hypopharyngeal and oropharyngeal lesions. The administration of cancer of the oropharynx is roofed intimately elsewhere, but the armamentarium of surgical approaches consists of transoral, transpharyngeal, and even mixed laryngectomy/hypopharyngectomy operations. Technical nuances in these procedures are critically important when offering optimal oncologic and useful outcomes. In order to be comprehensive, a surgeon must be acquainted with all of these approaches. The authors have taken a really tough and important subject and condensed it right into a valuable reference, which is an excellent starting point. Readers are encouraged to have a look at the references to other chapters and refer backwards and forwards to the chapters that overlap with this one to maximize the academic worth and assist master the crucial components in affected person care. Induction chemotherapy plus radiation compared with surgical procedure plus radiation in sufferers with superior laryngeal cancer. Hypopharyngeal cancer incidence, therapy, and survival: temporal developments in the United States. Transoral robotic surgery for hypopharyngeal squamous cell carcinoma: 3-year oncologic and useful evaluation. Supracricoid hemilaryngopharyngectomy in sufferers with invasive squamous cell carcinoma of the pyriform sinus. Trends in chemoradiation use in elderly patients with head and neck cancer: changing remedy patterns with cetuximab. Outcomes of intensity-modulated radiotherapy versus typical radiotherapy for hypopharyngeal cancer. Tassler demonstrates the complexity of evaluating and managing most cancers of the hypopharynx. The wide selection of presenting signs and bodily signs varies from minimal to profound. Many patients current only with neck metastasis or when the cancer may be very superior. The topic is covered very comprehensively but with an try and restrict any redundancy with different related chapters on administration of various aspects of cancer of the pharynx. Regarding imaging for hypopharyngeal tumors, which of the following statements is true Which of the following is a contraindication to partial laryngectomy together with partial or total pharyngectomy How a lot pharyngeal mucosa should remain following tumor resection to have the ability to carry out direct pharyngeal closure Supraglottic hemilaryngectopharyngectomy plus radiation for the remedy of early lateral margin and pyriform sinus carcinoma. Final results of the 94-01 French Head and Neck Oncology and Radiotherapy Group randomized trial evaluating radiotherapy alone with concomitant radiochemotherapy in advanced-stage oropharynx carcinoma. The prevertebral fascia: an alternative strategy for reconstruction of the posterior wall of the hypopharynx. Role of larynx-preserving partial hypopharyngectomy with and without postoperative radiotherapy for squamous cell carcinoma of the hypopharynx. Surgical management of posterior pharyngeal wall carcinomas: practical and oncologic outcomes. A classification system for the reconstruction of vertical hemipharyngolaryngectomy for hypopharyngeal squamous cell carcinoma. Posterior pharyngeal carcinoma resection with larynx preservation and radial forearm free flap reconstruction: a preliminary report. Combined chemotherapy and radiotherapy versus surgery and postoperative radiotherapy for advanced hypopharyngeal most cancers. Kass the hypopharynx is a complex anatomic region that begins on the degree of the hyoid and terminates at the esophageal inlet. It is adjoining to , however distinct from, the larynx and is the useful conduit that carries food from the oropharynx to the esophagus. A leak not only places a free tissue reconstruction at risk but in addition leads to fistula, wound healing problems, and an infection leading to attainable carotid blowout. This will extend the postoperative care and delay oral consumption and rehabilitation of speech. Examples embrace well-circumscribed cancers of the posterior pharyngeal wall or small cancers in the pyriform sinus that may be excised together with a portion of the aryepiglottic fold. Open approaches with partial resection of the larynx can carry larger morbidity, particularly if the affected person has had prior radiation of the neck. Laryngealsparing open approaches embody a midline pharyngotomy with or without mandibulotomy, lateral pharyngotomy, and partial resection of the larynx with partial pharyngectomy. More generally, a laryngectomy is required for patients with advanced cancer at presentation or persistent cancer following chemoradiation. When the cancer extends to the cervical esophagus, a cervical or complete esophagectomy is required. A defect-oriented method could be helpful when deciding reconstructive options (Table forty nine. With small lesions that may be eliminated through a transoral method no reconstruction could also be essential, and the tissue can be left to heal by secondary intention. Unfortunately, hypopharyngeal most cancers often presents late and requires not solely resection of the hypopharynx but in addition the larynx. In basic, tumors of the hypopharynx, greater than 95% of which are squamous cell carcinoma, carry very excessive general mortality charges (65% of patients die inside 5 years of presentation). These cancers are characterised by submucosal spread with invasion of surrounding buildings that lack obstacles for spread, metastases to the neck or distant metastases at presentation, and a better price of synchronous second primary cancers. Understanding the number of surgical approaches for tumor resection can be useful when anticipating the scale of the defect required for reconstruction (Table forty nine. They can typically be divided into approaches that spare the larynx and those that require a laryngectomy. Paired pyriform sinuses (A), postcricoid mucosa (B), and posterior pharyngeal wall (C).
Order artrichine with visaRobotic surgical platforms are one other expertise that has been utilized in minimal and remote entry surgery. Robotic surgical procedure allows for enhanced visualization utilizing a three-dimensional high-definition endoscopic digital camera system, wristed instrumentation, and tremor reducing know-how. Typically, the surgeon sits at a console that controls the robotic instrumentation, and a bedside cart incorporates the robotic arms and endoscope. The preliminary application in head and neck surgery for minimally invasive surgery, both endoscopic and robotic, was in parathyroid and thyroid surgical procedure. The first description of endoscopic excision of the submandibular gland in humans was described by Guyot, when he determined the feasibility in human cadavers. Robotic method to the submandibular gland via a retroauricular incision has additionally been described. Note the presence or absence of saliva and consistency (purulent, turbid, normal). Contraindications � Previous neck surgery � Metastases to the cervical lymph nodes with proof of extracapsular extension on imaging � History of radiation to the neck. Since these techniques approach from distant places and unusual angles, the surgeon can simply become disoriented. It is essential to know the anatomic relationships and dissection planes, so the operation may be carried out effectively and safely with out elevated problems. As dissection is carried alongside the posterior stomach of the digastric, identify and ligate the proximal facial artery with double hemoclips. If eradicating the gland for sialolithiasis, make positive that the calculus is included within the duct earlier than ligation. There are three steps to the surgical procedure: elevation of the flap, bedside direct visualization, and robotic visualization. Continue dissection to the midline anteriorly, clavicle inferiorly, and inferior mandible because the upper restrict. Example of the publicity gained via a retroauricular incision for removing of a branchial cleft cyst that has been excised. Dissect the fibroadipose tissue anteriorly over the deep cervical fascia and cervical rootlets. Dissect onto the ground of level V preserving the transverse cervical vessels and brachial plexus. If the supraclavicular nerves require sacrifice distally, make certain the proximal transection on the cervical rootlets preserves the contributions to the phrenic nerve. Next, retract the submandibular gland inferiorly and ligate the facial artery and vein distally at the inferior border of the mandible. The marginal mandibular nerve ought to be protected presently since it has already been recognized and swept over the mandible. When dissecting medially alongside the carotid sheath, use the Harmonic scalpel and hemoclips to divide the tissue inferiorly to prevent a chyle leak. Dissect in a suprafascial airplane above the pectoralis main muscle to the sternal notch and clavicle. Example of an inconspicuous healed retroauricular incision at 3 months postoperative. Positioning for the robotic transaxillary approach for thyroidectomy or neck dissection. The ProGrasp forcep should be positioned simply to the right of the camera however on the superior-most portion of the working house. The Maryland dissector is positioned as far to the left of the camera as potential and the Harmonic shears are as far to the right of the digital camera as potential. Once this airplane is developed, the fibroadipose tissue may be dissected off the carotid sheath in a medial to lateral trend. Take care to not harm the thoracic duct, phrenic nerve, and transverse cervical vessels. Dissection proceeds over the carotid sheath medially and cervical rootlets laterally. A hemostat clamp is placed over the puncture website to forestall additional leakage and to help with manipulation of the cyst. Endoscopic and Robotic Applications to Neck Surgery 503 � Dissect along the cyst wall circumferentially beneath endoscopic magnification. Editorial Comment Distant access surgery offers an choice for surgical entry for sufferers in search of a more beauty option for a visual scar on the neck. While distant entry neck surgical procedure (endoscopic and robotic) have been proven to be safe, these procedures are longer and require experience available in few facilities. In addition, sure issues are launched to the traditional procedure that are unique to distant entry surgical procedure, similar to conversions to open approaches, brachial plexus neuropathy due to arm place for transaxillary surgical procedure and hypercarbia, and subcutaneous emphysema associated with insufflation methods. The surgical anatomy and strategy for these procedures could be challenging for even skilled head and neck surgeons. Endoscopic subtotal parathyroidectomy in sufferers with main hyperparathyroidism. Minimally invasive video-assisted thyroidectomy for papillary carcinoma: a potential study of its completeness. Multicenter study of robotic thyroidectomy: short-term postoperative outcomes and surgeon ergonomic considerations. Robotic total thyroidectomy with modified radical neck dissection through unilateral retroauricular approach. Minimally invasive endoscopic resection of the submandibular gland: a brand new approach. Endoscope-assisted submandibular sialadenectomy: a new minimally invasive method to the submandibular gland. Minimally invasive video-assisted submandibular sialadenectomy: surgical approach and outcomes from two establishments. There was no significant difference within the total number of lymph nodes retrieved or in the rates of complications. Another research in contrast the two approaches retrospectively in patients with oral cavity most cancers. This again demonstrated no difference in the complication price or number of lymph nodes removed. Neither group had any evidence of regional recurrence, but the follow-up time was restricted to 6 months. Lastly, a North American�based group reported on their experience with robotic lateral neck dissection in sufferers with head and neck mucosal malignancies. In all the studies listed above, the robotic method was associated with significantly longer operative times than the normal approach. Which of the following is a contraindication to robotic and endoscopic neck surgery
Buy artrichine with a mastercardAerodigestive tract invasion by well-differentiated thyroid carcinoma: analysis, administration, prognosis, and biology. Extrathyroid spread in papillary carcinoma of the thyroid: clinicopathological and prognostic examine. Surgical administration of tracheal shaving for papillary thyroid carcinoma with tracheal invasion. Pathologic staging of papillary carcinoma of the thyroid with airway invasion based mostly on the anatomic manner of extension to the trachea: a clinicopathologic research based mostly on 22 sufferers who underwent thyroidectomy and airway resection. Cartilage-shaving procedure for the management of tracheal cartilage invasion by thyroid carcinoma. What is the most effective imaging modality to consider extent and location of tumor invasion into surrounding buildings What surgical choice allows the best probability of local control in tracheal invasion Surgery for sufferers with thyroid carcinoma invading the trachea: circumferential sleeve resection adopted by end-to-end anastomosis. The importance of preoperative laryngoscopy in sufferers undergoing thyroidectomy: voice, vocal twine operate, and the preoperative detection of invasive thyroid malignancy. E-cadherin loss rather than betacatenin alterations is a typical feature of poorly differentiated thyroid carcinomas. Management of invasive welldifferentiated thyroid most cancers: an American Head and Neck Society Consensus Statement. The mechanism by which this occurs is through renal tubular reabsorption, bone resorption, and formation of calcitriol from calcidiol within the renal tubular cells. The hormone is synthesized as an inactive polypeptide chain, which is then cleaved at the N-terminal within the parathyroid glands to an lively type. The half-life of the hormone ranges from 2 to four minutes, making it helpful for serologic analysis by speedy immunoassay following excision of an abnormally functioning gland. This most commonly outcomes from a single parathyroid adenoma (80% to 85%) or less frequently from four-gland hyperplasia (10% to 15%) or double adenoma (4% to 6%). However, bilateral neck exploration has the next incidence of momentary and permanent hypocalcemia, which may lead to longer hospital stays and elevated morbidity from symptomatic hypocalcemia. With the advent of improved imaging techniques and radioguided parathyroidectomy, minimally invasive methods have decreased the morbidity related to this situation and led to general higher outcomes. Preoperative imaging with a sestamibi scan has glorious sensitivity within the case of a single parathyroid adenoma. This decreased sensitivity could lead to therapy failure and topic sufferers to an additional surgical procedure. This decreases the need for bilateral neck exploration in addition to the general threat of postoperative hypocalcemia, hematoma, and recurrent laryngeal nerve harm; it also shortens the operative time. Hypocalcemia is essentially the most frequent complication following total thyroidectomy, with a reported incidence of 20% to 50%. Debilitating and everlasting hypocalcemia, though much less frequent, can still occur in close to 2% of sufferers. Historically sufferers are admitted to the hospital following whole thyroidectomy for the monitoring of hypocalcemia, since signs can happen within 24 to 48 hours and can be life threatening. A blood sample may be simply and rapidly collected from the inner jugular vein, peripheral vein, or an arterial line. Medical illness 1) Bone pain or history of pathologic fracture 2) History of renal calculi or different renal dysfunction 3) Underlying psychologic illness or melancholy 4) Generalized weakness, abdominal ache, muscle spasm b. In addition to supine positioning, proper neck extension and shoulder-roll placement are particularly essential in dissection of the lower neck. Perioperative Antibiotic Prophylaxis First-generation cephalosporin: We choose cefazolin 1 mg if the affected person weighs less than seventy five kg or 2 mg if the patient weighs more than that. Second-generation cephalosporin: Clindamycin if the affected person is allergic to penicillin Imaging No imaging is required. Ultrasound Thyroid ultrasound can be helpful for the localization of parathyroid adenoma; nevertheless, its utility is proscribed, particularly in the setting of thyroid nodule or multinodular goiter. Technetium-99 Sestamibi Scan the sestamibi scan has persistently been proven to be a extremely sensitive study in single parathyroid adenoma. However, in the setting of parathyroid hyperplasia or double adenoma the sensitivity significantly decreases to 30% to 44%. Its utility lies in the analysis of osteoporosis or osteopenia, conditions that may result in a pathologic fracture. In patients without any underlying bone abnormality, some high-risk patients with subclinical hyperparathyroidism can be safely observed. Monitoring None Recurrent laryngeal nerve monitor: Can be a helpful adjunct in the identification and preservation of the recurrent laryngeal nerve, especially in revision surgical procedure Instruments and Equipment to Have Available 1. The internal jugular vein lies within the carotid sheath lateral to the thyroid gland. This may be helpful in in any other case low-risk patients to decide the likelihood of symptomatic hypocalcemia in the perioperative period. Parathyroidectomy or whole parathyroidectomy; see Chapter 108 (Parathyroidectomy for Primary Hyperparathyroidism and Non-Localizing Hyperparathyroidism). Significant medical comorbidities with elevated perioperative risk Patients with important comorbidities that preclude operative intervention may be monitored for complications related to hyperparathyroidism, together with but not restricted to arrhythmias, renal disease, and pathologic fracture. Intraoperative hemorrhage from the inner jugular vein Venous thrombosis/thrombophlebitis Damage to the recurrent laryngeal nerve Devascularization of regular parathyroid tissue Preoperative Preparation 1. Discontinuation of antiplatelet medication if possible Surgical Technique � See Chapters 108 and 102 relating to surgical administration in parathyroidectomy and whole thyroidectomy. Dissection laterally from the thyroid gland results in the structures of the carotid sheath. In preparation for venipuncture, the interior jugular vein should be dissected bluntly from the carotid sheath with the assistance of a bipolar cautery. Minimally invasive radioguided parathyroidectomy Use of radiolabeled tracer in parathyroid surgery detected by the gamma probe is another helpful adjunct in minimally invasive surgical approaches to the parathyroid gland. Four-gland exploration Historically four-gland exploration was the usual for primary hyperparathyroidism. There is sadly an increased risk of complications and the necessity for repeat surgery within the event of four-gland hyperplasia. The accepted criterion is named the Miami criterion and has a sensitivity and overall accuracy of 97%. Additionally the constructive predictive worth is 99% and negative predictive value 88%. When several standards were in contrast, the Miami criterion showed significantly fewer false-negative outcomes (2. A systematic evaluate of the analysis and therapy of major hyperparathyroidism from 19952003. Validity and limits of intraoperative parathyroid hormone monitoring during minimally invasive parathyroidectomy: a 10-year expertise. Comparison of intraoperative versus postoperative parathyroid hormone levels to predict hypocalcemia earlier after total thyroidectomy.
Syndromes - Standing on one foot
- Convulsions
- Nurse practitioners
- Fainting or feeling light-headed
- Early menopause
- Diuretic medication, such as furosemide
- Immune hemolytic anemia
- Your liver function is becoming worse quickly
Order artrichine 0.5mg with mastercardSurgical Treatment with Microvascular Reconstruction of Oral and Oropharyngeal Cancer. The suprahyoid pharyngotomy method is right for all of the following tumors, except a. All oropharyngeal squamous cell carcinoma biopsy specimens ought to routinely be tested for a. What portion of the physical examination is most critical to assess for tumor extent Barium esophagram is normally a useful adjunctive imaging research in instances of suspected a. If a salivary fistula is nonhealing, which of the following must be suspected as underlying causes: a. Maxwell, Seungwon Kim A hollow viscus situated immediately posterior to the larynx, the hypopharynx is said to the oral pharynx superiorly and the cervical esophagus inferiorly. It is split into three anatomic sites: the pyriform sinuses (bilateral), the postcricoid mucosa, and the posterior pharyngeal wall. The postcricoid mucosa is the mucosa mendacity on the posterior aspect of the cricoid cartilage, which can be the anterior wall of the hypopharynx. Coordinated exercise in this laryngopharyngeal phase is important for swallowing and protecting the airway from aspiration. Squamous cell carcinoma of the hypopharynx accounts for only 3% to 5% of all head and neck squamous cell carcinomas. Family historical past of cancer of the pinnacle and neck most cancers or blood dyscrasias ought to be obtained. A full record of medications must be obtained, including using anticoagulants, antiplatelets, or herbal merchandise. Current alcohol use places the patient in danger for postoperative alcohol withdrawal. Oral cavity/oropharynx 1) A thorough examination of the oral cavity and oropharynx is important to rule out synchronous main cancers in these sufferers who usually have a historical past of heavy tobacco and alcohol consumption. Patients with poor dentition may have to have dental extractions previous to radiation therapy ideally at the time of surgical procedure. A key portion of the examination is direct fiberoptic laryngoscopy to verify the presence of a hypopharyngeal lesion, and to determine its extent. Does the cancer contain the endolarynx, post-cricoid region, or posterior pharyngeal wall If the tumor causes important obstruction of the larynx, an awake versatile fiberoptic intubation or an awake tracheostomy must be considered. Candidates for organ-preservation surgery require wonderful pulmonary operate standing. The normal approach to therapy of most cancers of the hypopharynx is either partial or total pharyngectomy, usually combined with total laryngectomy, followed by adjuvant chemoradiation. Involvement of the prevertebral fascia and/or the common carotid artery is considered to be inoperable. Common presenting indicators and signs include dysphagia, odynophagia, referred otalgia, and a mass within the neck. Has the patient been identified with most cancers of the top and neck up to now or previously been treated with radiation remedy Fixation to the prevertebral fascia or bone could be ascertained preoperatively with video fluoroscopy when fixation of the pyriform sinus is recognized during swallowing. Because most sufferers present with advanced stage cancer, the risk of distant metastases at presentation is substantial. It is crucial that these sufferers be mentioned at a multidisciplinary convention for therapy options, together with palliative care. Preoperative medical clearance, significantly with regard to cardiac and pulmonary standing 2. Laboratory exams ought to include a prealbumin and thyroidstimulating hormone as these are correctable causes of delayed wound therapeutic. Consider a gastrostomy tube if the patient is unable to swallow and is malnourished. Have any biopsy or imaging research carried out at one other hospital reviewed by in-house specialists. Extension to the apex or lateral wall of the pyriform sinus is a contraindication to this procedure. This procedure is most commonly carried out in sufferers with carcinoma of the pyriform sinus that extends to contain the larynx medially, the apex of the pyriform sinus inferiorly, or the lateral wall of the hypopharynx laterally. Cancer involving the postcricoid mucosa, superior most cancers of the posterior hypopharyngeal wall, and cancer involving the pyriform sinus with extension across the midline posteriorly require whole laryngopharyngectomy. More in depth cancers that stretch into the cervical esophagus are resected via whole laryngopharyngoesophagectomy. Antibiotic prophylaxis should target pathogens found within the higher aerodigestive tract. Monitoring Standard anesthesia protocol for major surgical procedure Instruments and Equipment to Have Available 1. The pharynx is entered superior to the hyoid bone on the facet contralateral to the cancer. Preservation of this cranial nerve is essential to useful deglutition following surgical procedure. If carotid artery involvement is suspected however not confirmed preoperatively, we propose beginning with the neck dissection on the affected aspect in the event that the case have to be aborted. Most of the cancer is confined to the intrinsic larynx; however, resection of the medial wall of the ipsilateral piriform sinus is required to get hold of a deep margin. Preservation of the contralateral piriform sinus, in addition to the ipsilateral lateral wall, will permit main closure. Care have to be taken to avoid damage to the hypoglossal nerve so that the affected person has optimum swallowing function postoperatively. Injury to the hypoglossal nerve could be prevented by identifying the nerve in the course of the neck dissection portion of the case. Once recognized laterally, the nerve could be traced medially until its relationship with the hyoid bone is clearly delineated. Lack of preoperative identification of inoperability, either by involvement of the frequent carotid artery or prevertebral fascia a. This could lead to significant hemorrhage intraoperatively, which requires immediate identification and repair. Delayed postoperative hemorrhage may be related to the displacement of a poorly secured vascular clip, a wound infection inflicting tissue breakdown, or persistent cancer. This is extra common in patients who endure a radical neck dissection, have radiated tissues, and a postoperative pharyngeal leak. Small leaks are managed conservatively by avoiding an oral diet, diverting the leak with a drain, and offering native wound care. Persistent giant leaks require returning the patient to the working room for restore and presumably local or free tissue reconstruction to prevent recurrence. Risk components that predispose to pharyngeal leak embody earlier radiotherapy and hypothyroidism.
Discount 0.5 mg artrichine mastercardAxial view of the surgical route to the pharyngoesophagus (retropharyngeal space). The retractor on the left is displacing the sternocleidomastoid muscle and the contents of the carotid sheath. Tracheoesophageal damage repaired primarily and strengthened with a strap muscle pedicle flap. In these instances, local or regional flaps may be needed, relying on the encircling tissue quality. The practitioner ought to have a low threshold for performing a tracheostomy beneath the level of tracheal harm to stop additional free air within the mediastinum. Improper neck incision placement for the extent of the defectFailure to correctly localize the fistula could result Penetrating Trauma to the Hypopharynx and Cervical Esophagus 333 6. Failure to adequately drain the area Prompt and enough drainage of the neck and prevertebral area are crucial factors affecting patient prognosis. Failure to recognize mediastinal extension of the method and drainage of the gathering can be devastating. Suction drains are preferable to a Penrose drain, as the drainage cavity typically extends below the sternum, resulting in a nondependent drain place. Consideration for gastrostomy tube placement in sufferers with complex defects requiring muscle flap repair, esophagostomy, or associated laryngotracheal restore 7. In a clean wound, with good drainage and vitamin, nearly all of salivary leaks ought to shut spontaneously within 2 weeks. Cellulitis/Abscess Due to delayed remedy, insufficient drainage, or slim antibiotic protection. Mediastinitis Due to delayed remedy, inadequate drainage, or slender antibiotic protection. Recurrent laryngeal or superior laryngeal nerve injury, which can have an effect on voice, airway, and swallowing 2. Approaching prevertebral area too medially After lateralizing the carotid sheath, the next step is to elevate the laryngopharyngeal framework off of the spine. Care must be taken to start far laterally on the spine to keep away from inadvertent injury to the pharynx or esophagus, which are often off the midline. Palpation of the nasogastric tube and blunt dissection on this space are useful techniques. Failure to freshen wound edges, invert the mucosa, or acknowledge compromised pharyngeal tissue, which may lead to delayed nonviable tissue within the suture line and hence delayed leaks the quality of the pharyngeal tissue and the closure approach (inverting the mucosal edges) are important to success. If the exploration is delayed more than 24 hours and/or the tissue has discoloration (dusky quality), the wound edges should be freshened until wholesome bleeding is seen, and secondary muscle patches must be utilized. Ischemic suture line Performing a operating suture line (particularly locking fashion) with rigidity can lead to tissue ischemia and delayed leaks. The tissues and closure have to be performed meticulously with light handling of the mucosa, enough bites of tissue, and appropriately spaced sutures to keep away from tissue ischemia. A retrospective evaluate of 70 patients revealed that the placement of a pharyngoesophageal damage did impression the outcomes of patients, in notably the successfulness of conservative management. However, 22% of the sufferers with a hypopharyngeal harm under this degree and 39% of patients with a cervical esophageal damage developed either a deep neck infection that required drainage or a postsurgical salivary fistula. They therefore concluded that injuries situated within the upper portion of the hypopharynx could be routinely managed without surgical intervention. Neck exploration and enough drainage of the deep neck areas are, nonetheless, obligatory for all penetrating accidents into the cervical esophagus and most accidents into the decrease portion of the hypopharynx. The position of the sternocleidomastoid flap for esophageal fistula repair in anterior cervical spine surgery. Improved restore of esophageal fistula complicating anterior spinal fusion: free omental flap in contrast with pectoralis main flap. Management of external penetrating accidents into the hypopharyngeal-cervical esophageal funnel. Hackman has done a superb job of reviewing the important thing points relating to the administration of penetrating trauma to the hypopharynx and cervical esophagus attributable to iatrogenic or unintended causes. As he has completely described, the administration includes not only meticulous surgical technique but also keen diagnostic analysis for different related accidents and associated medical and surgical treatments required. Some injuries are fairly delicate, and as stated in the chapter, extraordinarily cautious remark for issues is required postoperatively. All of the next are important within the administration of a pharyngoesophageal perforation, except: a. Fraioli, Andrew Tassler the hypopharynx is the inferior-most portion of the pharynx, bounded by the oropharynx superiorly and the esophagus inferiorly. The hypopharynx is intimately associated to the larynx, each anatomically and functionally. Anatomically, the hypopharynx extends from the base of the vallecula right down to the apices of the piriform sinuses and the inferior border of the cricoid cartilage. For purposes of classification, the hypopharynx is divided into three subsites: the piriform sinuses, the posterior pharyngeal wall, and the postcricoid space. The mucosa of the hypopharynx is continuous with that of the larynx, and cancers that originate in one website regularly unfold to the others. Functionally, the hypopharynx and larynx are responsible for coordinating the competing tasks of airway upkeep and deglutition. Alcohol and tobacco are sturdy danger factors, as with other cancers of the top and neck. However, following landmark studies using chemoradiation with surgical salvage for laryngeal1 and hypopharyngeal2 cancers, which showed equal survival within the surgical and nonsurgical arms, the usage of main surgical therapy of hypopharyngeal most cancers has decreased. Given the low treatment rates and high rates of functional sequelae, alternate options to laryngectomy and nonsurgical organ preservation continue to be of interest and evolve. Wound closure beneath rigidity due to inadequate mucosa will predispose to wound breakdown, fistula formation, and postoperative dysphagia as a outcome of stricture formation. Submucosal spread is frequent in hypopharyngeal cancers, and adverse margins should be confirmed by frozen section. Patients must understand that although every attempt may be made to perform partial laryngopharyngectomy, intraoperative findings or frozen part pathology may make this unimaginable. Therefore, patients should be consented for a attainable whole laryngopharyngectomy. Patients with prior radiation or chemoradiation should have pharyngeal closure performed with a vascularized flap both integrated into the remaining pharyngeal mucosa or tubed within the case of complete pharyngectomy defect. A pectoralis major flap can be utilized for closure of the anterior pharynx over remaining mucosa, however a complete pharyngeal defect with discontinuity is greatest reconstructed with free tissue switch. Cancer extension throughout the midline of the posterior hypopharyngeal wall or involving the postcricoid mucosa requires whole laryngopharyngectomy with reconstruction. A laryngopharyngectomy specimen removed for persistent disease following major chemoradiation therapy. Sore throat, blood in the saliva, weight loss, dysphagia, and odynophagia may all be symptoms of most cancers of the hypopharynx. Malnutrition may be a significant downside when sufferers present with a sophisticated stage most cancers.

Effective artrichine 0.5 mgClose or constructive margins on the resection specimen A thorough examination underneath general anesthesia is performed, including digital palpation to confirm the situation, size, and mobility of the tumor. For endophytic cancers, it may be useful to paint the surface with methylene blue because these lesions might turn into obscured when retraction is applied. The process is typically began with a 0-degree scope, with the 30-degree scope reserved if wanted for visualization. The monopolar spatula cautery is positioned ipsilateral to the tumor, and the Maryland dissector is initially positioned contralateral. The lateral tongue is slid underneath the straight edge of the retractor blade, and the slotted edge is stored medial. A small cuff of regular tongue is maintained between the tip of the retractor blade and the tumor to present room to get hold of an enough anterior margin of resection. The retractor is suspended with each chest support suspension and laterally with an endoscope holder. With the primary surgeon on the console, the assisting surgeon sits at the head of the mattress utilizing two baby Yankauer suctions to retract, suction smoke, and assist to achieve hemostasis. If cancer is present on the glossotonsillar sulcus, the constrictor muscles and the styloglossus must be resected with the specimen. A horizontal anterior incision is then made instantly beneath the tip of the retractor to permit the most cancers to fall posteriorly into the operative field. Horizontal incision on the anterior margin to permit the tumor to drop into the operative subject. Establishing the depth of resection by way of the medial margin the specimen is removed and brought to the pathology department for orientation and margin analysis. If the margins are deemed shut or constructive, methylene blue is used to ink the area of concern on the patient, and re-resection is carried out. Multiple Valsalva maneuvers are carried out, and meticulous hemostasis is obtained with electrocautery and hemoclips, as wanted. Arista absorbable hemostatic powder (Davol, Providence, Rhode Island) is applied to the resection mattress. A nasogastric tube is positioned beneath direct visualization and secured contralateral to the operative area for enteric access. If significant edema of the tongue is anticipated, sufferers may be stored intubated. This is important as a end result of irreversible compression and potential airway compromise might occur if the affected person inadvertently bites a wire-reinforced tube whereas intubated. Undercutting the most cancers at the horizontal anterior resection line as a substitute of angling the devices forward towards the hyoid bone 3. These arteries are often uncovered in the course of the resection and must be ligated at a number of positions to forestall potential main postoperative hemorrhage. In addition, ligating the lingual artery in the neck on the time of staged or concurrent neck dissection must be carried out. The resection is then carried out from medial to lateral following the beforehand made horizontal incision. It is necessary to angle the devices anteriorly in an imaginary line from the plane of the retractor blade to the hyoid as a end result of the tendency is to prematurely truncate the specimen right here. Angling the vector of the resection appropriately facilitates a wide anterior margin of muscle. At the lateral side of the base of the tongue, the lingual artery and its dorsal lingual branch shall be encountered at a depth of roughly 1 to 2 cm. If vital bleeding is encountered right here from an inadvertently transected artery, external neck stress at the higher cornu of the hyoid utilized by the bedside assistant may be helpful. If the affected person is felt to be in danger for postoperative airway compromise based mostly on the extent of most cancers resection or notable residual edema of the tongue or pharynx, she or he is often saved intubated for twenty-four to forty eight hours; otherwise he or she could also be extubated. We had previously administered intravenous dexamethasone 6 mg every 6 to 8 hours till discharge adopted by a Medrol Dose Pack upon discharge. A prophylactic nasogastric feeding tube (Dobhoff) is placed whereas the patient is in the working room for enteral entry. Most sufferers are then began on a food plan of clear liquids and advanced to a mechanical gentle food regimen as tolerated. If swallowing evaluation demonstrates significant dysphagia and/or aspiration, patients are discharged with tube feeds at house. Significant postoperative ache is anticipated after resection of the bottom of the tongue. Patients are started on a affected person controlled analgesia pump and transitioned to oral narcotics as tolerated. Nonsteroidal anti-inflammatory medication are sometimes averted within the first 2 weeks publish operative given the chance for bleeding. Patients are instructed to swish and spit with Peridex at least four times/day to preserve oral hygiene and increase consolation. Although these approaches had been utilized by some, the overwhelming majority of cancers of the bottom of the tongue had been handled with combined chemotherapy and radiation. Transoral robotic versus open surgical approaches to oropharyngeal squamous cell carcinoma by human papillomavirus standing. We routinely ligate the lingual, facial, and superior thyroid arteries preoperatively in the course of the neck dissection. In our expertise, this maneuver not solely decreases intraoperative bleeding that may obscure visualization but also minimizes the chance for catastrophic bleeding. All vessels greater than 2 mm which are encountered through the resection are clipped in a number of areas. The lingual artery or its dorsal lingual branch is typically encountered on the lateral side of the resection. When identified, multiple clips are placed alongside the uncovered portion of the artery. The danger with postoperative bleeding is the risk of aspiration and subsequent airway compromise quite than exsanguination. The patient is then delivered to the working room immediately to discover the wound and management the bleeding. Inadvertent harm to the enamel can occur from retractor manipulation throughout surgical procedure. Care is taken to place a tooth guard to shield the maxillary dentition previous to transoral publicity. In the occasion of chipped or avulsed tooth, the patient is referred for dental care. In the occasion of major postoperative hemorrhage, the entire following must be performed, besides a. Positioning the pivot level of the digicam arm at the level of the oral commissure d. Its axial airplane defines the superior boundary of the oropharynx, incompletely separating it from the nasopharynx above.
Buy discount artrichine 0.5mg on lineIn-office d�bridement and clearance of fabric from within the sinus cavity (usually performed on postoperative day 7 to 14) four. Typical drugs include antistaphylococcal antibiotics, oral prednisone, and a short course of analgesic medicines. In-office endoscopic surveillance for proof of ongoing irritation and/or restenosis as indicated Complications 1. Synechiae Postoperative initial follow-up typically helps limit the extent of synechiae formation. If it occurs and likewise becomes symptomatic, cicatricial scar can usually be resected in the office with through-cutting and powered instruments. If circumferential stenosis develops, this could sometimes be enlarged in office beneath native anesthesia with an elevator and mushroom punch. This procedure allows light widening of the ostium via the motion of balloon-based dilation of the sphenoid ostium. Sinuplasty has the advantage of efficiency beneath local anesthesia in the office as an initial procedure or also in the working room when combined with different sinonasal interventions. In-office/intraoperative picture guidance platforms can be found to verify entry and placement of the balloon tip inside the sinus airspace. This procedure could additionally be indicated in sufferers suffering from chronic sinusitis with out nasal polyps or recognized with recurrent acute sinusitis. In most patients with inflammatory disease of the sphenoid sinus, continued medical therapy is an alternative. Dissection inferiorly, by way of the posterior septal branch of sphenopalatine artery 3. Inadequate blunt dissection of the ostium, resulting in difficulty passing the Kerrison or mushroom punch into the ostium 4. Contact with the posterior wall of the sphenoid sinus throughout ostial identification or dissection might lead to inadvertent damage to the carotid artery or optic nerve. Endoscopic Sphenoidotomy 733 Olfactory fibers emanate from perforations in the cribriform plate and innervate the olfactory epithelium located within the olfactory area of the nasal cavity, which includes the superior parts of the nasal septum and the medial surfaces of the superior and middle turbinates. Twelve percent of sufferers in this cohort had complaints of olfactory loss after surgery, but none of the latter patients had olfactory neurons detectable on histology. Much continues to be unknown in regards to the results on olfaction of endoscopic sinus surgical procedure, including endoscopic sphenoidotomy. The posterior septum is disarticulated from the sphenoid rostrum with a Cottle instrument, and the rostral bone is removed with rongeurs or a drill to open each side of the sphenoid sinus. The anterior face of the sphenoid sinus can be safely punctured with a Frazier suction inferomedial to the sphenoid ostium where the bone is thinnest typically. In patients with persistent inflammatory illness and osteitis of the bone, circumferential stenosis of the sphenoidotomy is widespread postoperatively. A wide sphenoidotomy that extends to the floor of the sinus or crosses the podium and intersinus septum will assist forestall circumferential scarring and stenosis. Endoscopic view of proper sphenoid sinus after completion of endoscopic sphenoidotomy process. The clival recess (C) and the pituitary gland (P) could be readily observed alongside the posterior wall of this sinus cavity, and the impression of optic nerve (*) is seen within the superolateral nook of this sinus. Olfactory neuroepithelium in the superior and center turbinates: which is the optimum biopsy web site The forgotten turbinate: the function of the superior turbinate in endoscopic sinus surgery. Resection of the inferior superior turbinate: does it affect olfactory capability or include olfactory neuronal tissue What artery could also be encountered during inferior enlargement of the sphenoid ostium Second, trephination may be mixed with transnasal endoscopic approaches to the frontal sinus for severe inflammatory disease or challenging frontal recess anatomy, frequently referred to as a minitrephine. This article discusses the use of trephination to instill water (minitrephine) or of the trephine as a portal to assist within the performance or outcome of an endoscopic sinus process. Indications As endoscopic strategies have improved, so too has the flexibility of sinus surgeons to handle frontal sinus pathology endonasally. The utility of frontal sinus minitrephine, therefore, has become more and more limited. Frontal sinus trephination does, nonetheless, stay a useful tool as a stand-alone process, as an adjunct to frontal sinus endoscopy, and likewise as a combined endonasal and external approach for the next indications3,four: 1. Inflammatory frontal sinus pathology that meets criteria for endoscopic sinus surgical procedure after medical remedy has failed a. Altered nasofrontal anatomy (obstructing frontal cells, frontal recess scarring/stenosis and ossification) c. The affected person being considered for frontal sinus trephination is one who has failed medical remedy and is a candidate for endoscopic sinus surgery with a present frontal sinus part. History of facial trauma or exterior surgical procedure for the frontal sinus Contraindications 1. Frontal sinus trephination is contraindicated in the patient with a small shallow frontal sinus as a result of the chance of unintentional drilling via the posterior table. Nasal endoscopy to assess visualization of the outflow tract of the frontal sinus. This ought to include the presence of ipsilateral septal deviation and the dimensions and configuration of the center turbinate. Palpation of the forehead will give a basic indication of the bony prominence of the frontal sinus and its likely extent above the brow. Palpation of the supraorbital foramina and testing of sensory function Preoperative Preparation 1. Adjust the place of picture steering hardware if essential to present full entry to trephine landmarks. Positioning � Supine: the patient is positioned the same as any endoscopic sinus procedure with the pinnacle turned barely towards the surgeon. Drilling skills Perioperative Antibiotic Prophylaxis � First-generation cephalosporin to cowl skin organisms except a preoperative sinus culture suggests various coverage Operative Risks 1. Depression of the soft tissues into the trephine site if the trephine is massive enough to allow for a scope and instrumentation and never just for the instillation of fluids 4. Eye harm through irrigation into orbit from frontal bone dehiscence or corneal abrasion from working close to globe Monitoring � No routine monitoring required Instruments and Equipment to Have Available 1. Most powered instrument firms manufacture a kit for frontal sinus trephination. The sleeve has enamel to grip the periosteum of the frontal bone, permitting for preservation and cannulation of the drill gap by the surgeon. A fluted irrigation canula to permit for a good match of the grommet to the frontal bone 3. Fast-absorbing 6-0 suture for closure Surgical Technique Mini�frontal sinus trephination (see video 111.
Purchase artrichine overnightCarcinoma of the tongue base handled by transoral laser microsurgery, part one: untreated tumors, a potential analysis of oncologic and practical outcomes.
[newline]Transoral surgical anatomy and clinical concerns of lateral oropharyngeal wall, parapharyngeal space, and tongue base. Transoral laser microsurgery as main treatment for advanced-stage oropharyngeal most cancers: a United States multicenter examine. Adjuvant radiotherapy after transoral laser microsurgery for advanced squamous carcinoma of the top and neck. Transoral laser microsurgery � adjuvant therapy for superior stage oropharyngeal cancer: outcomes and prognostic components. Postoperative bleeding in transoral laser microsurgery for upper aerodigestive tract tumors. Transoral laser microsurgery for oropharyngeal squamous cell carcinoma: a paradigm shift in therapeutic method. Editorial Comment As the section editor would like to touch upon a quantity of of the numerous essential points and ideas offered on this chapter. While I fully agree with this remark throughout the collective spectrum of small to larger tongue base procedures, there are extra components to the lingual artery that come into play with bigger resections. This is a much larger diameter artery with important anterograde and retrograde blood circulate. Ideally this vessel would be identified and dissected proximally and distally with clip ligature previous to inadvertent transection. This vessel has anastomoses with the contralateral suprahyoid artery and might prove to be a major supply of postoperative bleed if it was not adequately controlled through the resection of the bottom of the tongue. What are the problems associated with extended retractor time and extra stress Reduced fee of infection due to reduced want for pharyngotomy Superior useful outcomes as a result of mucosal re-epithelization, maintained sensory and motor function, and reduced want for flap reconstruction 5. Endoscopic Laser Surgery of the Upper Aerodigestive Tract: With Special Emphasis on Cancer Surgery. Note: this surgical atlas is required for anyone critically contemplating incorporating transoral laser microsurgery into his or her head and neck apply. It is clearly written, well-illustrated, and reflects the wealth of experience gained by the true pioneers in the fields of transoral laser surgery for benign and malignant illness. Medical sickness: History of different head and neck cancers (which could be seen in more than 36% of patients who smoke),eight,9 historical past of lung most cancers, history of cervical most cancers,10 earlier surgery within the oropharynx 1) Any sicknesses that may be contraindications for surgical intervention including important cardiovascular, pulmonary, or different end-stage cancers 2) Hypercoagulable problems requiring persistent anticoagulation 3) Coagulopathy together with von Willebrand illness or other 4) Stents requiring antiplatelet remedy 5) Significant sleep apnea (to perceive postoperative danger of flash pulmonary edema and/or want for tracheostomy) 6) History of aspiration occasions 7) History of autoimmune disorders or transplantation requiring long-term antirejection remedy c. History of radiation to the top or neck space (including for Hodgkin, treatment of acne) d. Surgery 1) Previous tonsillectomy or sleep apnea surgery 2) Any neck surgical procedure 3) Arm and leg surgical procedure (in case the affected person may require free flap reconstruction). Family historical past 1) History of head and neck cancers 2) Autoimmune disorders 3) Cervical cancer in important different (Data from the Swedish Cancer Registry (1958�1996) confirmed that spouses of patients with cervical most cancers had a considerably elevated threat of growth of tongue or tonsil cancer. Medications 1) Antiplatelet drugs or anticoagulant drugs 2) Immunosuppressive medications 3) Herbal products (fish oil, valerian root) g. When diagnosed and treated in its early stages, 5-year survival charges can exceed 83%. Patient selection is of the utmost importance as a result of margin-negative resection is very predictive of overall survival in head and neck cancers. Knowledge of inside-out anatomy is essential to a protected and effective operation, particularly when approaching the oropharynx transorally. Halstedian ideas of oncologic surgical procedure have to be maintained when eradicating tumors, allowing for adequate margins and decreased tumor spillage. Ligating feeding vessels to the oropharynx in the course of the neck dissection can assist in prevention of postoperative hemorrhage. Many sufferers will present initially with a mass in the neck; in these instances, questions concerning onset, location, length, exacerbation, and any treatments could give insight into the underlying etiology of the mass (vascular, infectious, autoimmune, neoplastic). The affected person should be questioned relating to dysphagia, odynophagia, otalgia, weight loss, hemoptysis, hoarseness, dysgeusia, and dyspnea, as a outcome of these are most likely to be seen in sufferers with underlying malignancy. Note high quality of breathing-mouth breathing or stridor; indicators of obstruction, drooling or dry mouth b. Some patients could have a attribute foul odor of the breath, notably these with larger cancers. Examine lips, gums, enamel, ground of mouth, tongue, and visual oropharynx with two tongue blades. Bimanual palpation of lips, ground of mouth, tongue, base of the tongue, cheeks, and onerous palate c. Topical anesthetic and decongestant may additionally be utilized presently in preparation for nasal endoscopy. Palpation of the lymph node basins of the neck from degree Ia to level V 1) Any lymph nodes must be assessed for fixation, mobility in sure directions b. It also can present info concerning involvement of vessels or local buildings. Mobility of the tumor, involvement of adjacent buildings, and exposure are all evaluated on the time of this endoscopy. This also provides the surgeon an idea of how properly the cancer can be uncovered, particularly if transoral resection is being deliberate or if the patient would require intensive reconstruction (in which case, a mandible cut up or a robotic strategy may be necessary). Relaxation is of the utmost efficiency during transoral surgery as a outcome of this aids in visualization, dissection, and in reducing the risk of the affected person transferring during surgery. Patients with primary T1, T2, T3, and select T4 lesions of the oropharynx with possible reconstruction 2. Patients with recurrent cancer of the oropharynx; to be carried out at the aspect of a reconstructive surgeon three. Metastatic most cancers to the neck from an unknown primary as part of the analysis and therapy Positioning Supine: the affected person is positioned supine, without a shoulder bump. Additionally, if the surgical robotic shall be used, this permits maximization of the robotic digital camera and instrument mobility. Medical comorbidities with elevated risk for general anesthesia: End-stage cardiac disease (Preoperative risk assessment by a cardiologist is necessary. Relative contraindication: Pterygoid involvement (will require in depth reconstruction as a part of planning) Perioperative Antibiotic Prophylaxis First-generation cephalosporin and metronidazole: Due to the standard flora of the oral cavity, twin coverage with a cephalosporin and metronidazole are warranted. Clindamycin: Can be used in its place in patients with penicillin allergy as a end result of it covers nearly all of oral flora. The caveat with this treatment is its association with Clostridium difficile as a complication. Monitoring Monitoring for continued neuromuscular paralysis Preoperative Preparation Procedures 1. Two Bovie pads (one for normal monopolar cautery and one for suction cautery) 4. Optional: Can use a 30-degree endoscope to evaluate the base of the tongue if not well visualized transorally. Three chairs which have a foot pedal for adjusting up and down, two on the bedside (for the nurse and the bedside surgical assistant) and one at the surgeon console 22. Recommended 5-mm EndoWrist Instrumentation: 1) Monopolar cautery 2) Maryland forceps an anterior digastric flap to bolster this space. Injury to the carotid artery: Rare but possible if the surgeon dissects too far laterally.
References - Keating NL, OiMalley AJ, Freedland SJ, et al: Diabetes and cardiovascular disease during androgen deprivation therapy: observational study of veterans with prostate cancer, J Natl Cancer Inst 102(1):39n46, 2010.
- Hahn AF: The challenge of respiratory dysfunction in Guillain- Barre syndrome. Arch Neurol 58(6):871n872, 2001
- Wiart L, Joseph PA, Petit H, et al: The effects of capsaicin on the neurogenic hyperreflexic detrusor. A double blind placebo controlled study in patients with spinal cord disease. Preliminary results, Spinal Cord 36(2):95n99, 1998.
- Marchiole P, Benchaib M, Buenerd A, et al: Oncological safety of laparoscopicassisted vaginal radical trachelectomy (LARVT or Dargentis operation): a comparative study with laparoscopic-assisted vaginal radical hysterectomy (LARVH), Gynecol Oncol 106(1):132n141, 2007.
|
|